How Do Pulmonary Artery Models Replicate Embolism Scenarios?
Anatomical Accuracy and Pathological Variations
Pulmonary artery models are meticulously crafted to mirror the intricate vascular anatomy of the human body. These models incorporate detailed representations of the pulmonary trunk, right and left pulmonary arteries, and their subsequent branches. The anatomical accuracy extends to the inclusion of key landmarks and surrounding structures, providing a comprehensive view of the pulmonary vasculature.
To replicate embolism scenarios, these models are designed with customizable pathological variations. Manufacturers can incorporate simulated clots or obstructions at various locations within the pulmonary arterial tree. These artificial emboli can be strategically placed to mimic different clinical presentations, from massive central embolisms to peripheral subsegmental occlusions. The ability to recreate diverse pathological states allows medical professionals to encounter and manage a wide spectrum of embolism scenarios during their training.
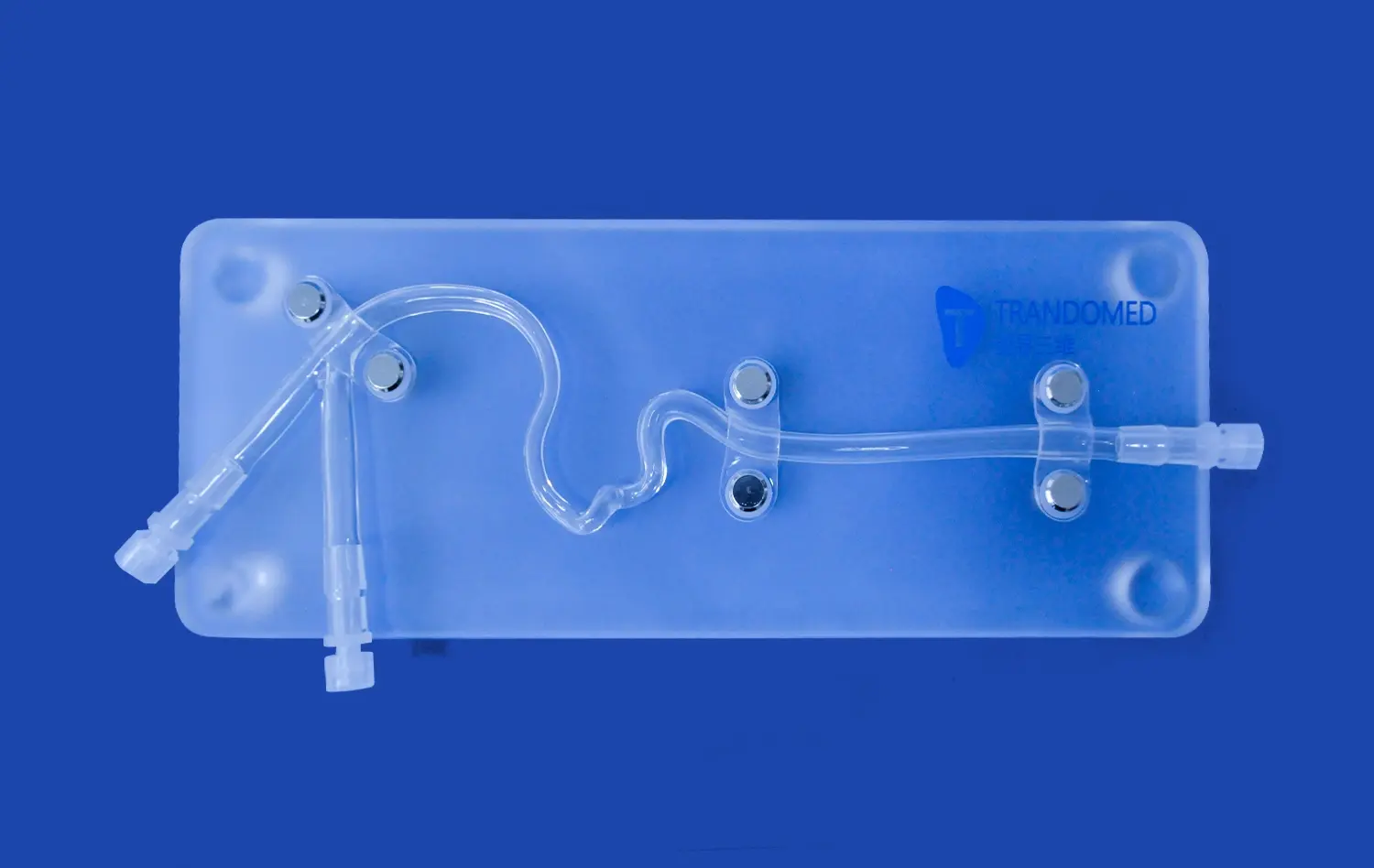
Material Properties and Vessel Wall Characteristics
The choice of materials used in pulmonary artery models plays a crucial role in replicating the physical properties of blood vessels. Advanced silicone formulations, such as those with a Shore 40A hardness, provide a realistic feel and response to interventional devices. These materials can be engineered to mimic the elasticity and compliance of actual pulmonary arteries, allowing for authentic tactile feedback during simulated procedures.
Vessel wall characteristics are carefully reproduced in these models. The three-layered structure of arteries - the tunica intima, media, and adventitia - can be simulated to provide accurate resistance and behavior during catheter navigation and device deployment. This attention to detail ensures that trainees experience realistic challenges when maneuvering through the pulmonary vasculature, closely mimicking the sensations encountered in live patients.
Modular Design for Diverse Training Scenarios
Modern pulmonary artery models often feature modular designs that enhance their versatility in replicating various embolism scenarios. For instance, the ability to detach and replace sections of the model, such as the superior vena cava and right heart chambers, allows for the simulation of different access routes and anatomical variations. This modularity enables educators to present trainees with a diverse range of clinical challenges, from straightforward cases to complex anatomical anomalies.
The modular approach also facilitates the integration of specialized training modules. For example, educators can incorporate segments with varying degrees of vessel tortuosity or introduce rare congenital malformations. This flexibility in design allows for the creation of tailored training experiences that address specific learning objectives or focus on particularly challenging aspects of pulmonary embolism management.
Realistic Clot Placement and Flow Simulation Techniques
Advanced Clot Modeling Methodologies
The realism of pulmonary artery models in embolism training hinges on the accurate representation of blood clots. Advanced clot modeling methodologies have been developed to create artificial thrombi that closely resemble their biological counterparts in terms of size, shape, and consistency. These simulated clots are often crafted using materials that mimic the density and mechanical properties of actual blood clots, allowing for realistic interactions with interventional devices.
Clot placement within the model is a precise process, guided by clinical data and expert input. Manufacturers can position these artificial emboli at various locations, from large central arteries to distal subsegmental branches. The ability to customize clot size and distribution enables the simulation of different embolism severities, from small peripheral occlusions to life-threatening saddle emboli. This level of customization allows trainers to present a wide range of clinical scenarios, preparing medical professionals for diverse real-world situations.
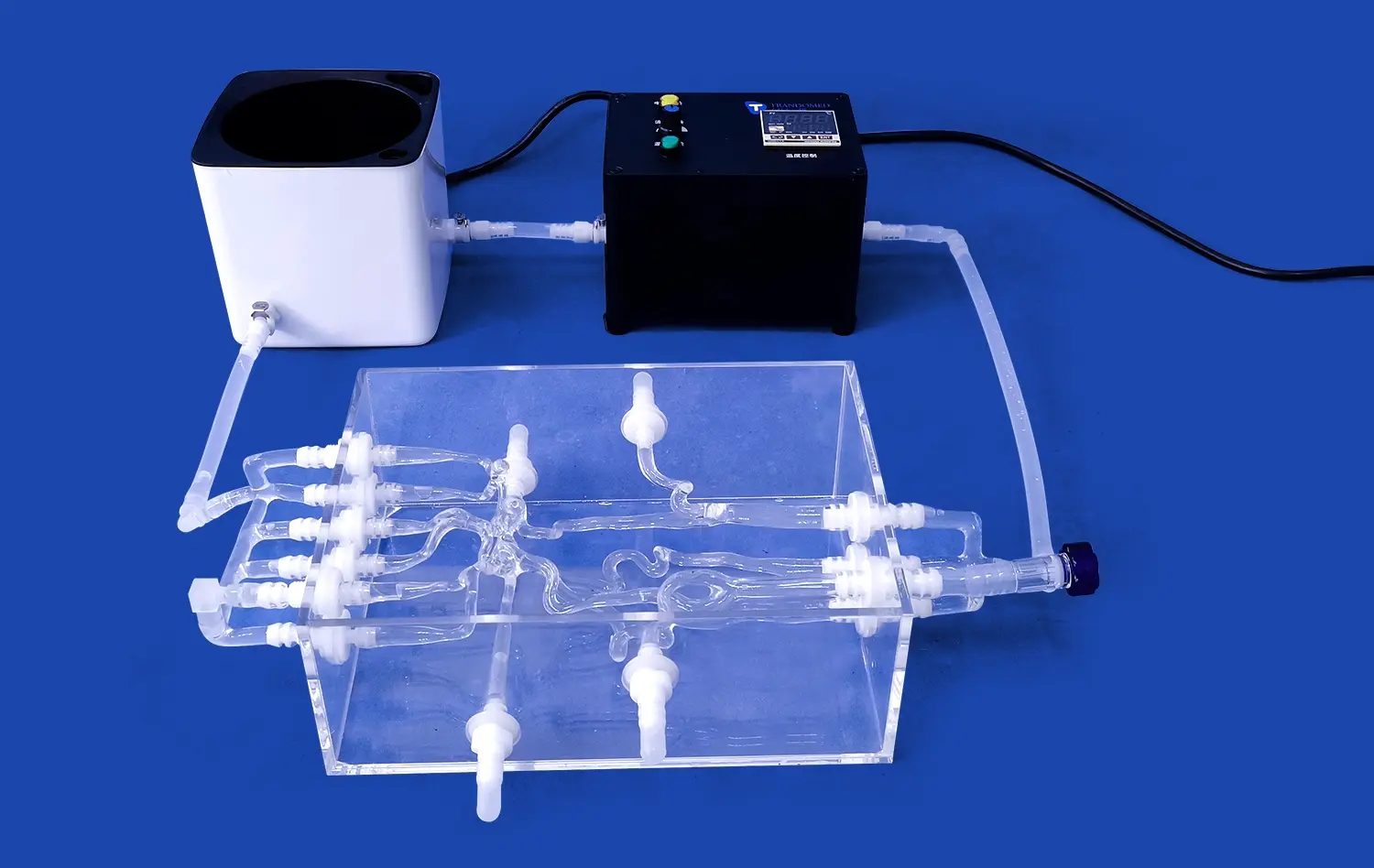
Dynamic Flow Simulation Systems
To enhance the fidelity of embolism scenarios, pulmonary artery models are often integrated with dynamic flow simulation systems. These systems use specialized pumps and fluid reservoirs to replicate physiological blood flow patterns within the pulmonary circulation. By adjusting flow rates and pressures, trainers can simulate various hemodynamic states associated with pulmonary embolism, from mild flow disturbances to severe circulatory compromise.
Advanced flow simulation techniques may incorporate pulsatile flow generators to mimic cardiac output and respiratory variations. This dynamic element adds a layer of complexity to the training experience, requiring trainees to adapt their techniques to changing flow conditions. Some systems even allow for the real-time adjustment of hemodynamic parameters, enabling instructors to simulate the progression of an embolism or the effects of therapeutic interventions on pulmonary blood flow.
Integration of Imaging Modalities
Modern pulmonary artery models are designed to be compatible with various imaging modalities commonly used in the diagnosis and management of pulmonary embolism. These models can be constructed using materials that are radiopaque or echogenic, allowing for realistic visualization under fluoroscopy, CT angiography, or ultrasound. This integration of imaging capabilities enhances the training experience by allowing practitioners to correlate anatomical landmarks with their corresponding imaging appearances.
Some advanced training setups incorporate virtual reality or augmented reality systems that overlay simulated imaging data onto the physical model. This fusion of physical and digital elements creates a highly immersive training environment, allowing trainees to practice interpreting imaging studies in conjunction with hands-on interventional techniques. The ability to seamlessly integrate multiple imaging modalities into the training process helps bridge the gap between theoretical knowledge and practical application in pulmonary embolism management.
Integrating Models into Advanced Pulmonary Embolism Training Programs
Curriculum Development and Skill Progression
The integration of pulmonary artery models into advanced training programs requires thoughtful curriculum development. Educators typically structure these programs to ensure a logical progression of skills, starting with basic anatomy recognition and catheter navigation techniques before advancing to more complex scenarios. The curriculum may be designed to cover a range of competencies, including clot identification, risk stratification, and selection of appropriate interventional strategies.
Training modules are often tailored to different levels of expertise, accommodating everyone from medical students to experienced interventionalists seeking to refine their skills. As trainees progress, they encounter increasingly challenging scenarios that test their decision-making abilities under pressure. This staged approach allows for the gradual build-up of confidence and competence in managing pulmonary embolism cases of varying complexity.
Simulation-Based Team Training
Pulmonary artery models serve as a focal point for simulation-based team training exercises. These sessions bring together multidisciplinary teams, including interventional radiologists, pulmonologists, emergency physicians, and nursing staff, to practice coordinated responses to pulmonary embolism scenarios. The models provide a tangible, shared reference point around which team members can communicate and collaborate.
During these simulations, teams are challenged with realistic case scenarios that require rapid assessment, decision-making, and execution of interventional procedures. The use of high-fidelity models allows for the practice of critical steps in embolism management, from initial diagnosis to catheter-directed thrombolysis or mechanical thrombectomy. This team-based approach enhances not only individual skills but also improves overall team performance and communication in high-stress situations.
Performance Assessment and Feedback Mechanisms
Advanced pulmonary embolism training programs incorporate robust performance assessment and feedback mechanisms. Objective metrics, such as procedure time, accuracy of clot localization, and success rates of simulated interventions, can be tracked and analyzed. Some training systems are equipped with sensors or tracking devices that provide quantitative data on catheter movements and device deployments, offering detailed insights into trainee performance.
Feedback is often delivered through a combination of automated system reports and expert instructor evaluations. Post-simulation debriefing sessions allow trainees to reflect on their performance, discuss challenges encountered, and receive personalized guidance on areas for improvement. This comprehensive feedback approach ensures that learners can identify and address specific skill gaps, leading to continuous improvement in their ability to manage pulmonary embolism cases effectively.
Conclusion
The integration of advanced pulmonary artery models into medical training programs represents a significant leap forward in preparing healthcare professionals to manage pulmonary embolism effectively. These anatomically accurate and pathologically diverse models provide a safe, repeatable environment for honing critical skills. By combining realistic clot simulations, dynamic flow systems, and cutting-edge imaging capabilities, these training platforms offer an unparalleled learning experience. As medical education continues to evolve, the role of high-fidelity simulation in pulmonary embolism training will undoubtedly expand, contributing to improved patient outcomes and advancing the field of vascular intervention.
Contact Us
Elevate your pulmonary embolism training program with Trandomed's state-of-the-art pulmonary artery models. Our customizable, anatomically precise simulators offer unparalleled realism for advanced medical education. Experience the benefits of hands-on training without patient risk. For more information on how our innovative solutions can transform your educational initiatives, contact us at jackson.chen@trandomed.com.
_1734507815464.webp)
_1732866687283.webp)
_1732843184544.webp)