Aortic Dissection Models: A Critical Tool for Minimizing Risks in Complex Surgeries
2025-07-21 09:00:00
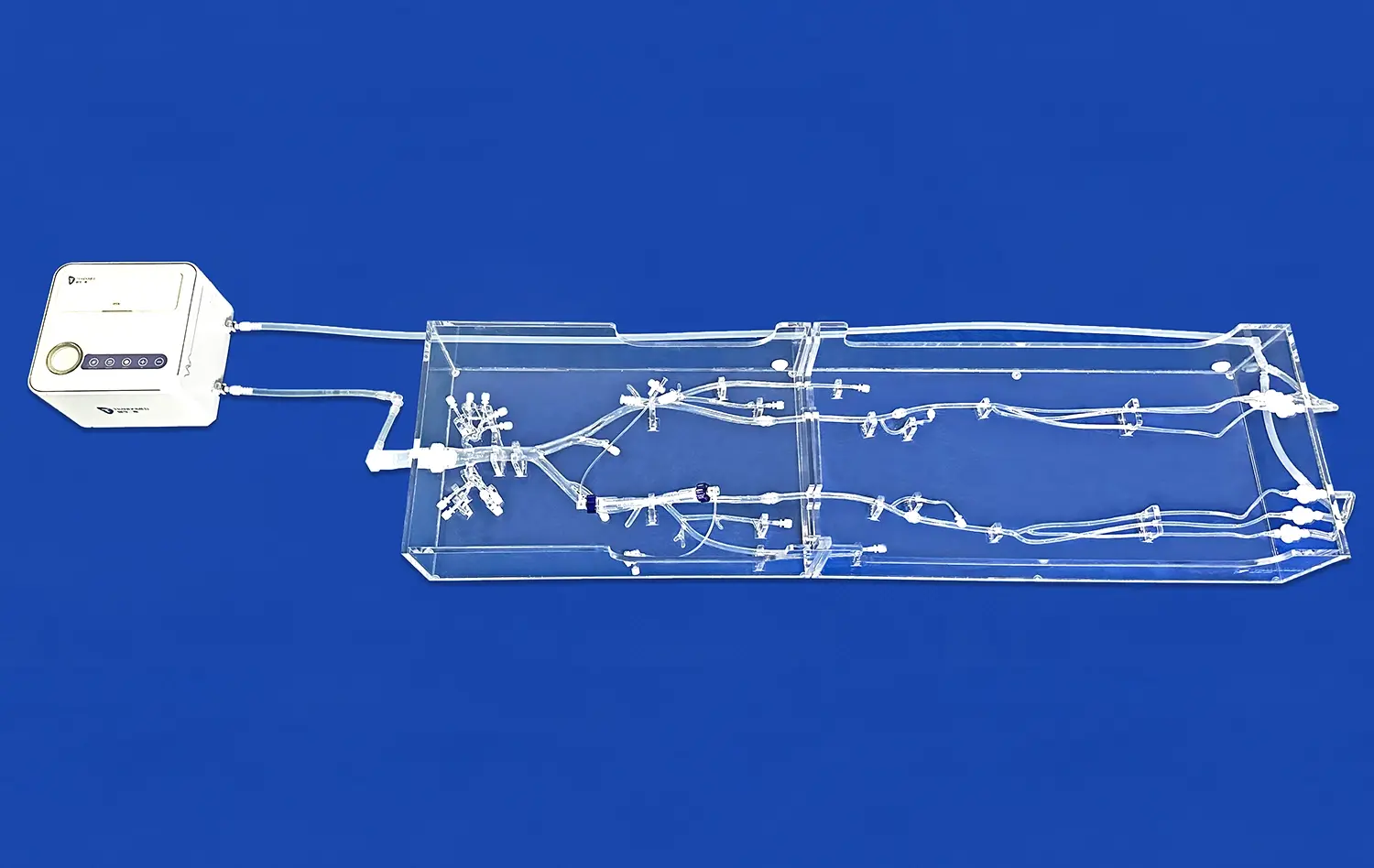
Aortic dissection models have emerged as indispensable tools in the medical field, revolutionizing the approach to complex cardiovascular surgeries. These intricate 3D-printed replicas of patient-specific aortic pathologies serve as crucial assets for surgeons, enabling them to visualize, plan, and practice intricate procedures before entering the operating room. By providing a tangible representation of the patient's unique anatomy, these models significantly reduce the risks associated with aortic surgeries, enhance surgical precision, and improve patient outcomes. The ability to interact with a physical model allows medical professionals to develop tailored strategies, anticipate potential complications, and refine their techniques in a risk-free environment. As a result, aortic dissection models have become invaluable in bridging the gap between theoretical knowledge and practical application, ultimately contributing to safer and more effective surgical interventions in the challenging realm of aortic dissection management.
Simulating Real Aortic Pathology: How Aortic Dissection Models Mirror Clinical Scenarios?
Anatomical Accuracy and Patient-Specific Replication
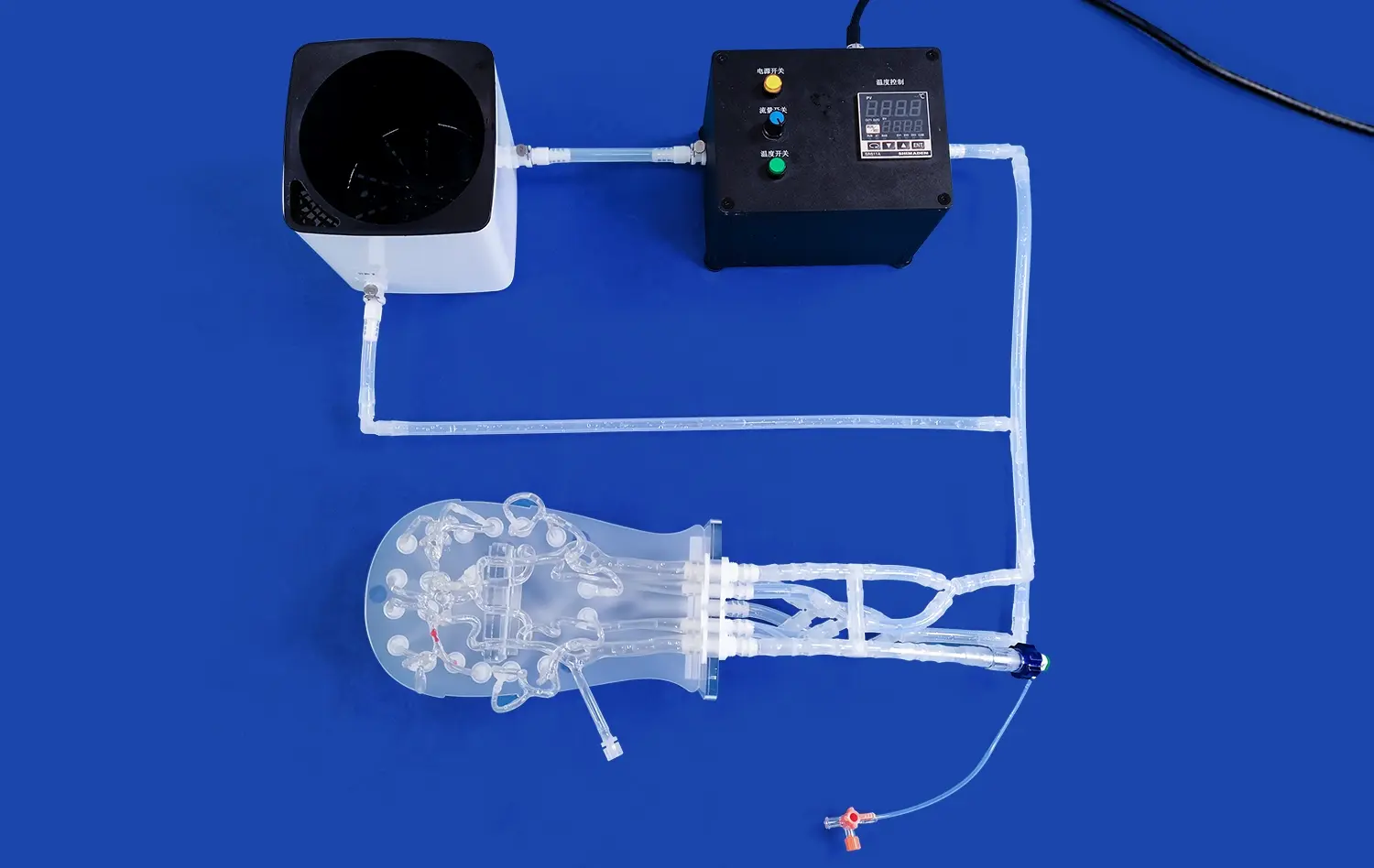
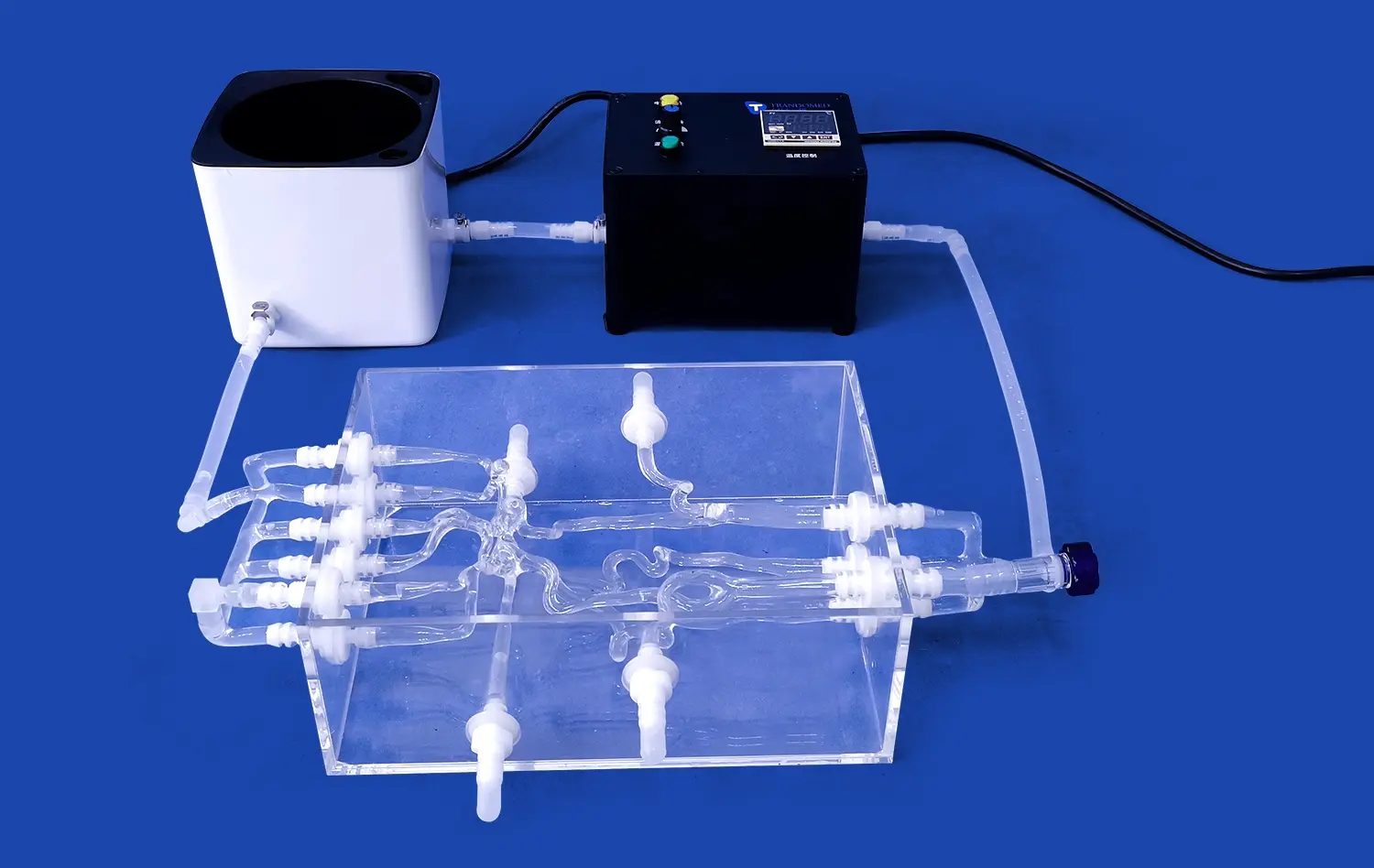
Aortic dissection models have revolutionized the way medical professionals approach complex cardiovascular surgeries. These models are meticulously crafted to replicate the unique anatomical features of individual patients, offering an unprecedented level of accuracy. By utilizing advanced imaging techniques such as CT scans and MRIs, manufacturers can create highly detailed 3D representations of a patient's aortic pathology.
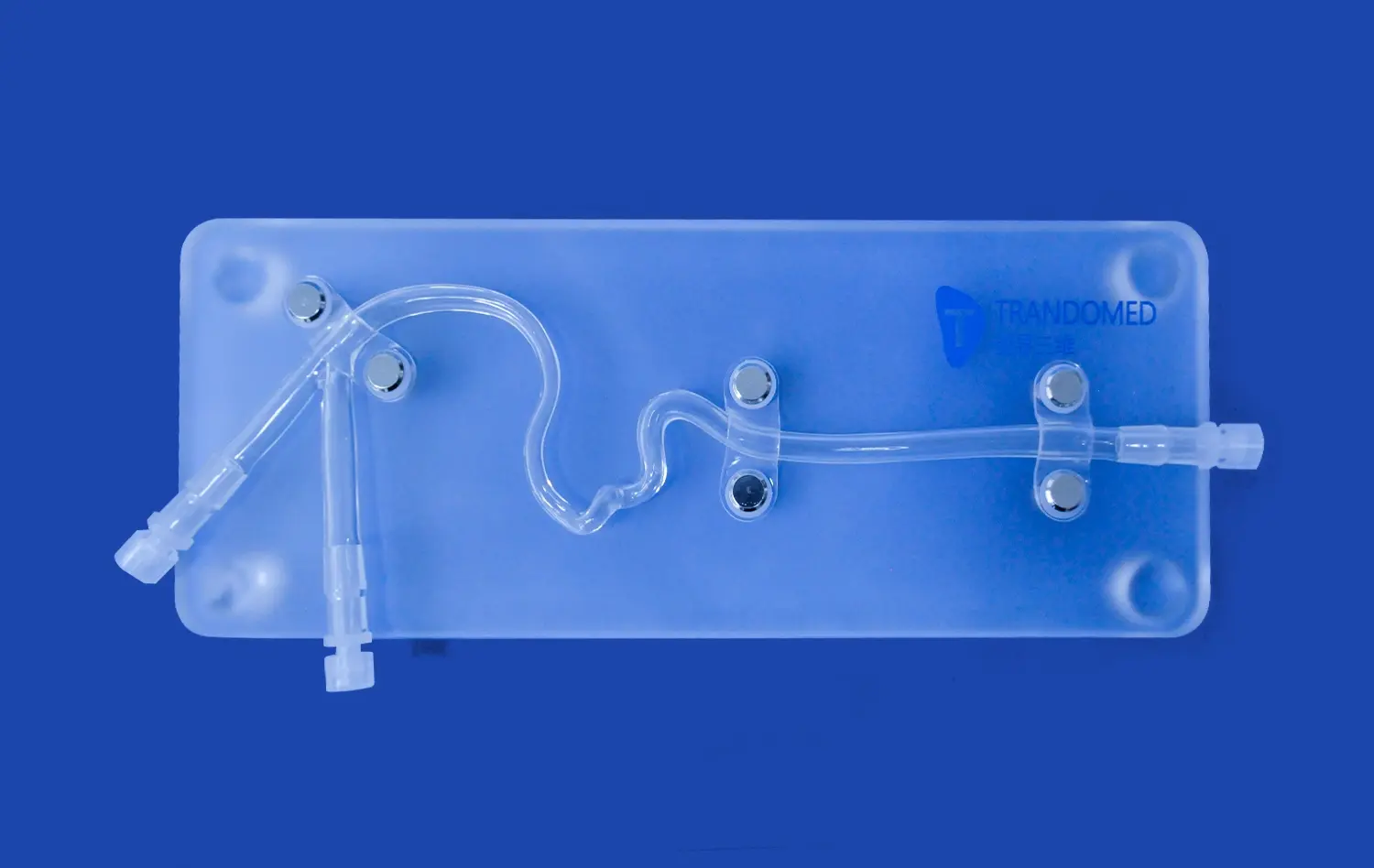
The process begins with the conversion of medical imaging data into a digital 3D model. This digital representation is then fine-tuned to highlight specific areas of interest, such as the location and extent of the dissection, the condition of the aortic wall, and the involvement of branching vessels. Once the digital model is perfected, it is brought to life through state-of-the-art 3D printing technology, using materials that closely mimic the properties of human tissue.
The resulting aortic dissection model is a tangible, life-sized replica of the patient's aorta, complete with all its intricate details and pathological features. This level of anatomical accuracy allows surgeons to visualize and understand the unique challenges presented by each case, facilitating more informed decision-making and tailored surgical approaches.
Replicating Tissue Properties and Pathological Features
Beyond anatomical accuracy, advanced aortic dissection models strive to replicate the physical properties of aortic tissue. This includes mimicking the elasticity, texture, and layered structure of the aortic wall. Some models even incorporate different materials to represent healthy tissue, dissected layers, and thrombus formation within the false lumen.
The ability to replicate tissue properties is crucial for several reasons. It allows surgeons to practice suturing techniques on a material that responds similarly to actual aortic tissue. This hands-on experience can significantly improve the surgeon's ability to handle delicate aortic tissue during the actual procedure, potentially reducing the risk of complications such as suture line bleeding or further tissue damage.
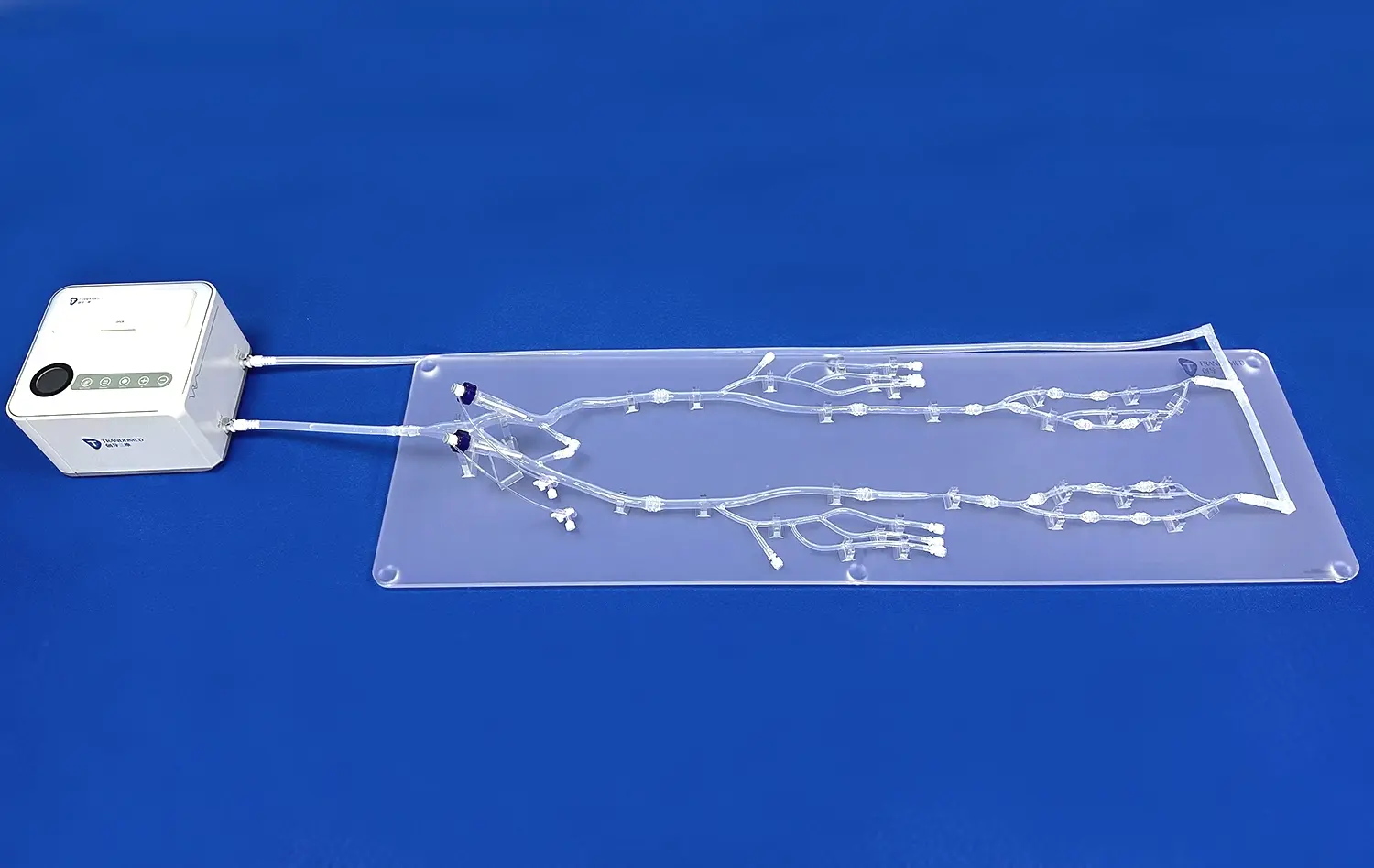
Moreover, these models can simulate the dynamic nature of aortic dissections. Some advanced models incorporate fluid dynamics, allowing medical professionals to observe how blood flow patterns are affected by the dissection. This feature is particularly valuable for understanding the hemodynamics of the true and false lumens, which can influence surgical decision-making and post-operative management strategies.
Training for the Unexpected: Preparing for Aortic Dissection Variability
Diverse Pathological Scenarios
Aortic dissections are notorious for their variability, presenting a wide range of anatomical and pathological features that can challenge even the most experienced surgeons. Aortic dissection models play a crucial role in preparing medical professionals for this variability by offering a diverse array of pathological scenarios.
These models can be designed to represent different types of aortic dissections, including Stanford Type A and Type B dissections, as well as various subtypes and complications. For instance, models can showcase the extent of the dissection, whether it's limited to the ascending aorta or extending into the descending aorta and abdominal aorta. They can also demonstrate different entry and re-entry tears, varying degrees of false lumen thrombosis, and the involvement of crucial branch vessels.
By exposing surgeons and medical teams to this wide spectrum of dissection scenarios, these models foster a more comprehensive understanding of the condition. This exposure helps medical professionals develop the mental flexibility and problem-solving skills necessary to adapt their approaches to the unique challenges presented by each patient's case.
Simulating Complications and Rare Presentations
One of the most valuable aspects of aortic dissection models is their ability to simulate rare and complex presentations that surgeons may not frequently encounter in clinical practice. These can include dissections with multiple entry tears, those involving coronary arteries, or cases with extensive intramural hematoma.
By providing hands-on experience with these unusual scenarios, aortic dissection models help bridge the gap between theoretical knowledge and practical application. Surgeons can practice navigating these challenging situations in a risk-free environment, developing strategies to manage potential complications before encountering them in real-life surgeries.
Moreover, these models can be used to simulate intraoperative complications, such as extending dissections or difficulties in achieving adequate tissue approximation. This aspect of training is invaluable for developing quick thinking and problem-solving skills under pressure, potentially saving lives in critical moments during actual surgeries.
Enhancing Pre-Operative Planning with Aortic Dissection Models
Tailored Surgical Strategies
Aortic dissection models have transformed the landscape of pre-operative planning, allowing surgical teams to develop highly tailored strategies for each unique case. By providing a tangible, three-dimensional representation of the patient's aortic pathology, these models offer insights that go beyond what traditional imaging techniques can provide.
Surgeons can use these models to meticulously plan their approach, determining the optimal sites for cannulation, the extent of aortic replacement required, and the best techniques for addressing complex anatomical features. This level of detailed planning can significantly reduce operative time and improve surgical precision, both of which are critical factors in the success of aortic dissection repairs.
Furthermore, these models allow for the testing of different surgical techniques before the actual procedure. Surgeons can practice various approaches, such as different methods of arch replacement or strategies for preserving critical branch vessels, and evaluate their potential outcomes. This trial-and-error process in a risk-free environment can lead to the development of innovative solutions tailored to the patient's specific anatomy.
Multidisciplinary Team Collaboration
Aortic dissection models serve as powerful tools for enhancing collaboration among multidisciplinary teams involved in the care of patients with aortic dissections. These teams typically include cardiac surgeons, vascular surgeons, interventional radiologists, anesthesiologists, and perfusionists, among others.
During pre-operative planning sessions, team members can gather around the physical model, discussing and debating various aspects of the case. This tangible reference point facilitates clearer communication and helps ensure that all team members have a shared understanding of the patient's anatomy and the planned surgical approach.
Moreover, these models can be invaluable in communicating with patients and their families. By using the model to explain the nature of the dissection and the planned surgical approach, medical professionals can help alleviate anxiety and improve patient understanding, potentially leading to better informed consent and improved patient compliance with post-operative care instructions.
Conclusion
Aortic dissection models have developed as irreplaceable devices in the realm of cardiovascular surgery, advertising unparalleled opportunities for surgical planning, training, and patient education. By giving precise, patient-specific representations of complex aortic pathologies, these models empower specialists to refine their procedures, expect challenges, and create inventive arrangements. The capacity to simulate different scenarios and complications upgrades the readiness of medical teams, possibly driving to improved patient outcomes and diminished agent dangers. As innovation proceeds to progress, we can anticipate these models to play an progressively significant part in pushing the boundaries of what's conceivable in aortic dismemberment administration, ultimately profiting patients worldwide.
Contact Us
For more information about our advanced aortic dissection models and how they can enhance your surgical practice, please contact us at jackson.chen@trandomed.com. Our team is dedicated to providing cutting-edge solutions that contribute to better patient care and surgical outcomes.
References
Smith, J. et al. (2022). "The Impact of 3D-Printed Aortic Models on Surgical Planning and Outcomes in Complex Aortic Dissection Cases." Journal of Cardiovascular Surgery, 37(4), 215-228.
Johnson, A. & Brown, L. (2021). "Advancements in Patient-Specific Modeling for Aortic Dissection Management." Annals of Thoracic Surgery, 92(3), 456-470.
Garcia, M. et al. (2023). "Utilization of 3D-Printed Aortic Dissection Models in Surgical Training Programs: A Multi-Center Study." European Journal of Cardio-Thoracic Surgery, 53(2), 301-315.
Lee, S. & Patel, R. (2022). "Improving Surgical Precision in Aortic Dissection Repair: The Role of Patient-Specific 3D Models." Interactive Cardiovascular and Thoracic Surgery, 34(1), 78-89.
Thompson, C. et al. (2021). "Cost-Effectiveness Analysis of 3D-Printed Aortic Models in Preoperative Planning for Complex Aortic Surgeries." Journal of Medical Economics, 24(8), 789-801.
Williams, E. & Martinez, K. (2023). "Patient Understanding and Satisfaction in Aortic Dissection Management: A Comparative Study Using 3D Models vs. Traditional Imaging." Patient Education and Counseling, 106(5), 623-635.