How does the Model Assist in RF Ablation Pathway Training?
Anatomical Accuracy and Tactile Feedback
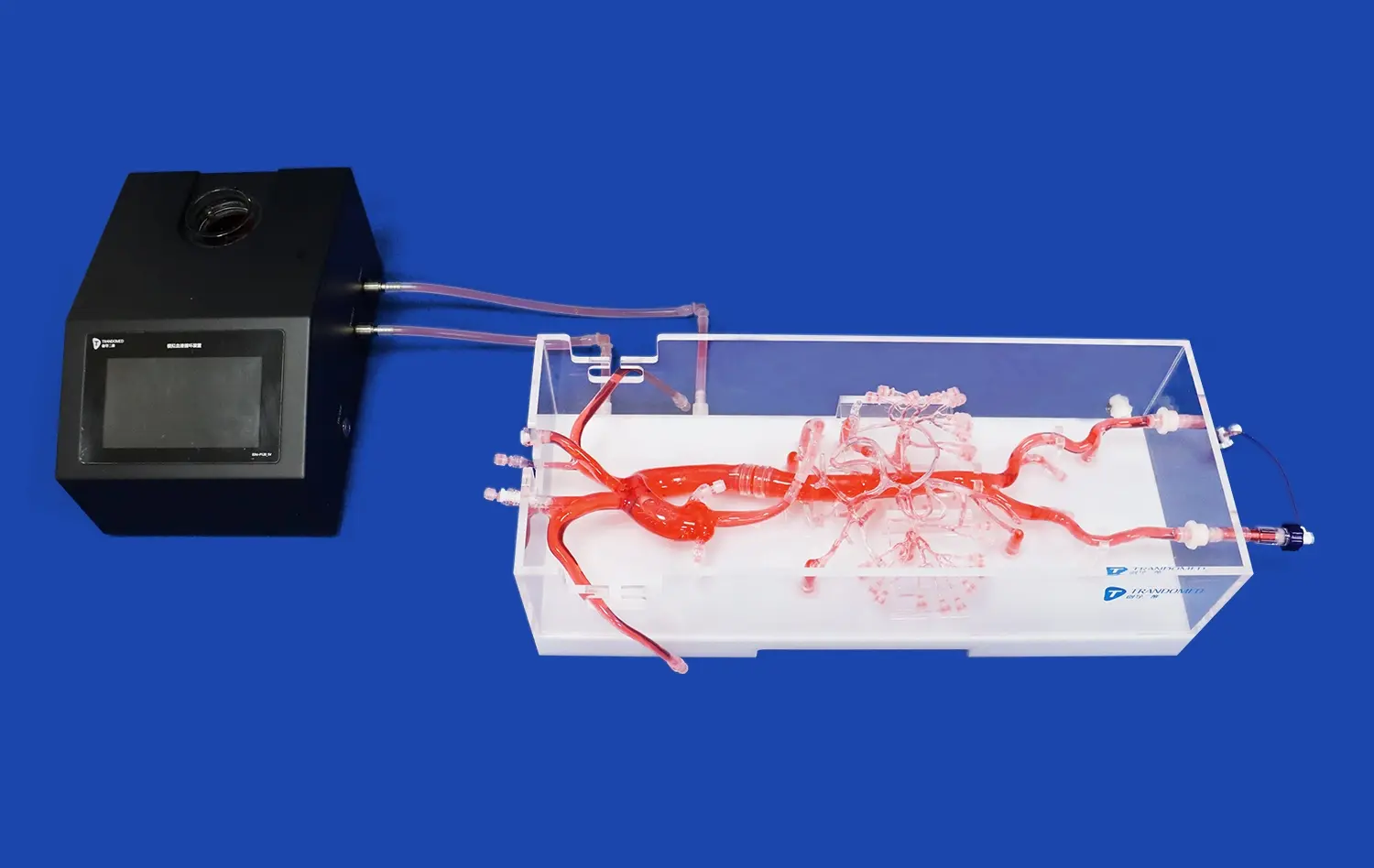
The atrial septal puncture model excels in providing an anatomically accurate representation of the heart's structures. Crafted from high-quality silicone with a Shore hardness of 40A, the model mimics the texture and resistance of actual cardiac tissue. This fidelity allows trainees to experience realistic tactile feedback when navigating catheters and performing punctures, closely simulating the sensations encountered during live procedures. The model's precise replication of the femoral vein, iliac vein, superior and inferior vena cava, left and right atria, and pulmonary veins ensures that practitioners can develop a comprehensive understanding of the cardiac anatomy relevant to RF ablation pathways.
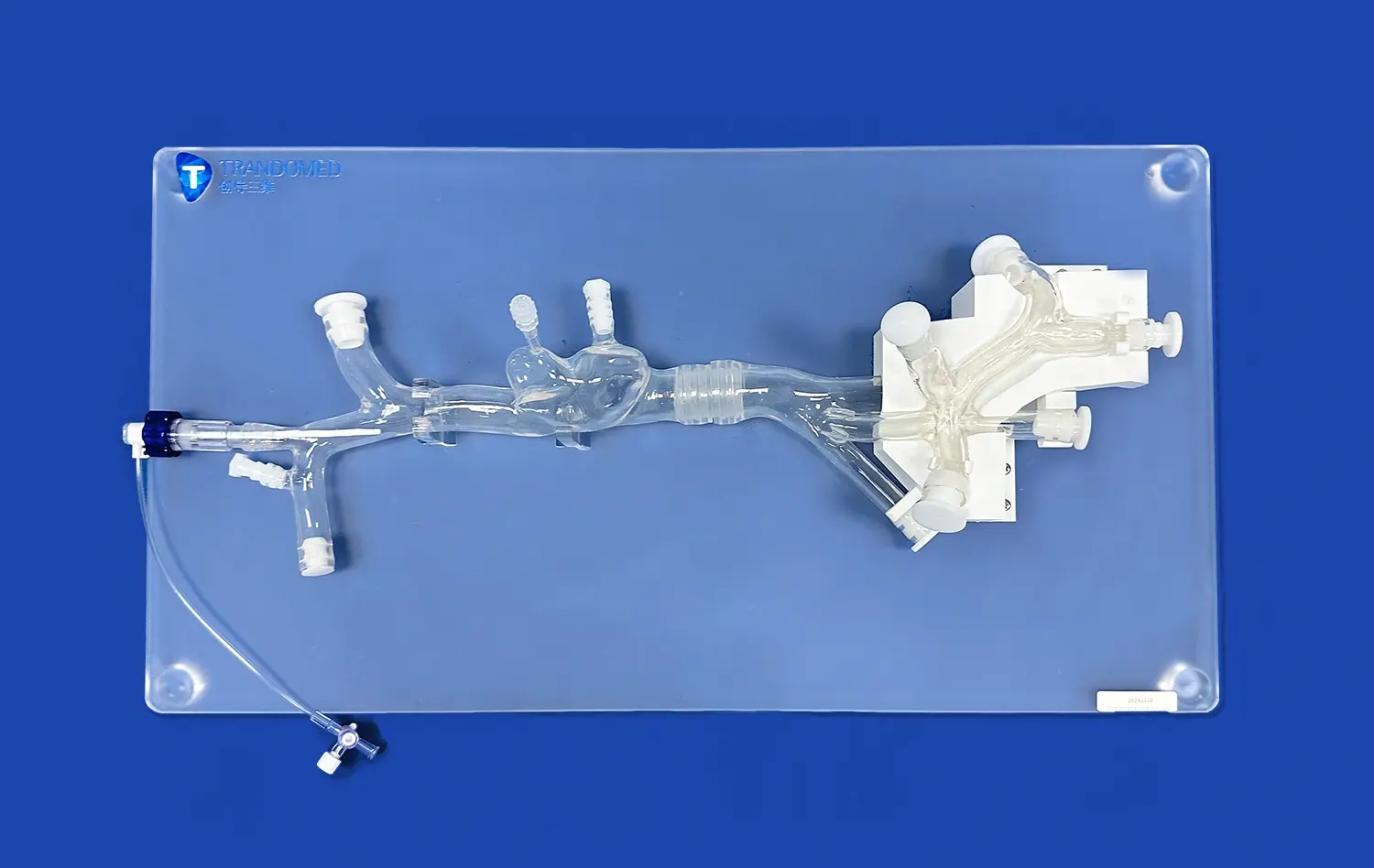
Modular Design for Versatile Training Scenarios
The modular design of the atrial septal puncture model enhances its versatility in training scenarios. With detachable upper (SVC with heart) and lower (IVC) parts, instructors can create various anatomical configurations to challenge trainees at different skill levels. This feature allows for the simulation of diverse patient anatomies, preparing practitioners for the wide range of scenarios they may encounter in clinical practice. Additionally, the interchangeable atrial septal inserts, including normal atrial septum and atrial septal defect (ASD) variants, provide opportunities to practice different puncture techniques and decision-making processes based on specific anatomical conditions.
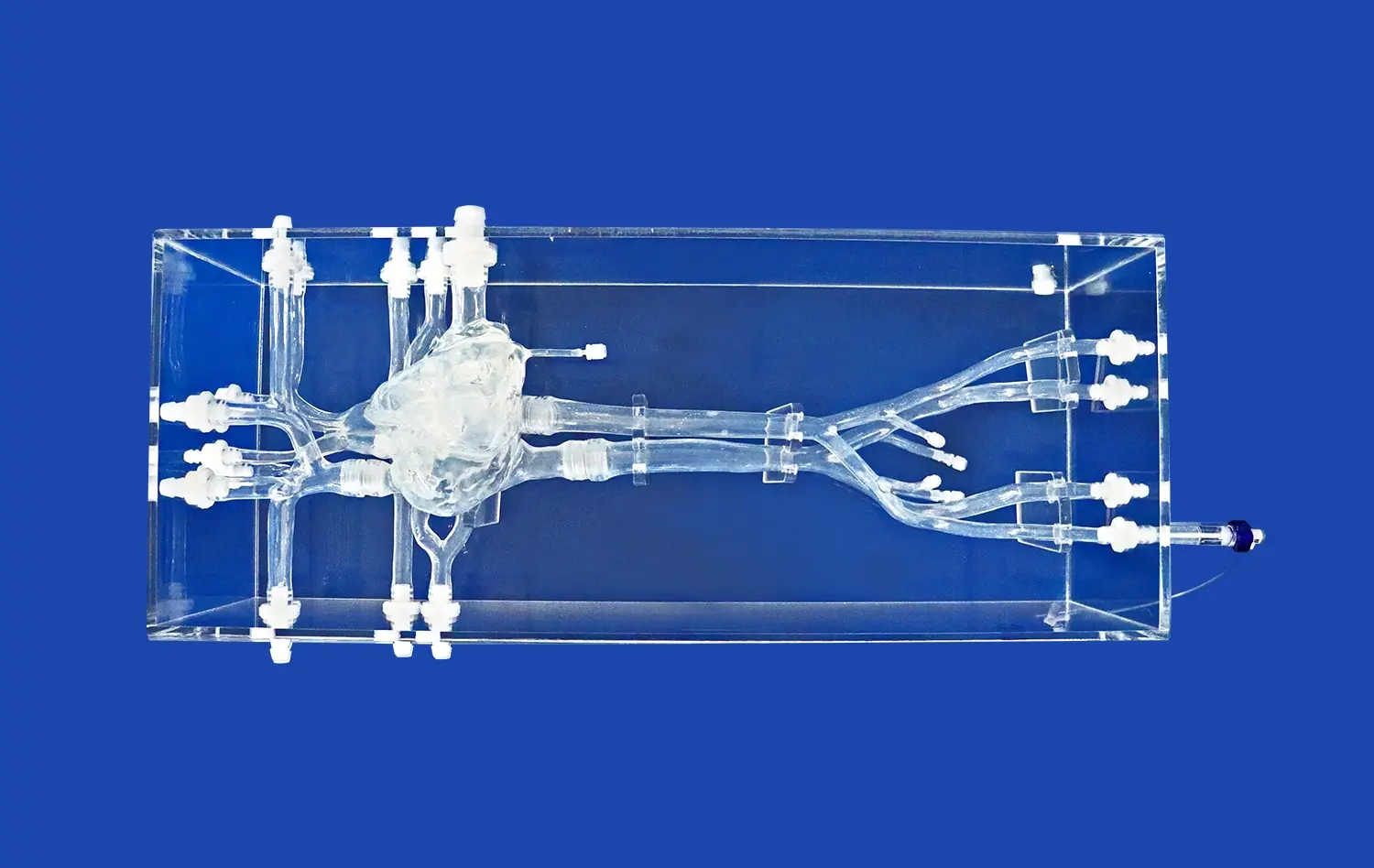
Visualization of Catheter Navigation
Transparency is a key feature of many atrial septal puncture models, allowing for clear visualization of catheter movement within the simulated cardiac structures. This visibility is invaluable for both trainees and instructors, as it facilitates real-time observation of catheter navigation, positioning, and manipulation during simulated RF ablation procedures. The ability to see the catheter's path through the venous system and into the heart chambers helps in understanding the three-dimensional relationships between anatomical structures and improves spatial awareness, which is crucial for successful RF ablation pathway training.
Simulation of Venous System Access Techniques
Femoral Vein Access Practice
The atrial septal puncture model provides a realistic platform for practicing femoral vein access, a critical first step in many cardiac catheterization procedures, including RF ablation. The model's accurate representation of the femoral and iliac veins allows trainees to develop proficiency in needle insertion, guidewire advancement, and sheath placement techniques. This hands-on experience helps build confidence and muscle memory for performing these essential access procedures, reducing the risk of vascular complications in actual patients.
Navigation Through Complex Venous Anatomy
Navigating the complex venous anatomy is a crucial skill for successful RF ablation procedures. The model's detailed replication of the venous system, from the femoral vein to the pulmonary veins, challenges practitioners to maneuver catheters through realistic anatomical structures. This simulation helps develop the dexterity and spatial awareness required to navigate tortuous vessels and overcome potential obstacles, such as venous valves or anatomical variations. By repeatedly practicing these navigation techniques, healthcare providers can improve their efficiency and reduce procedure times in clinical settings.
Transseptal Puncture Technique Refinement
The atrial septal puncture model excels in providing a platform for refining transseptal puncture techniques. The interchangeable atrial septal inserts allow for practice on both normal and defective septa, offering varied levels of difficulty. Trainees can perfect their ability to locate the fossa ovalis, apply appropriate pressure for tenting, and perform controlled punctures. This targeted practice helps in developing the precise motor skills and judgment necessary for safe and effective transseptal access, a critical step in many left atrial procedures, including RF ablation of atrial fibrillation.
Enhancing Consistency in Lesion Formation Practices
Catheter Contact Force Optimization
Achieving optimal catheter contact force is crucial for effective lesion formation during RF ablation procedures. The atrial septal puncture model allows practitioners to refine their technique in applying and maintaining appropriate contact force. By simulating the resistance and elasticity of cardiac tissue, the model provides realistic feedback, helping users develop a tactile sense for proper catheter positioning. This practice leads to more consistent and effective lesion creation, potentially improving procedural outcomes and reducing the risk of complications such as cardiac perforation or ineffective ablation.
Energy Delivery Simulation
While the atrial septal puncture model does not directly simulate energy delivery, it plays a vital role in preparing practitioners for this aspect of RF ablation. By providing a realistic anatomical environment, the model allows users to practice catheter positioning and stability maintenance during simulated energy delivery. This preparation is crucial for achieving consistent lesion formation in clinical settings. Trainees can focus on factors such as catheter orientation, stability, and duration of application, which directly influence the effectiveness of RF energy delivery and resultant lesion formation.
Pulmonary Vein Isolation Techniques
Pulmonary vein isolation is a cornerstone technique in RF ablation for atrial fibrillation treatment. The atrial septal puncture model's accurate representation of pulmonary vein anatomy allows practitioners to hone their skills in accessing and navigating these critical structures. Users can practice creating continuous, transmural lesions around pulmonary vein ostia, improving their ability to achieve complete electrical isolation. This targeted practice enhances the consistency of lesion formation in challenging anatomical locations, potentially leading to more successful outcomes in clinical procedures.
Conclusion
The atrial septal puncture model serves as an indispensable tool in the simulation of radiofrequency ablation procedures. Its anatomical accuracy, versatility, and ability to provide realistic tactile feedback make it an invaluable asset for medical training and device testing. By offering a safe environment to practice complex techniques such as transseptal puncture, catheter navigation, and lesion formation, these models contribute significantly to improving procedural skills and patient outcomes. As the field of cardiac electrophysiology continues to advance, the role of high-fidelity simulation tools in preparing the next generation of healthcare providers becomes increasingly crucial.
Contact Us
For more information on how Trandomed's advanced atrial septal puncture models can enhance your training programs or device development processes, please contact us at jackson.chen@trandomed.com. Our team is dedicated to providing cutting-edge simulation solutions that drive innovation and improve patient care in the field of cardiac electrophysiology.
References
Calkins H, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275-e444.
Sugumar H, et al. Advances in Atrial Septal Puncture Techniques. Current Cardiology Reports. 2019;21(11):133.
Miyazaki S, et al. Simulation-Based Training for Cardiac Electrophysiology Procedures. Journal of Arrhythmia. 2019;35(2):186-189.
Jongbloed MRM, et al. Atrial Fibrillation: Multi-Modality Imaging in Electrophysiology Interventions. Cardiovascular Imaging. 2020;13(1):145-159.
Opolski MP, et al. CT Imaging for Planning of Atrial Fibrillation Ablation. JACC: Cardiovascular Imaging. 2021;14(1):69-82.
Enriquez A, et al. Use of Intracardiac Echocardiography in Interventional Cardiology: Working With the Anatomy Rather Than Fighting It. Circulation. 2018;137(21):2278-2294.

_1734504197376.webp)
_1732843184544.webp)