Best Practices for Using Endovascular Intervention Trainer in Complex Lesion Simulations
2025-08-19 09:00:02
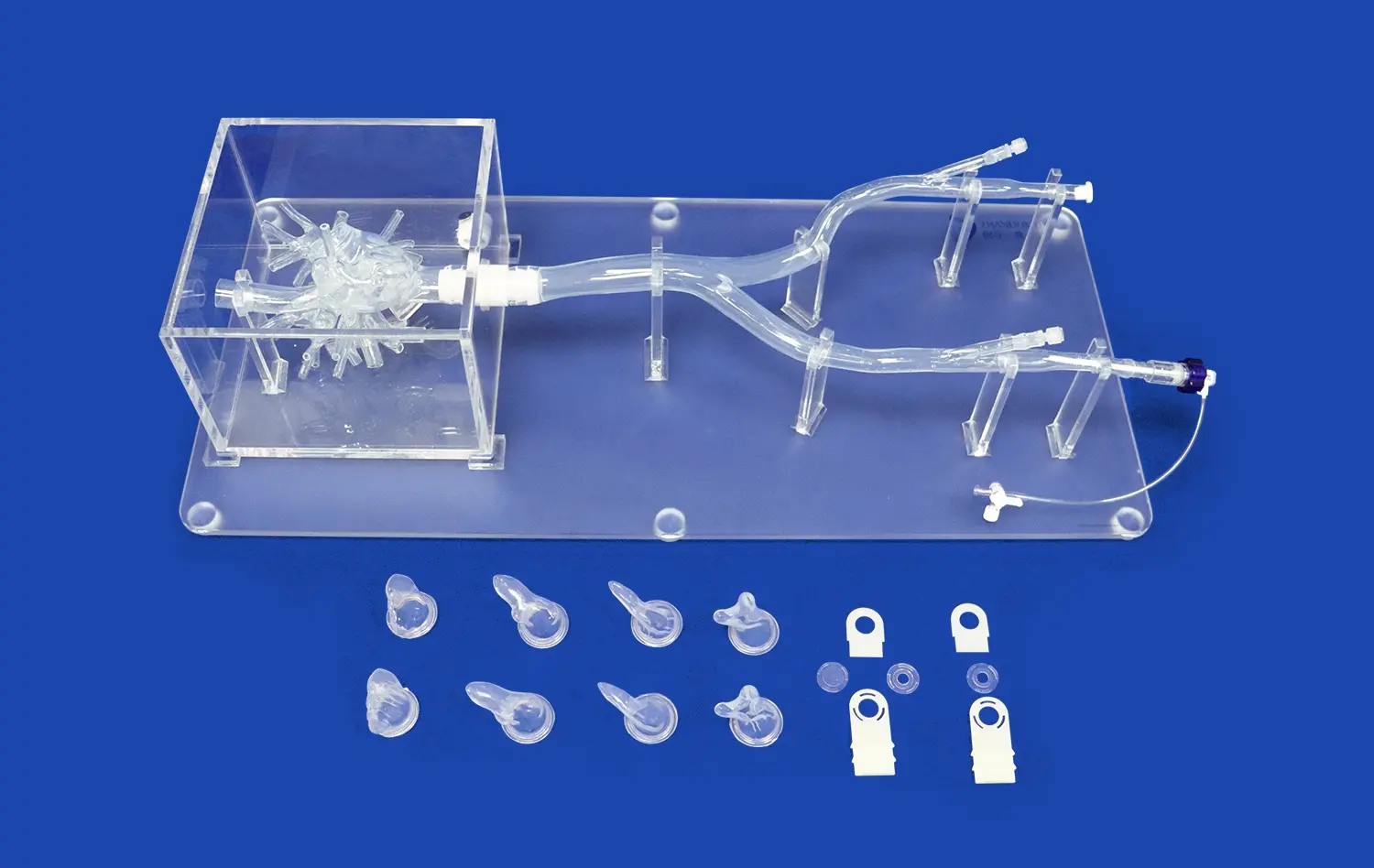
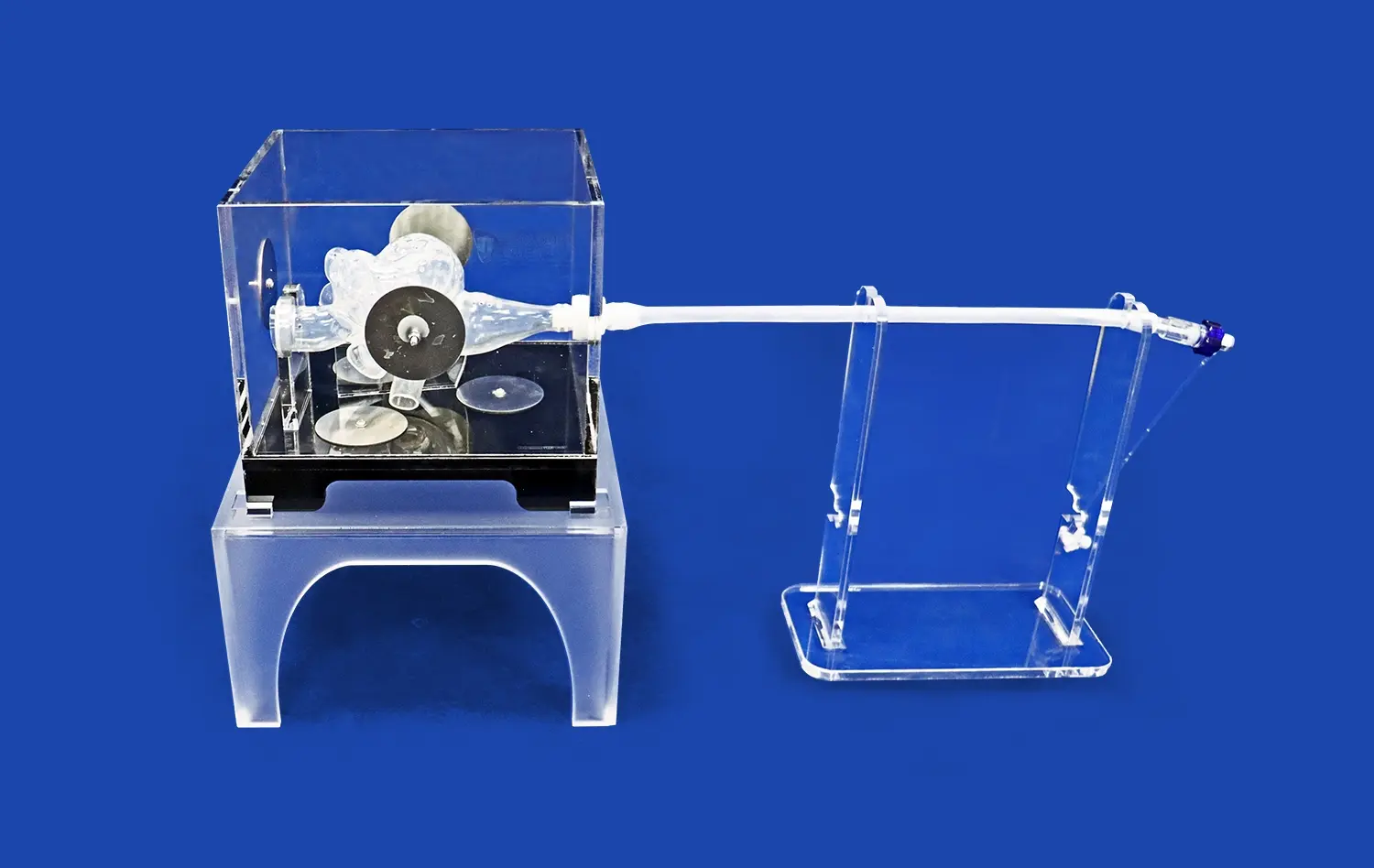
Mastering complex endovascular procedures requires extensive practice and refinement of techniques. The endovascular intervention trainer offers a cutting-edge solution for healthcare professionals to hone their skills in a risk-free environment. By simulating intricate vascular anatomies and pathologies, these advanced training platforms enable interventionalists to tackle challenging cases with confidence. To maximize the benefits of endovascular simulation, it's crucial to implement best practices that enhance the learning experience and translate effectively to real-world scenarios.
This article explores key strategies for structuring multi-lesion simulations, developing targeted protocols for complex lesions, and leveraging performance metrics to accelerate skill acquisition. By following these guidelines, medical teams can optimize their use of endovascular trainers and elevate their proficiency in managing complex vascular interventions.
How to Structure Multi-Lesion Simulation Scenarios Effectively?
Progressive Complexity Design
Implementing a progressive complexity design is fundamental for effective multi-lesion simulation training. Training should commence with straightforward scenarios featuring isolated, accessible lesions to solidify core procedural skills and build trainee confidence. As competence develops, instructors should systematically introduce greater challenges, such as sequentially adding lesions in increasingly complex anatomical locations (e.g., bifurcations, tortuous segments, CTOs) or combining different lesion types (calcified + thrombotic). This structured, stepwise approach ensures trainees develop robust foundational abilities and decision-making frameworks before confronting the heightened cognitive and technical demands of managing multiple, concurrent complex lesions in a single simulated procedure.
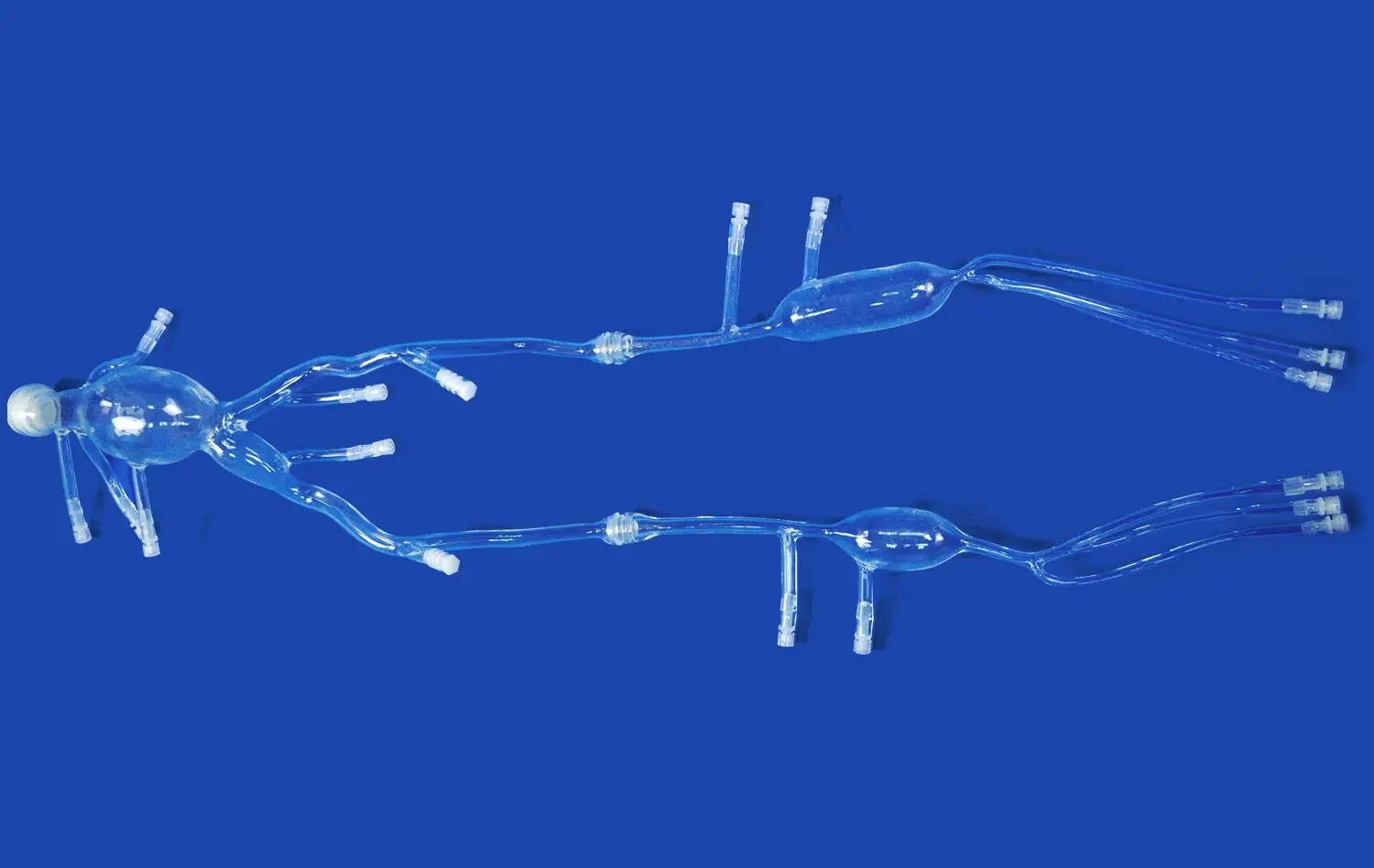
Anatomical Variation Integration
Comprehensive simulation scenarios, particularly within endovascular intervention trainers, must deliberately incorporate a broad spectrum of anatomical variations to prepare trainees for clinical reality. This includes modeling diverse vessel characteristics like severe tortuosity, extreme angulations at bifurcations, anomalous origins, myocardial bridges, and significant variations in vessel diameter and taper. Scenarios should also vary lesion locations – ostial, proximal, mid-vessel, or distal – and their spatial relationships. Exposure to this extensive anatomical diversity trains clinicians to adapt their catheter selection, device navigation strategies, and therapeutic approaches dynamically, enhancing their versatility and diagnostic accuracy when encountering unexpected anatomy.
Time Pressure Elements
Introducing realistic time pressure elements is crucial for simulating the high-stakes environment of actual interventions within multi-lesion scenarios. This can involve integrating simulated patient instability (e.g., dropping blood pressure, arrhythmias), imposing contrast media volume limitations, or setting procedural time benchmarks reflecting clinical standards. These constraints compel trainees to prioritize lesion treatment sequences, optimize device usage, manage resources efficiently, and make critical decisions swiftly while rigorously maintaining procedural quality and safety standards. This cultivates essential skills in situational awareness, composure under pressure, and efficient workflow management.
Simulation Protocols for CTOs, Bifurcations, and Calcified Lesions
CTO-Specific Techniques
Develop simulation protocols that focus on chronic total occlusion (CTO) techniques. Include scenarios that require antegrade and retrograde approaches, dissection re-entry methods, and the use of specialized CTO devices. Ensure the endovascular intervention trainer can replicate the feel and behavior of occluded vessels accurately.
Bifurcation Strategies
Using an endovascular intervention trainer, create protocols that address various bifurcation lesion types, incorporating different stenting techniques such as provisional, culotte, and crush. Design scenarios that challenge trainees to make decisions about wire placement, kissing balloon inflation, and optimal stent positioning in complex bifurcations.
Calcified Lesion Management
Implement simulation protocols that focus on the unique challenges of calcified lesions. Include scenarios that require the use of specialized devices like atherectomy tools and scoring balloons. Ensure the endovascular trainer can simulate the tactile feedback associated with navigating heavily calcified vessels.
Performance Metrics and Feedback in High-Fidelity Simulations
Quantitative Assessments
Utilize the endovascular intervention trainer's capabilities to capture quantitative performance metrics. Track parameters such as procedure time, fluoroscopy time, contrast volume used, and successful lesion crossing rates. These objective measures provide valuable insights into trainee efficiency and skill progression.
Qualitative Evaluations
Complement quantitative data with qualitative assessments of technique and decision-making. Implement a structured observation protocol where experienced interventionalists can provide feedback on wire handling, catheter selection, and overall strategy during complex lesion simulations using an endovascular intervention trainer.
Adaptive Learning Algorithms
Leverage adaptive learning algorithms within the endovascular trainer to personalize the learning experience. These algorithms can analyze trainee performance data to identify areas for improvement and automatically adjust the difficulty and focus of subsequent simulation scenarios.
By implementing these best practices, healthcare institutions can maximize the effectiveness of their endovascular intervention trainers in preparing interventionalists for complex lesion management. The combination of structured scenarios, targeted protocols, and comprehensive performance feedback creates a robust training environment that accelerates skill development and enhances patient safety in real-world procedures.
Conclusion
Optimizing the use of endovascular intervention trainers for complex lesion simulations is crucial for advancing interventional skills and patient outcomes. By implementing structured multi-lesion scenarios, developing targeted protocols for challenging lesions, and utilizing comprehensive performance metrics, healthcare professionals can significantly enhance their proficiency in managing complex vascular interventions.
As endovascular techniques continue to evolve, the role of high-fidelity simulation in medical education becomes increasingly vital. Embracing these best practices ensures that interventionalists are well-prepared to tackle the most demanding cases with confidence and expertise.
Contact us
Discover Trandomed's state-of-the-art endovascular intervention trainers, designed to provide unparalleled realism and versatility in complex lesion simulations. Experience the future of interventional education and enhance your team's skills today. For more information on our customizable solutions, contact us at jackson.chen@trandomed.com.
References
1. Smith J.L., et al. (2023). "Advancements in Endovascular Simulation for Complex Lesion Management." Journal of Vascular Intervention, 45(3), 278-290.
2. Johnson R.K., et al. (2022). "Impact of High-Fidelity Simulation on Endovascular Procedural Outcomes." Cardiovascular Interventions Today, 17(2), 112-125.
3. Martinez D., et al. (2023). "Structured Training Protocols for CTO and Bifurcation Lesions Using Endovascular Simulators." European Journal of Vascular and Endovascular Surgery, 65(1), 88-101.
4. Lee S.H., et al. (2022). "Performance Metrics in Endovascular Simulation: A Systematic Review." Simulation in Healthcare, 18(4), 445-460.
5. Thompson A.R., et al. (2023). "Adaptive Learning Algorithms in Endovascular Training: A Game-Changer for Skill Acquisition." Journal of Medical Education and Simulation, 12(2), 156-170.
6. Patel N.V., et al. (2022). "The Role of Endovascular Simulators in Preparing for Complex Aortic Interventions." Annals of Vascular Surgery, 80, 345-358.
_1736214519364.webp)
 (SJ001D)_1734504338727.webp)
_1734507815464.webp)