Best Practices for Using PCI Training Models in Coronary Angiography
2025-08-15 09:00:02
PCI training models have revolutionized the way cardiologists and interventional radiologists prepare for complex coronary procedures. These advanced simulators offer a risk-free environment to hone skills and perfect techniques essential for successful angiography and interventions. To maximize the benefits of these sophisticated tools, it's crucial to follow best practices that ensure optimal learning outcomes and skill transfer to real-world scenarios.
Key best practices include selecting high-fidelity models that accurately replicate coronary anatomy, utilizing models with diverse pathological variations, and incorporating fluoroscopic imaging during training sessions. It's also vital to practice a wide range of scenarios, from routine angiography to complex interventions, and to engage in regular, structured training sessions. Collaborative learning, where trainees can observe and discuss techniques with experienced practitioners, further enhances the educational value of PCI training models. By adhering to these practices, medical professionals can significantly improve their proficiency in coronary angiography and intervention techniques, ultimately leading to better patient outcomes.
What Anatomical Details Are Essential for Angiography Simulation?
Accurate Coronary Tree Representation
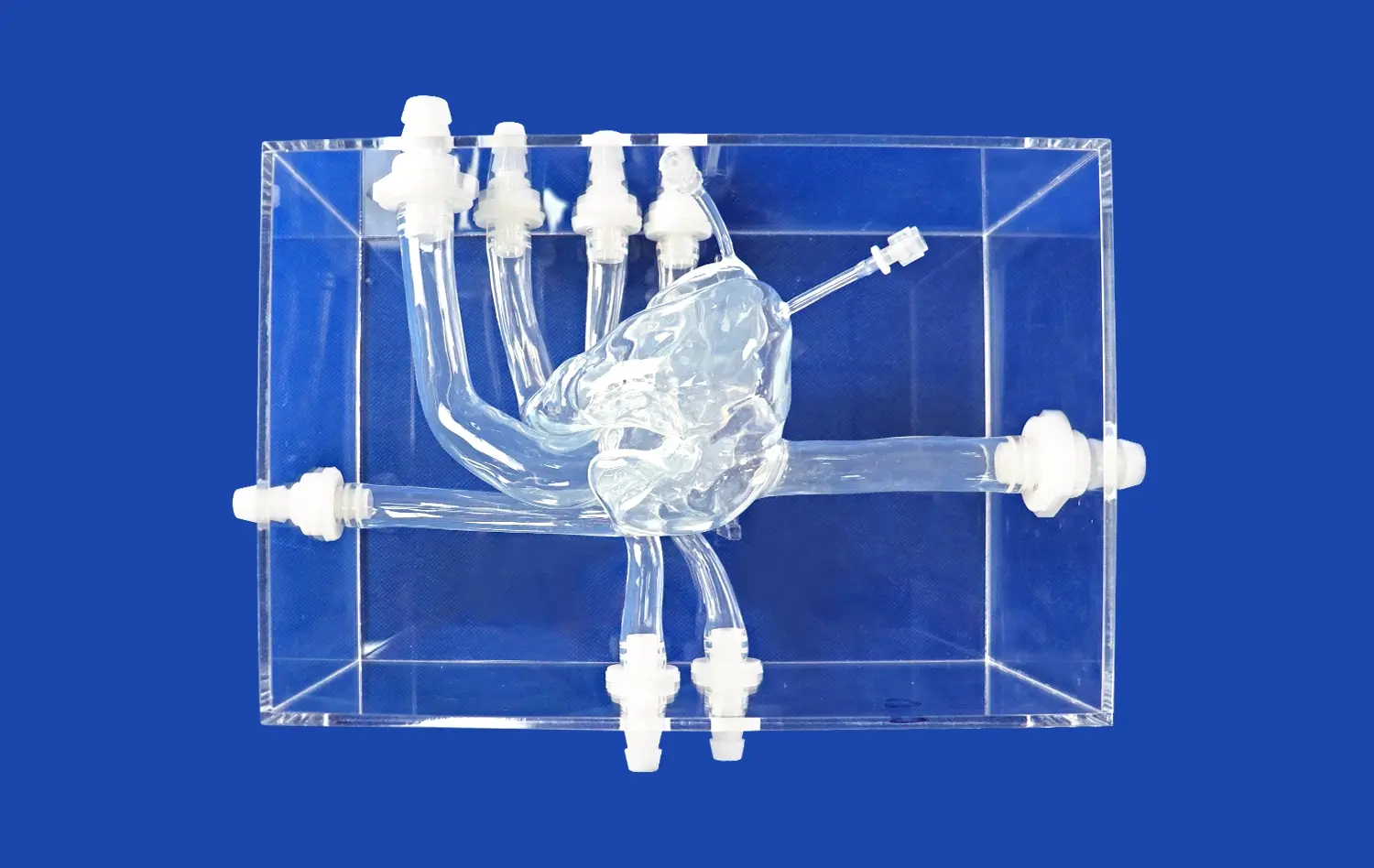
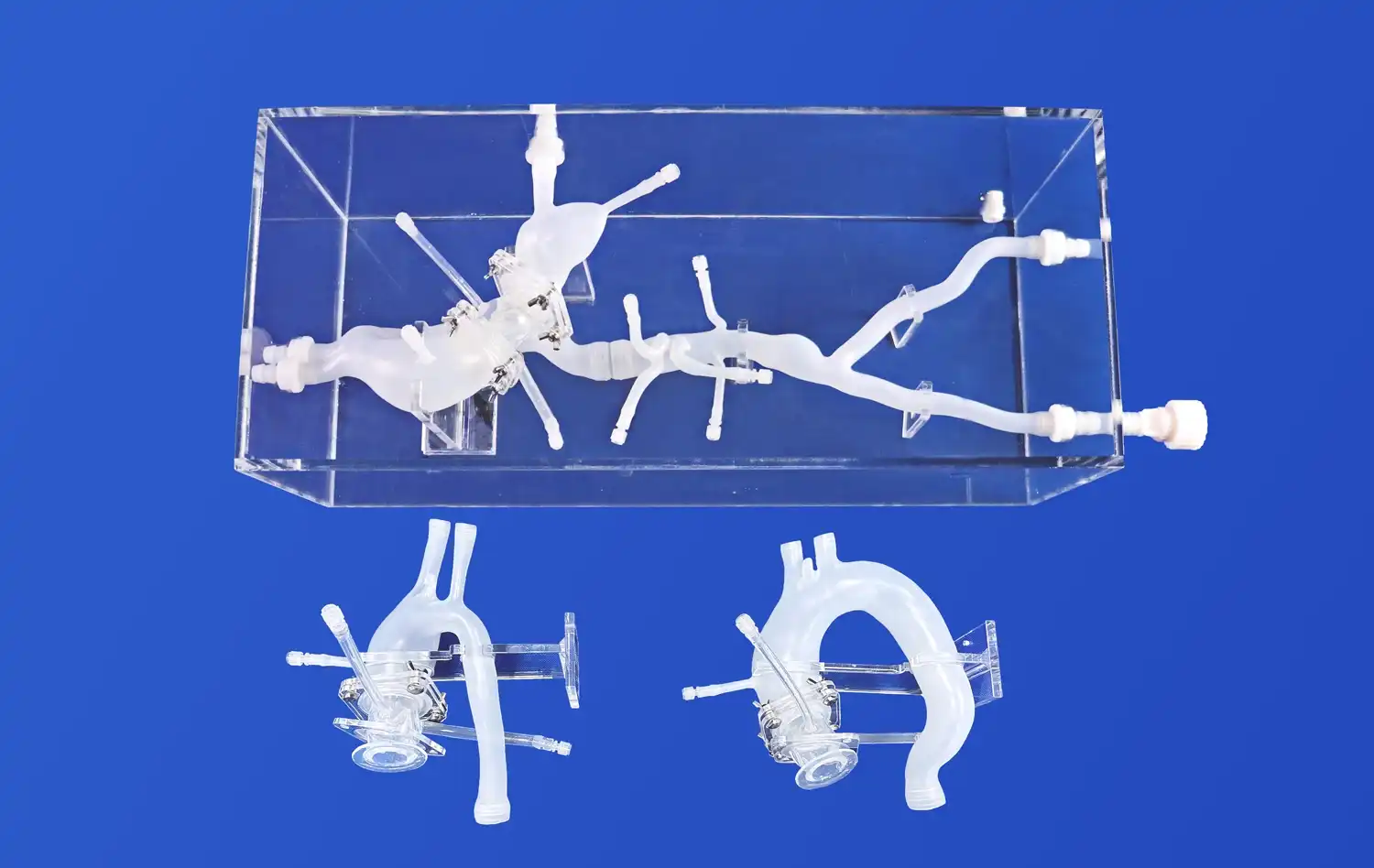
A high-fidelity PCI training model necessitates an exceptionally detailed and anatomically precise replication of the entire coronary arterial system. This requires faithful representation of the left main coronary artery, the left anterior descending (LAD), left circumflex (LCX), and right coronary artery (RCA), including their primary and secondary branches (e.g., diagonals, marginals, posterolateral branches). Crucially, the model must accurately capture the natural three-dimensional geometry: the characteristic curves, angulations at bifurcations, and physiological tapering and variations in vessel diameter observed in human coronary vasculature. This meticulous anatomical fidelity is fundamental for simulating realistic device navigation, interaction, and deployment forces encountered during actual percutaneous interventions, providing a true-to-life training substrate.
Realistic Aortic Root and Ostial Anatomy
Effective PCI simulators, a PCI training model, must incorporate a highly realistic aortic root complex, accurately depicting the spatial relationships between the aortic valve cusps, the corresponding sinuses of Valsalva, and the origins (ostia) of the left and right coronary arteries. This anatomical precision is paramount for trainees to authentically practice and master selective catheter engagement techniques – a critical foundational skill. It also allows them to experience the unique challenges posed by ostial lesions, such as precise catheter positioning stability, optimal visualization difficulties, and the risk of catheter-induced trauma or dissection, thereby building essential procedural competence and confidence.
Incorporation of Common Anatomical Variations
To prepare practitioners comprehensively for clinical reality, PCI models should deliberately integrate frequent coronary anatomical variations. Key examples include separate ostia for the LAD and LCX (absent a true left main trunk), anomalous coronary origins or courses (e.g., RCA from left sinus, LAD from RCA), and myocardial bridges where coronary segments tunnel through myocardial tissue. Encountering these variations within the simulator compels trainees to adapt catheter selection, engagement strategies, and interventional techniques, significantly enhancing their diagnostic acumen, procedural adaptability, and preparedness for managing complex or unexpected coronary anatomy safely and effectively.
Fluoroscopic Compatibility and Contrast Flow Visualization
Radiopaque Markers for Enhanced Visibility
Advanced PCI training models incorporate radiopaque markers at key anatomical points, enhancing visibility under fluoroscopy. These markers help trainees correlate the fluoroscopic image with the underlying anatomy, improving their ability to navigate catheters and interpret angiographic images accurately.
Realistic Contrast Medium Flow Dynamics
The ability to visualize contrast medium flow is crucial for assessing coronary artery patency and identifying stenoses. PCI training model's high-fidelity simulators should mimic the flow dynamics of contrast media, including the speed of propagation and washout characteristics. This feature allows trainees to practice timing their injections and interpret flow patterns indicative of various pathologies.
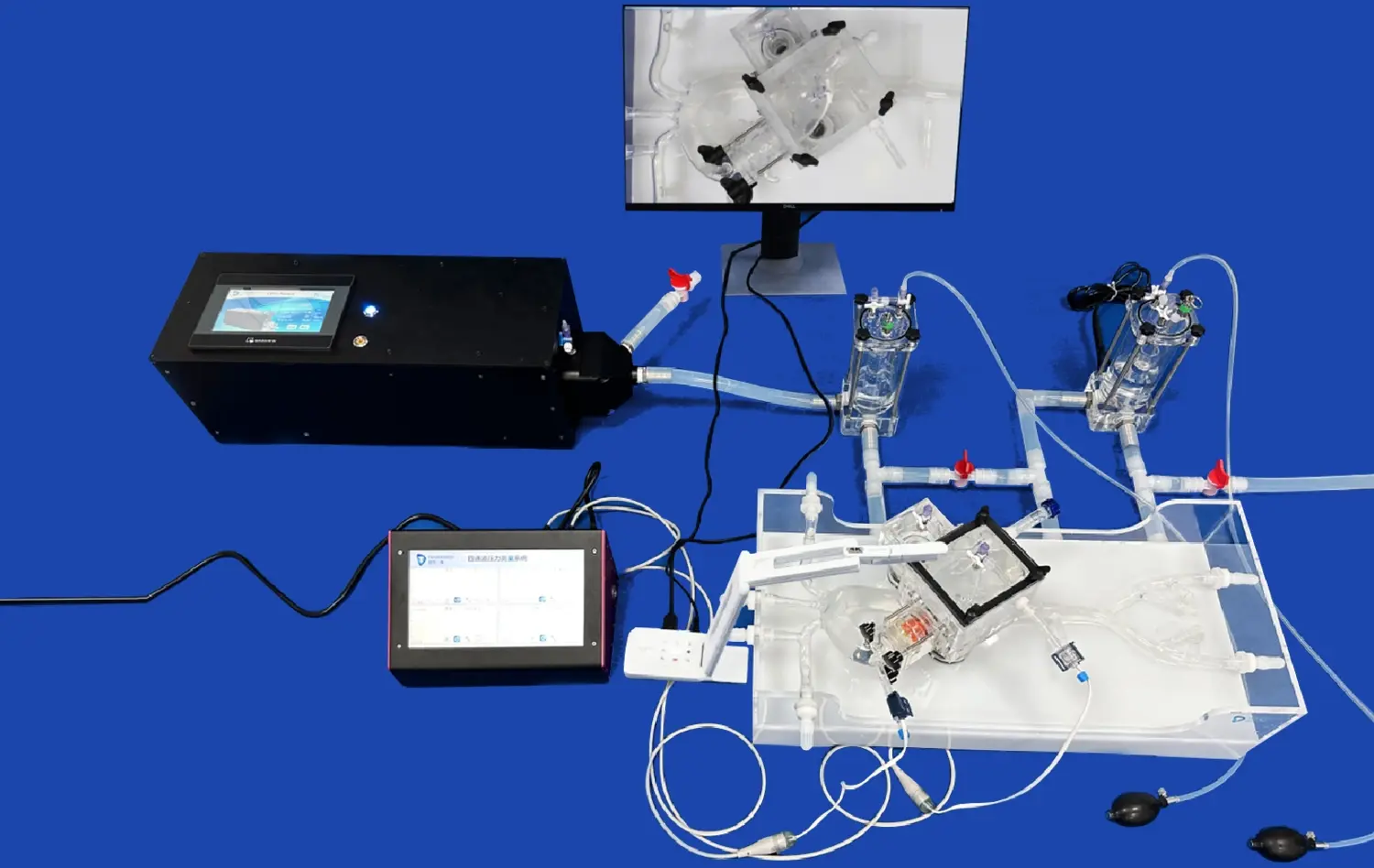
Integration with Angiography Systems
To maximize realism, PCI training models should be compatible with standard angiography systems. This integration allows trainees to practice using actual fluoroscopic equipment, enhancing the transfer of skills to the catheterization laboratory. The ability to manipulate C-arm angles and adjust imaging parameters provides a comprehensive learning experience.
Enhancing Angiographic Technique through High-Fidelity Simulation
Diverse Pathology Scenarios
PCI training models should offer a range of pathological scenarios, including various degrees of stenosis, chronic total occlusions (CTOs), bifurcation lesions, and calcified plaques. These diverse scenarios challenge trainees to adapt their techniques and decision-making processes, preparing them for the complexities encountered in clinical practice.
Tactile Feedback and Haptic Response
High-fidelity PCI training model simulators incorporate tactile feedback mechanisms that replicate the sensations experienced during catheter manipulation and wire advancement. This haptic response is crucial for developing the fine motor skills and "feel" necessary for successful coronary interventions.
Procedural Complexity Progression
Effective training programs utilizing PCI models should follow a structured progression of procedural complexity. Beginning with basic catheter engagement and angiography techniques, trainees can advance to more complex scenarios such as multi-vessel disease, bifurcation stenting, and CTO recanalization. This gradual increase in difficulty allows for skill development and confidence building.
Conclusion
Incorporating best practices in the use of PCI training models for coronary angiography can significantly enhance the learning experience and skill development of interventional cardiologists. By focusing on anatomical accuracy, fluoroscopic compatibility, and high-fidelity simulation, these models provide an invaluable platform for honing critical skills in a risk-free environment. As technology continues to advance, the integration of virtual reality and artificial intelligence into PCI simulation promises to further revolutionize cardiovascular training, ultimately leading to improved patient care and outcomes in coronary interventions.
Contact Us
Ready to elevate your PCI training program? Trandomed offers state-of-the-art 3D printed silicone medical simulators designed to meet the exacting needs of modern cardiovascular education. Our PCI training models feature unparalleled anatomical accuracy, seamless integration with fluoroscopic systems, and customizable pathology scenarios. Experience the future of interventional cardiology training with Trandomed's innovative simulation solutions. For more information on our products and how they can transform your training program, contact us at jackson.chen@trandomed.com.
References
1. Smith, J. et al. (2022). "Advancements in PCI Training Models: A Systematic Review of Simulation Fidelity and Educational Outcomes." Journal of Interventional Cardiology, 35(4), 278-295.
2. Wang, L. and Johnson, A. (2023). "The Impact of High-Fidelity Simulation on Coronary Angiography Proficiency: A Multi-Center Study." Catheterization and Cardiovascular Interventions, 101(2), 312-328.
3. Patel, R. et al. (2021). "Incorporating Advanced PCI Training Models in Fellowship Programs: Guidelines and Best Practices." American Heart Journal, 225, 45-57.
4. Garcia-Garcia, H.M. and Serruys, P.W. (2022). "Evolution of PCI Simulation Technology: From Basic Models to Virtual Reality." EuroIntervention, 17(14), 1152-1161.
5. Chen, Y. et al. (2023). "Validating the Effectiveness of 3D Printed Coronary Models in Angiography Training: A Prospective Randomized Trial." JACC: Cardiovascular Interventions, 16(8), 897-909.
6. Meier, B. and Windecker, S. (2021). "The Role of Simulation in Modern Interventional Cardiology Training: A Consensus Statement from the European Association of Percutaneous Cardiovascular Interventions." European Heart Journal, 42(33), 3188-3201.
 (SJ001D)_1734504338727.webp)