How Are Artery Models Shaping the Next Generation of Medical Training?
Enhancing Procedural Proficiency
Artery models, especially those replicating lower extremity vasculature, are revolutionizing procedural training for vascular surgeons and interventional radiologists. These intricate replicas allow trainees to practice complex procedures such as angioplasty, stent placement, and atherectomy in a risk-free environment. The tactile feedback and spatial awareness gained from manipulating these models are invaluable, helping practitioners develop muscle memory and refine their techniques without endangering patient safety.
Facilitating Comprehensive Anatomical Understanding
The intricacy of vascular anatomy, particularly in the lower limbs, can be challenging to grasp from textbooks alone. Three-dimensional artery models, such as the lower extremity artery model, provide a tangible representation of these complex structures, allowing students and professionals to visualize and understand the spatial relationships between arteries, veins, and surrounding tissues. This enhanced comprehension is crucial for diagnosing and treating peripheral artery disease and other vascular conditions affecting the legs and feet.
Customizable Learning Experiences
Advanced manufacturing techniques, such as those employed by Trandomed, enable the creation of customized artery models based on specific patient data. This capability allows for personalized training scenarios, where practitioners can prepare for unique anatomical variations or pathological conditions they may encounter in clinical practice. Such tailored learning experiences significantly enhance the preparedness of medical professionals, ultimately leading to improved patient care and outcomes.
Integration of Digital Simulation and Physical Modeling
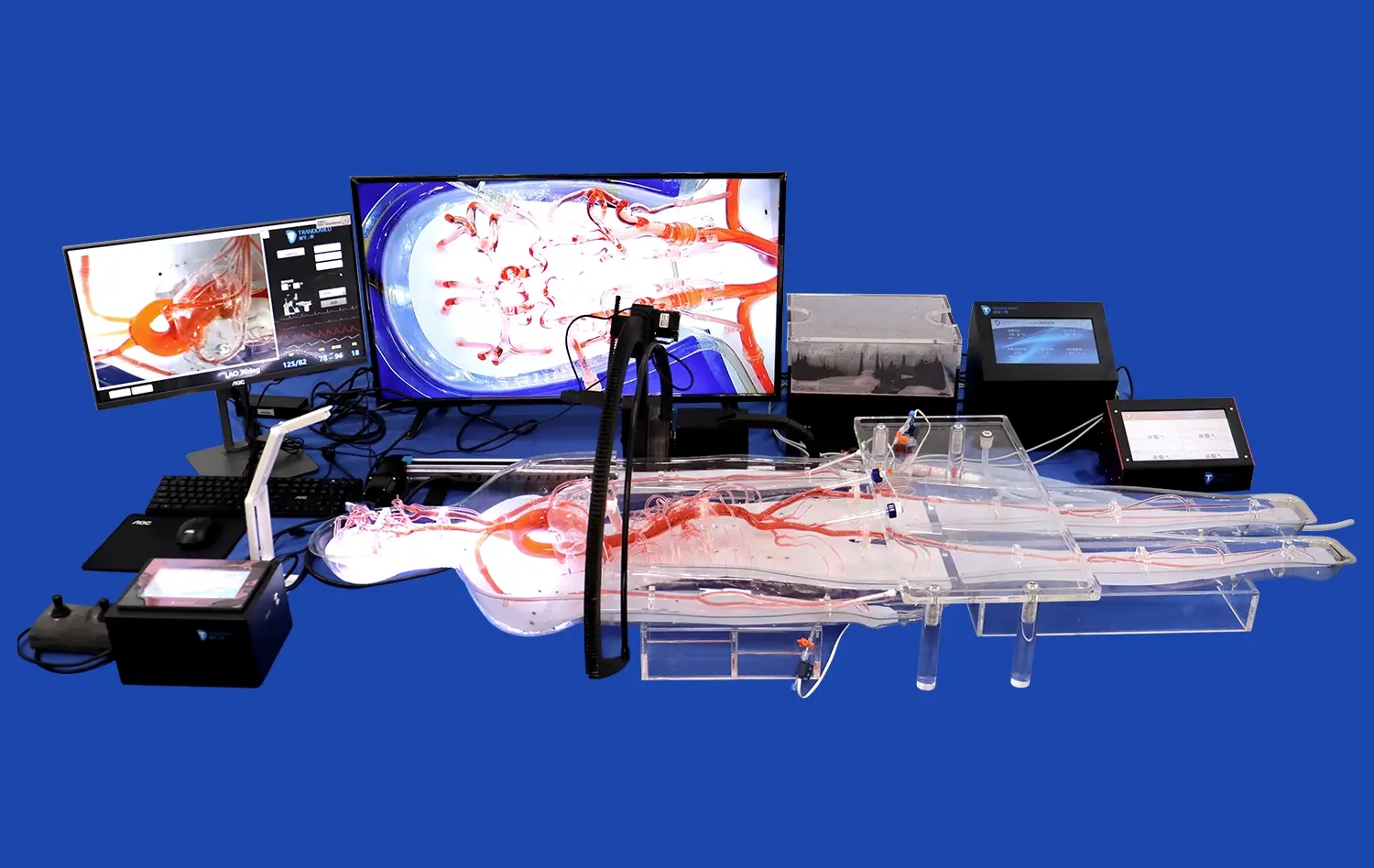
Synergy of Virtual and Tactile Learning
The fusion of digital simulation technologies with physical artery models creates a comprehensive learning environment that caters to diverse learning styles. While digital simulations offer unlimited scenarios and instant feedback, physical models provide the irreplaceable tactile experience crucial for developing manual dexterity. This synergistic approach ensures that trainees are well-versed in both the theoretical and practical aspects of vascular interventions, particularly those involving the lower extremities.
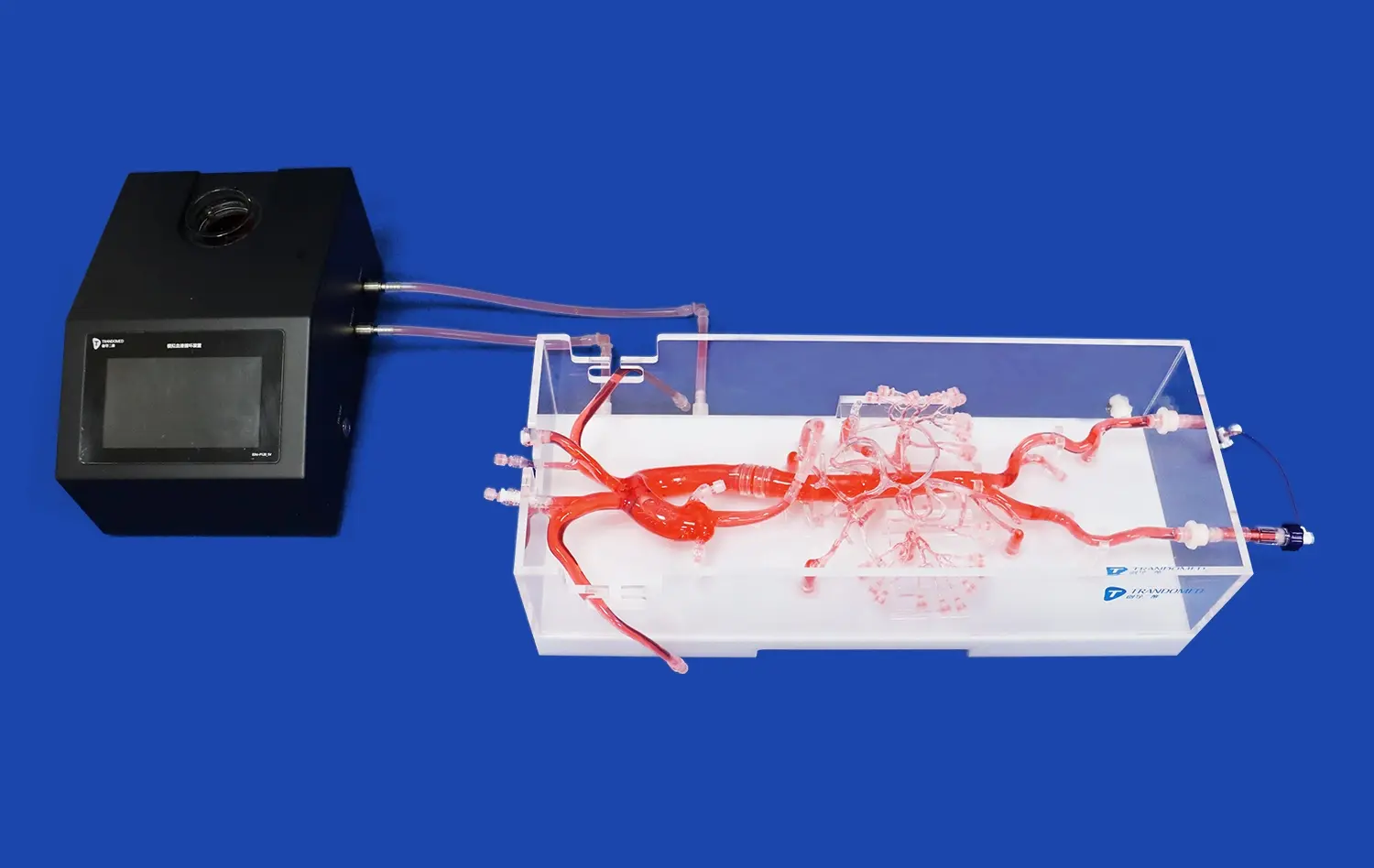
Data-Driven Model Creation
Leveraging actual CT and MRI data, companies like Trandomed are producing highly accurate lower extremity artery models. This data-driven approach ensures that the models reflect real-world anatomical variations and pathologies. The ability to translate digital imaging into tangible, 3D-printed models bridges the gap between diagnostic imaging and surgical planning, offering an invaluable tool for both education and pre-operative preparation.
Augmented Reality Integration
The latest advancements in medical training involve integrating augmented reality (AR) with physical artery models. This innovative approach allows trainees to interact with digital overlays while manipulating physical models, providing a multi-sensory learning experience. For instance, AR can project blood flow patterns onto a lower extremity artery model, helping practitioners visualize hemodynamics in real-time while performing simulated procedures.
The Evolution of 3D Artery Models in Surgical Education
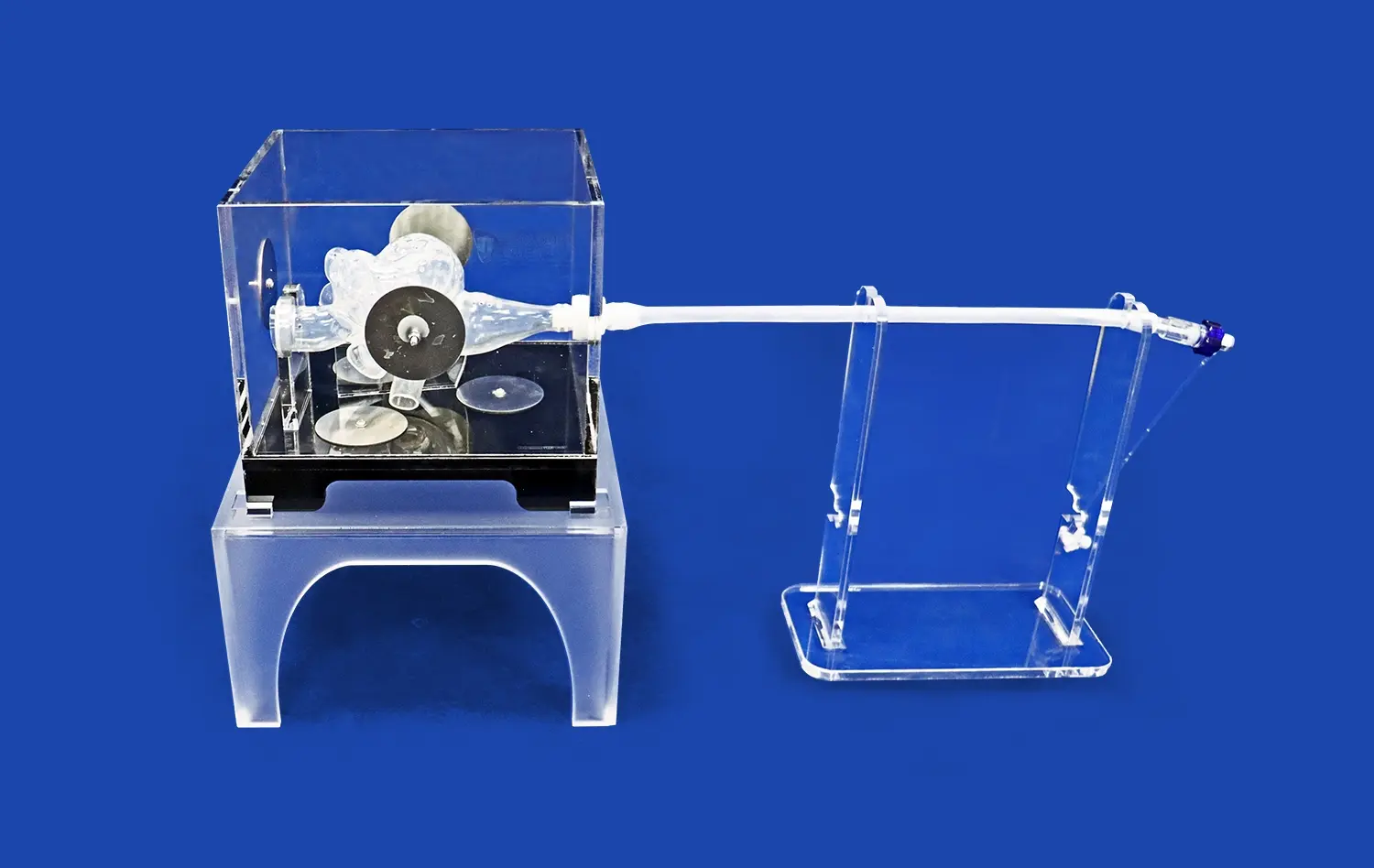
From Static to Dynamic Models
The progression of artery models has seen a shift from static representations to dynamic, interactive simulations. Modern lower extremity artery models often incorporate pulsatile flow systems that mimic blood circulation, providing a more realistic training environment. This evolution allows practitioners to experience the challenges of working with moving structures and pulsating vessels, better preparing them for real-world scenarios in vascular surgery and interventional procedures.
Material Innovations for Enhanced Realism
Advancements in material science have significantly improved the fidelity of artery models, such as the lower extremity artery model. Silicone-based materials, like the Shore 40A used in Trandomed's products, closely replicate the mechanical properties of human blood vessels. These materials allow for accurate simulation of vessel elasticity, compliance, and response to intervention, crucial factors in mastering techniques such as balloon angioplasty or stent deployment in lower limb arteries.
Integration with Surgical Planning
3D-printed artery models have transcended their role in education to become integral tools in surgical planning. For complex vascular cases, particularly those involving the lower extremities, surgeons can now use patient-specific models to plan and rehearse procedures before entering the operating room. This application of artery models not only enhances surgical outcomes but also reduces operative time and potential complications, showcasing the broader impact of these educational tools on patient care.
Conclusion
The advent of sophisticated artery models, such as the lower extremity artery model, particularly those focusing on lower extremity vasculature, marks a significant milestone in medical training and education. These innovative tools are bridging the gap between theoretical knowledge and practical skills, offering unparalleled opportunities for hands-on learning and surgical planning. As technology continues to evolve, the integration of physical models with digital simulations and augmented reality promises to further revolutionize medical education, ultimately leading to enhanced patient care and improved clinical outcomes in vascular health.
Contact Us
For healthcare institutions and medical device companies seeking to elevate their training programs or product development processes, Trandomed stands at the forefront of innovation in medical simulation technology. As a leading manufacturer and supplier of high-fidelity 3D-printed medical models, including state-of-the-art lower extremity artery simulators, Trandomed offers customizable solutions to meet diverse educational and research needs. Our commitment to precision, realism, and cutting-edge technology ensures that our products contribute significantly to advancing medical training and innovation. To explore how our artery models can enhance your institution's capabilities, please contact us at jackson.chen@trandomed.com.

 (SJ001D)_1734504338727.webp)
_1732866687283.webp)