Medical practitioners' approaches to patient care and training have been completely transformed by sophisticated neurovascular simulators. The cerebral model represents a sophisticated anatomical replication system that accurately simulates the brain's vascular architecture, including critical structures like the Circle of Willis and various aneurysm formations. These lifelike platforms for procedure practice, device testing, and patient education make these high-fidelity simulators essential resources for medical schools, hospitals, research labs, and training facilities. These models help close the gap between clinical practice and theoretical understanding by providing tactile, three-dimensional representations of intricate neurovascular anatomy, which eventually improves patient safety and educational outcomes.

Understanding the Cerebral Model in Clinical and Educational Contexts
What Defines a Modern Neurovascular Simulator?
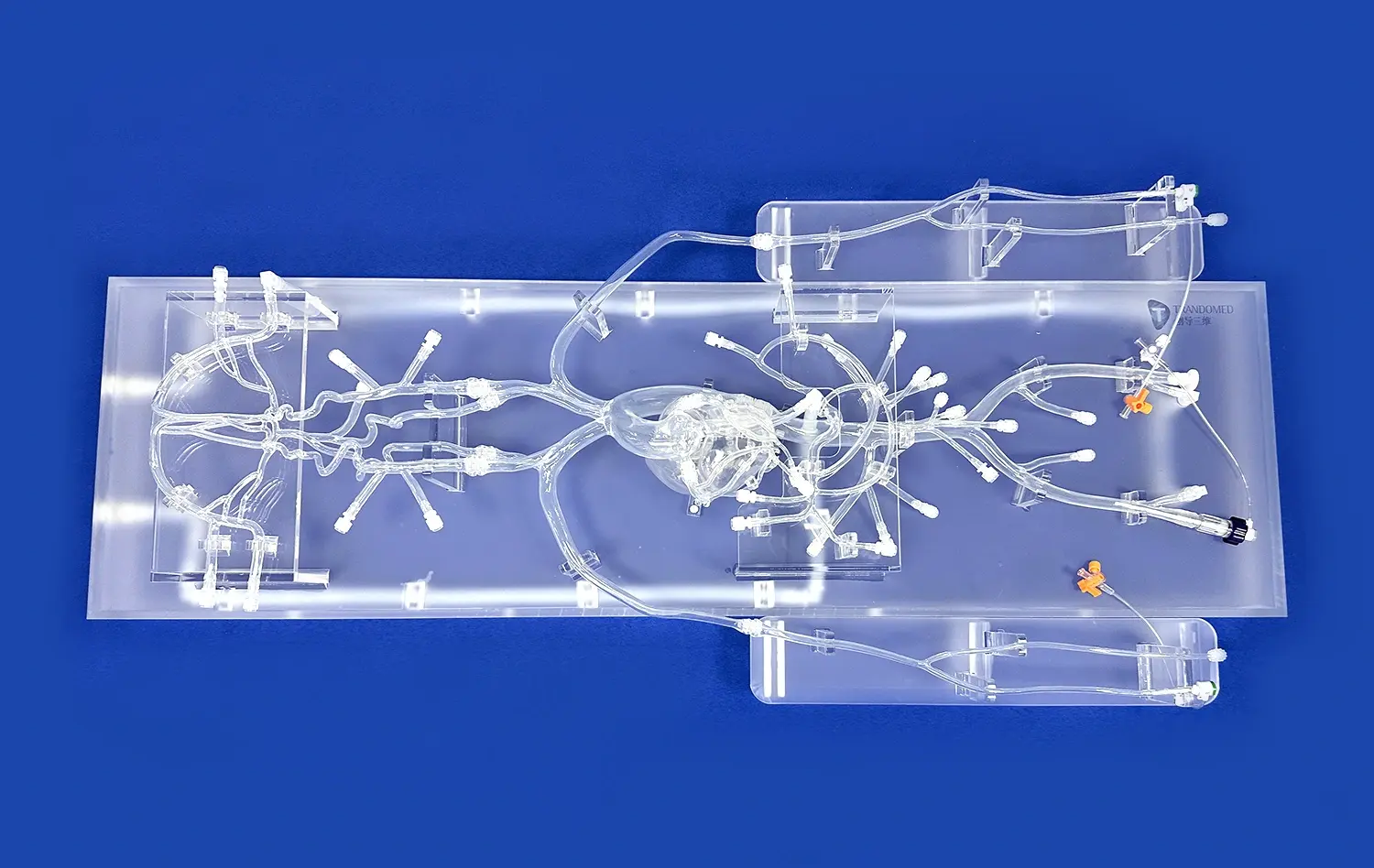
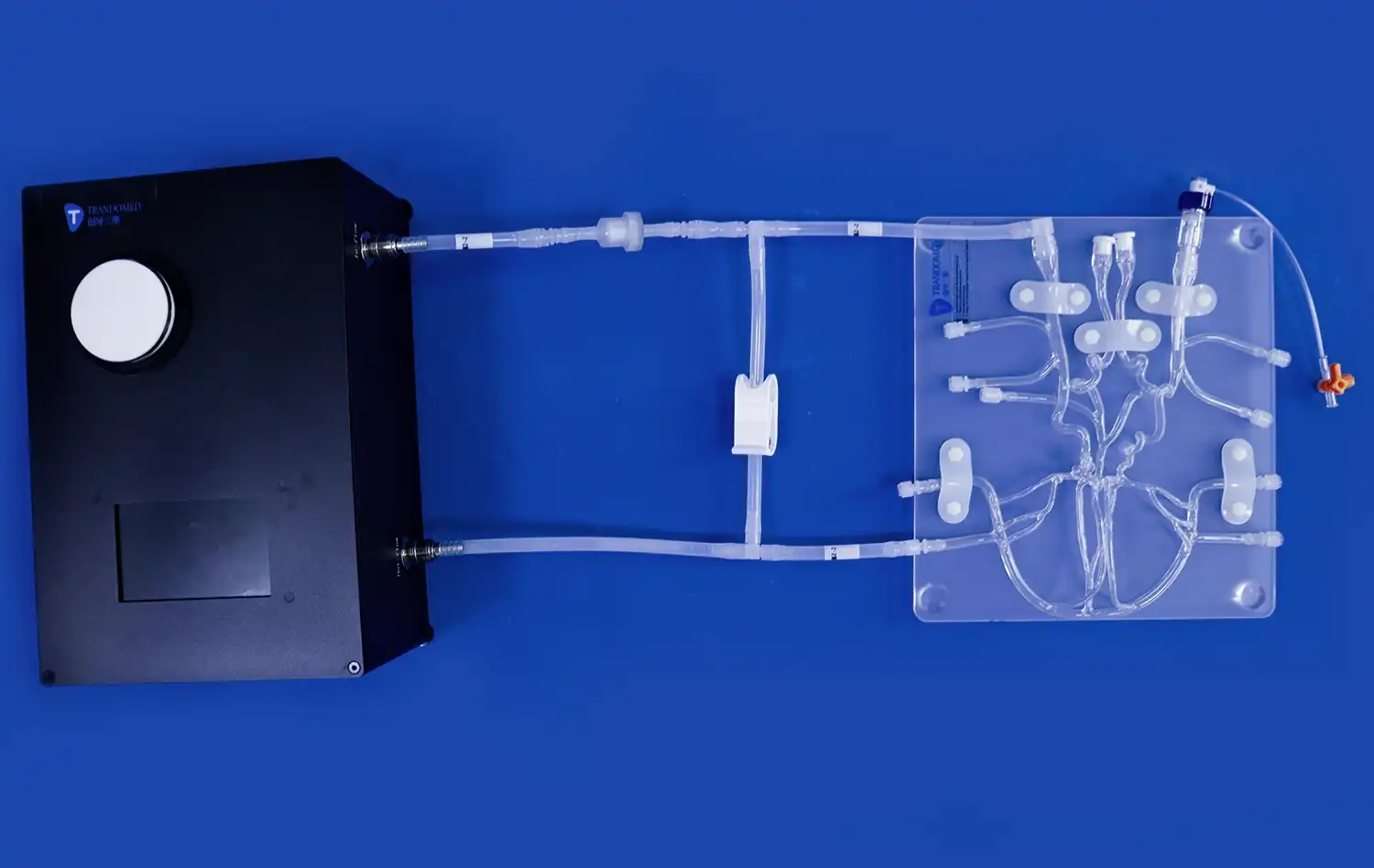
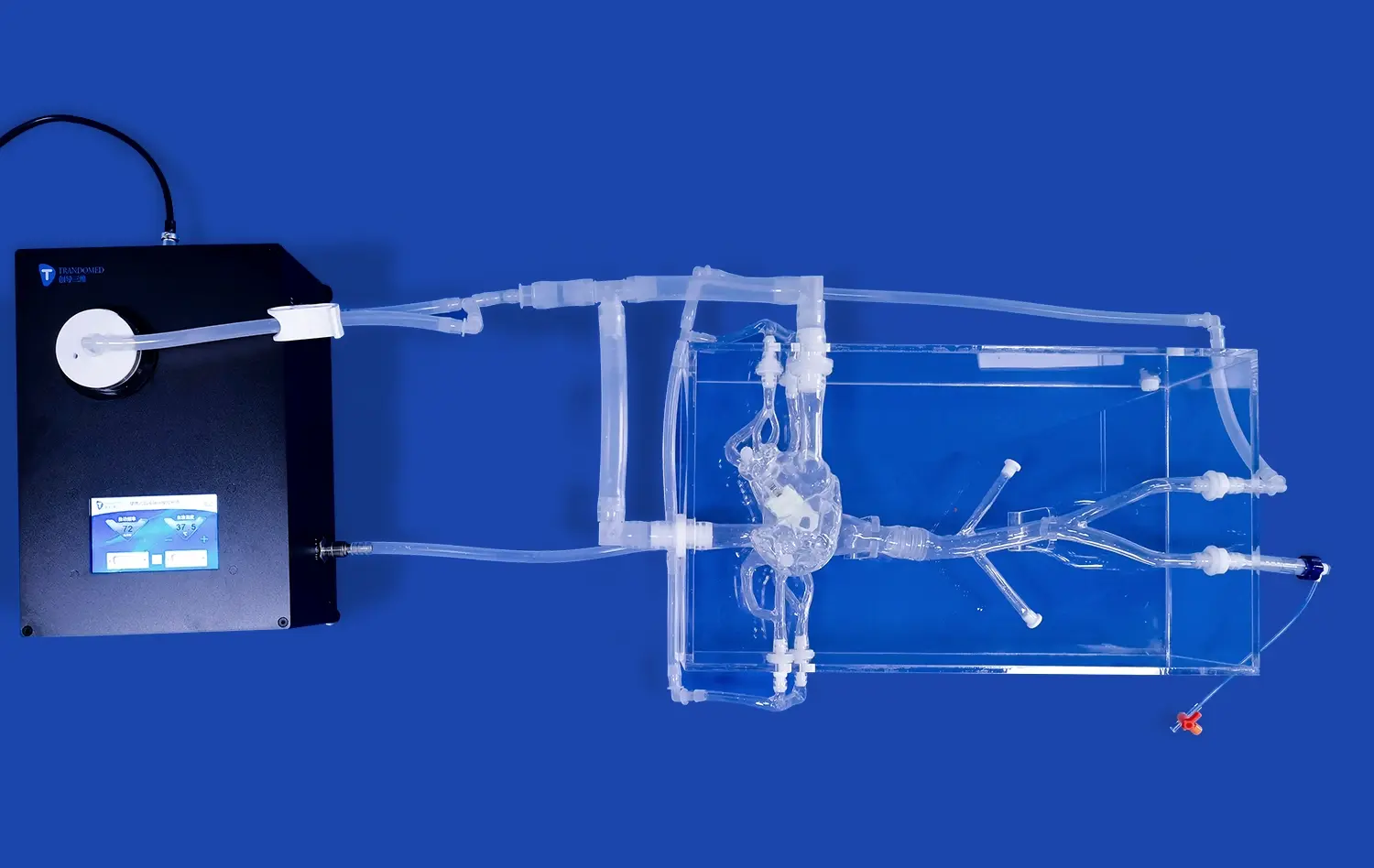
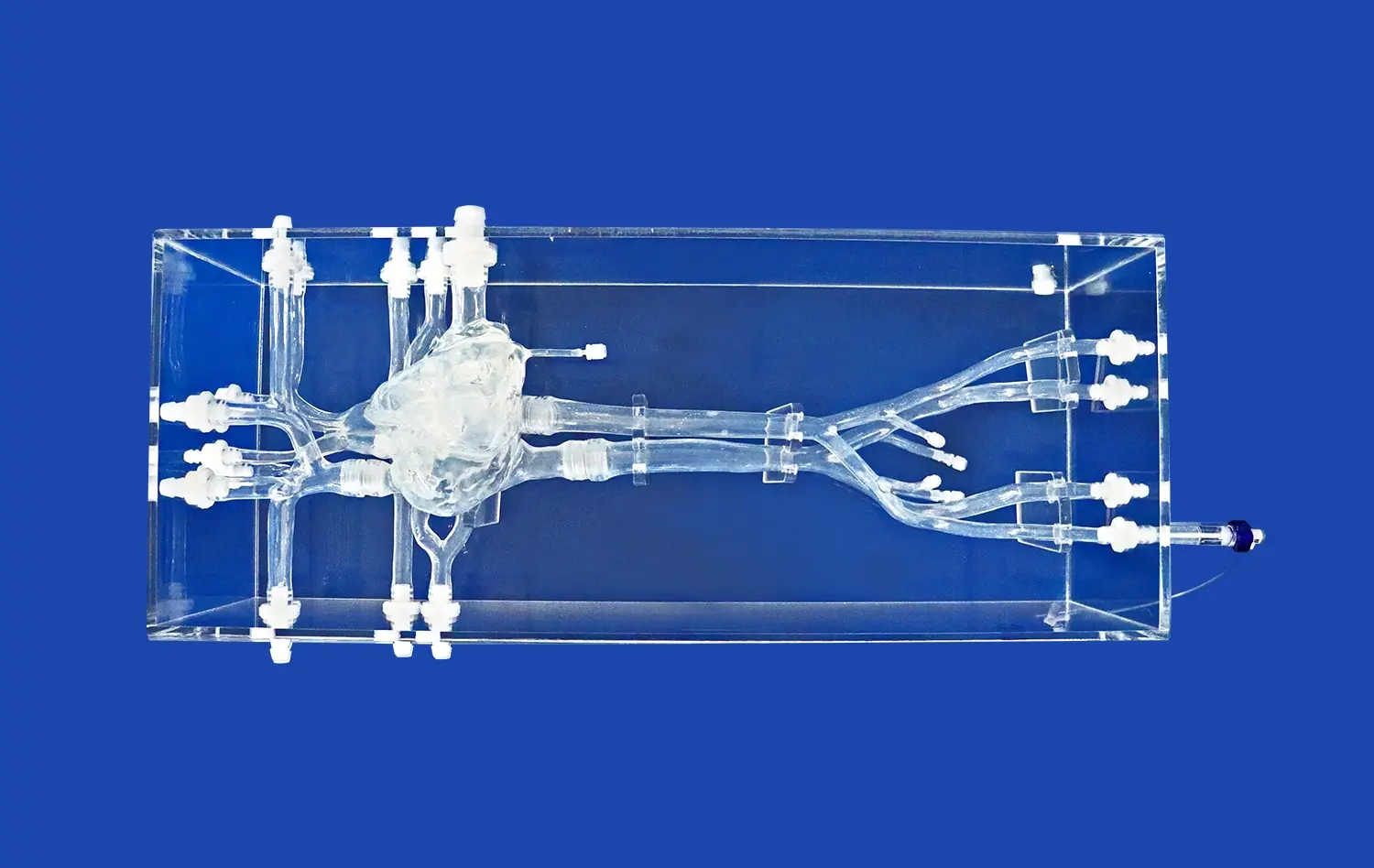
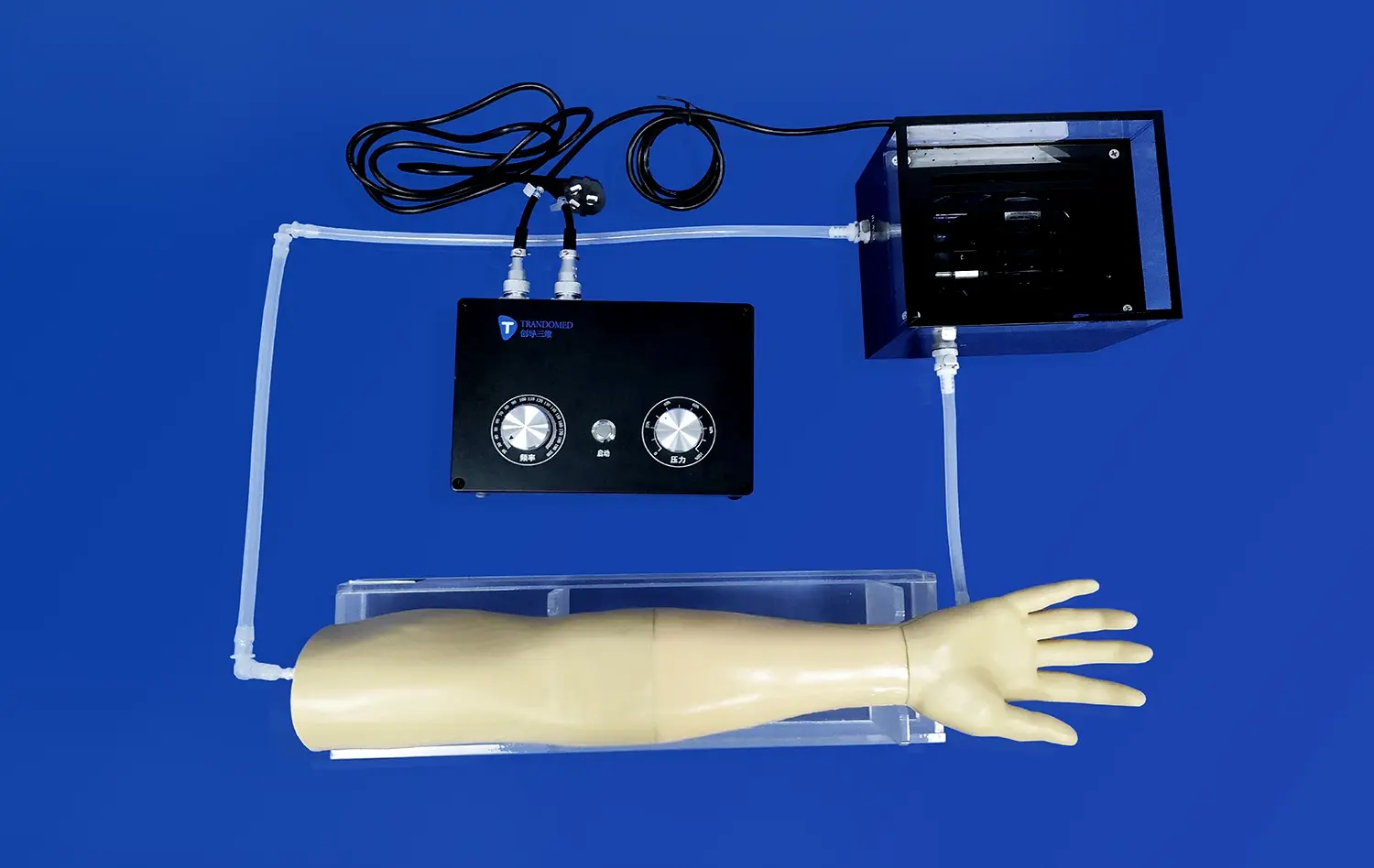
The complex structure of cerebral blood arteries can be precisely modeled by a neurovascular simulator. Trandomed's cerebral model, also known as the Circle of Willis Aneurysm III (Product No. SJK002D), exemplifies this technology through its detailed representation of arterial structures. This simulator, which is made of medical-grade Silicone Shore 40A, offers a realistic tactile feel that closely resembles the characteristics of genuine tissue during interventional treatments. Aneurysms on the ophthalmic segment, basilar artery, carotid artery, and middle cerebral artery are included in the model to create realistic anatomical obstacles that physicians might face in actual surgical settings.
These simulators' design philosophy goes beyond straightforward anatomical imitation. The model improves three-dimensional spatial comprehension when fixed inside a clear acrylic box, giving students the opportunity to comprehend intricate vascular linkages from a variety of angles. With an all-encompassing approach to simulation, medical personnel can acquire vital skills in an immersive setting without endangering patients. With decades of advancements in medical 3D printing technology, these models' anatomical correctness guarantees that every vascular curve and aneurysmal bulge replicates actual clinical situations.
The Role of Physical Simulation in Medical Training
From cadaver-based learning and theoretical instruction alone, medical education has undergone tremendous change. These days, physical anatomical simulators play a major role in competency-based training programs at clinical skills centers, medical schools, and nursing institutions. By offering opportunities for repeatable, standardized practice that let students advance at their own speed, these models fill a significant vacuum in medical education. Synthetic simulators provide consistent anatomical presentations that facilitate methodical skill development, in contrast to cadaveric specimens, which are few and variable.
There is increasing pressure on training institutes to produce graduates who are clinically competent and capable of safely conducting sophisticated procedures on a cerebral model. In order to address this issue, neurovascular simulators provide for practical experience with interventional procedures such cerebral angiography, aneurysm coiling, and catheter navigation. Before moving on to supervised clinical practice, students can make mistakes, learn from them, and improve their technique in a controlled setting. This progression reduces the learning curve associated with high-risk procedures and contributes to improved patient outcomes when graduates enter professional practice.
Applications Across Multiple Healthcare Sectors
The versatility of neurovascular training models extends across diverse healthcare environments. These simulators help practicing doctors' ongoing professional growth as well as undergraduate medical education in academic medical institutes. They are used in surgical departments for preoperative planning, which enables interventional radiologists and neurosurgeons to practice complicated scenarios with patient-specific anatomical configurations. In addition to lowering operating time and complication rates, this preparation increases procedural confidence.
Research institutions leverage these models for biomechanical studies and device validation protocols. Anatomically precise testing platforms are necessary for medical device manufacturers to assess the performance of new stents, catheters, guidewires, or embolic materials prior to clinical trials. The cerebral model efficiently accomplishes this goal by offering reliable anatomical foundations for regulatory documentation and comparative testing. In order to guarantee that healthcare professionals at all levels remain proficient in crucial neurovascular interventions, government health organizations and emergency response training programs also include these simulators into disaster preparedness exercises and certification programs.
Benefits and Advantages of Cerebral Models for Clinical and Educational Use
Enhanced Learning Outcomes Through Realistic Practice
Educational research consistently demonstrates that hands-on simulation training produces superior learning outcomes compared to passive learning methods. Neurovascular models engage several sensory channels at once to promote active learning. Trainees gain cognitive comprehension of procedural workflows, physical familiarity with catheter handling, and visual awareness of anatomical landmarks. Stronger memory consolidation and skill retention are produced by this multimodal engagement, and this immediately improves clinical performance.
The realistic material qualities of silicone-based simulators greatly enhance the efficacy of training. Practitioners encounter resistance and feedback similar to real vascular tissue while using Trandomed's Shore 40A silicone models. The sensitive touch necessary for effective catheter navigation and device deployment is developed thanks to this genuine tactile response. By developing the haptic discrimination abilities necessary for safe interventional treatments, trainees learn to distinguish the minute variations between healthy artery walls and diseased abnormalities like aneurysms.
Risk Reduction and Patient Safety Improvements
In the delivery of modern healthcare, patient safety is the top priority. This need is immediately addressed by simulation-based training, which enables medical professionals to become competent before operating on real patients. Inadequate training or limited exposure to intricate anatomical variations may lead to medical blunders. Healthcare professionals can lower error rates in clinical settings by honing their problem-solving abilities and procedural confidence by practicing on models that mimic uncommon or difficult anatomical presentations.
Measurable increases in procedural outcomes on a cerebral model are reported by hospitals that use extensive simulation training programs. During fluoroscopy-guided treatments, surgical training laboratories employing high-fidelity neurovascular models report lower radiation exposure, shorter operation times, and fewer complications. These advancements show how skills from virtual settings are applied in real-world clinical settings. The ability to rehearse complex cases multiple times before entering the operating room provides clinicians with valuable experience that would otherwise require years of supervised practice to acquire.
Cost-Effectiveness and Training Efficiency
Although resources must be allocated for the initial purchase of high-quality simulation equipment, there are significant long-term economic advantages. Longer operation times, more radiation exposure, and higher incidence of complications during the learning curve are some of the hidden costs associated with traditional medical apprenticeship arrangements. This learning curve is greatly shortened by simulation training, which enables learners to become proficient faster and with fewer supervised clinical situations. This efficiency translates to reduced training costs per clinician and faster integration of new practitioners into productive clinical roles.
The cost-effectiveness of silicone-based models is further increased by their robustness and reusability. In contrast to biological specimens, which degrade quickly, synthetic simulators can endure hundreds of practice sessions before needing to be replaced. Training facilities can plan rigorous practice sessions without worrying about preservation standards or specimen availability. Since a single platform can be modified to depict various anatomical variations and clinical states, the necessity for a diversified inventory is eliminated by the capacity to create models according to individual training objectives.
Implementation Strategies and Case Studies of Cerebral Models in B2B Environments
Planning and Integration for Educational Institutions
The first steps in implementing neurovascular simulation programs successfully are thorough needs analysis and strategic planning. Medical schools and nursing colleges must align simulator selection with curriculum objectives, competency milestones, and accreditation requirements. Stakeholders from several areas, including anatomy, surgery, radiology, and simulation center operations, are involved in this process. Institutions can make sure that the models they choose promote particular educational aims rather just being underutilized capital equipment by clearly defining learning objectives and assessment criteria before to procurement.
Integration into current courses necessitates faculty development and careful scheduling. Traditional teaching techniques should be supplemented by simulation sessions, which offer practical reinforcement of theoretical ideas covered in readings and lectures. In addition to using models, faculty members need to be trained in performance evaluation, debriefing methods, and simulation pedagogy. Higher utilization rates and superior educational outcomes are attained by institutions that invest in extensive faculty development programs as opposed to those that merely buy equipment without providing the necessary infrastructure for deployment.
Clinical Department Adoption and Workflow Integration
Workflow integration and employee engagement present special implementation problems for hospital surgical training departments using a cerebral model. Programs that are successful present simulation training as a chance for professional growth rather than an extra strain on already overworked professionals. Building physician buy-in and ongoing involvement can be achieved by scheduling specific simulation sessions within protected time, providing continuing medical education credits, and showcasing quantifiable skill progress.
Clinical benefits of neurovascular simulation programs are demonstrated by case studies from specialist hospitals. Following the implementation of required simulation training utilizing anatomically correct models, one academic medical center observed a 35% decrease in procedural problems among interventional radiology fellows. After comprehensive simulation-based preparation for challenging cases, another institution reported lower fluoroscopy exposure and shorter average operation times. These results offer strong support for program growth and vindicate the investment in top-notch training infrastructure.
Research Laboratory and Device Testing Applications
Compared to educational institutions, biomedical research centers use neurovascular models differently, emphasizing device validation studies, biomechanical analysis, and experimental protocols. Models with accurate anatomical specifications and uniform material qualities that facilitate repeatable testing conditions are necessary for implementation in these contexts. Customization capabilities become particularly important for research applications, as investigators often require specific anatomical configurations to test particular hypotheses or evaluate device performance in defined scenarios.
Anatomically accurate models are used by medical device manufacturers to prove safety and efficacy prior to clinical trials during product development and regulatory testing. A crucial step in the product development process is the capacity to gather validation data, record performance metrics, and conduct standardized testing across several prototypes. Iterative design procedures are supported by Trandomed's quick manufacturing timeline of seven to ten days, which enables manufacturers to swiftly get models reflecting design alterations and do comparative testing that speeds up development cycles.
Conclusion
Neurovascular simulators are now essential instruments in clinical training, research, medical education, and device development. Modern cerebral models' anatomical precision, material authenticity, and customizability directly meet the changing needs of healthcare organizations looking to increase patient safety, training quality, and medical knowledge. Advanced materials, patient-specific modeling, and digital integration will all contribute to the further development of simulation technology, which will become more and more important in educating medical personnel about the intricacies of contemporary neurovascular care. Businesses that make deliberate investments in top-notch simulation infrastructure put themselves at the forefront of clinical excellence and medical education.
FAQs
Which particular processes can neurovascular simulators be used to practice?
Numerous interventional techniques, such as aneurysm coiling and tamponade, cerebral angiography, catheter navigation through convoluted arteries, stent deployment, thrombectomy treatments, and diagnostic imaging interpretation, are supported by neurovascular training models. These simulators' adaptability enables trainees to proceed from fundamental catheter manipulation skills to sophisticated interventional techniques, methodically developing competency prior to moving into supervised clinical practice.
In what ways do choices for personalization improve the efficacy of training?
Customization enables organizations to match simulators with particular learning goals, patient demographics, and clinical situations that are pertinent to their practice setting. Targeted training experiences that cater to specific learning objectives are made possible by the option to select aneurysm locations, sizes, and numbers. In order to ensure that trainees are ready for difficult situations when they occur, custom models can also reproduce complex pathological states or uncommon anatomical variants that they might not usually meet in clinical practice.
When choosing a supplier, what aspects should procurement teams take into account?
Critical evaluation criteria include anatomical accuracy validated through comparison with medical imaging data, material quality and durability, customization capabilities, production timelines, customer support infrastructure, and vendor experience in the medical simulation field. Procurement teams should assess the technical proficiency of the supplier's support staff, examine case studies from comparable organizations, and seek product samples. Simple transactional purchases are frequently less valuable than long-term vendor partnerships that involve continuous consultation and product development cooperation.
How long do models made of silicone usually endure when used frequently?
Excellent endurance is demonstrated by high-quality medical-grade silicone models, which usually endure hundreds of practice sessions before exhibiting noticeable wear. The amount of use, appropriate handling, and storage conditions all affect the actual lifespan. Compared to models used for sporadic advanced training or preoperative planning, models utilized in high-volume training programs might need to be replaced more regularly. Model longevity and training efficacy are maintained by proper maintenance, which includes routine cleaning and suitable storage.
Partner with a Trusted Cerebral Model Manufacturer for Your Training Programs
Trandomed is prepared to assist your organization's simulation training efforts with cutting-edge neurovascular models that combine outstanding anatomical correctness, adaptability for customisation, and demonstrated durability. Our cerebral model solutions, supported by more than 20 years of specialist experience in medical 3D printing technology, are used by hospitals, medical institutions, research labs, and device makers worldwide. We maintain quick manufacturing schedules, accept special specifications without charging design fees, and offer thorough technical assistance both during and after implementation. Get in touch with jackson.chen@trandomed.com right now to talk about your unique training needs and learn how our anatomically accurate simulators can improve your clinical results and educational initiatives.
References
Spiotta, A.M., Rasmussen, P.A., Masaryk, T.J., Benzel, E.C., and Schlenk, R. (2013). "Simulated diagnostic cerebral angiography in neurosurgical training: A pilot program." Journal of NeuroInterventional Surgery, 5(4), 376-381.
Mashiko, T., Otani, K., Kawano, R., Konno, T., Kaneko, N., Ito, Y., and Watanabe, E. (2015). "Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping." World Neurosurgery, 83(3), 351-361.
Bambakidis, N.C., Selman, W.R., and Sloan, A.E. (2013). "Surgical rehearsal platform: Potential uses in microsurgery." Neurosurgery, 73(Suppl 1), 122-126.
Ryan, J.R., Almefty, K.K., Nakaji, P., and Frakes, D.H. (2016). "Cerebral aneurysm clipping surgery simulation using patient-specific 3D printing and silicone casting." World Neurosurgery, 88, 175-181.
Waran, V., Narayanan, V., Karuppiah, R., Owen, S.L., and Aziz, T. (2014). "Utility of multimaterial 3D printers in creating models with pathological entities to enhance the training experience of neurosurgeons." Journal of Neurosurgery, 120(2), 489-492.
Anderson, J.R., Thompson, W.L., Alkattan, A.K., Diaz, O., Klucznik, R., Zhang, Y.J., Britz, G.W., Grossman, R.G., and Karmonik, C. (2016). "Three-dimensional printing of anatomically accurate, patient specific intracranial aneurysm models." Journal of NeuroInterventional Surgery, 8(5), 517-520.