Clinical and Educational Uses of the Circle of Willis Brain Model
2026-01-15 17:22:35
In neurovascular education and clinical training, the circle of Willis brain model is a significant accomplishment. When artery disease or damage occurs, this unique simulation tool protects against ischemia events by simulating the complex arterial network that supplies collateral blood flow between the anterior and posterior brain circulations. High-fidelity cerebrovascular models have become essential resources for clinical training departments, research labs, and medical facilities throughout the United States. These anatomically accurate instruments give surgical teams the ability to practice difficult operations, let medical trainees see pathological abnormalities, and give device manufacturers realistic testing platforms that help close the knowledge gap between theory and practice.
Understanding the Anatomy and Function of the Circle of Willis
Situated in the interpeduncular cistern of the subarachnoid space at the base of the brain, the circle of Willis is a magnificent hexagonal ring of arteries. This arterial circle is the main collateral circulation system in the brain, encircling important structures such as the optic chiasm and the pituitary gland's infundibulum. Recognizing the protective role of the circle of Willis is the first step towards understanding why it is so crucial to brain function. When one feeding vessel is compromised due to stenosis, thrombosis, or aneurysm, this anatomical configuration allows blood to be rerouted from other sources, potentially preventing catastrophic neurological damage.
Essential Components of the Cerebrovascular Circle
Several crucial parts of the entire vascular circle cooperate to sustain brain perfusion. The anterior part of the circle is formed by the anterior communicating artery connecting the anterior cerebral arteries at their A1 segments, which split off from the internal carotid arteries. Before splitting off to form the anterior and middle cerebral arteries, the internal carotid arteries contribute at their distal ends, or the carotid terminus. The basilar artery, which is created by the union of vertebral arteries arriving through the foramen magnum, gives rise to the posterior cerebral arteries at their P1 segments, which are part of the posterior circulation. This protective vascular ring is completed by the posterior connecting arteries on either side, which connect the anterior and posterior circulations. It's interesting to note that studies show that about 20 to 25 percent of people have a full circle of Willis without any missing or hypoplastic elements, therefore anatomical variance is more common than uncommon.
Clinical Significance of Anatomical Variations and Pathologies
Variations in the cerebrovascular circle's anatomy have a significant clinical impact on how patients fare during neurovascular events. When primary vessels become blocked, the reduced collateral flow capacity caused by hypoplastic or missing communication arteries increases the risk of stroke. Within the circle, aneurysms commonly form at arterial connections, especially at bifurcation locations where hemodynamic stress is concentrated. In areas such as the M1 segment of the middle cerebral artery, stenotic lesions can seriously impair downstream perfusion. Standard textbook diagrams are unable to fully address the educational opportunities created by these diseased states. Medical students are exposed to the complexity they will face in real-world clinical practice through sophisticated cerebrovascular simulation models that include anatomical variations, multiple aneurysm locations, and stenosis lesions. This helps them identify warning signs and develop appropriate interventions.
Comparing Different Types of Circle of Willis Brain Models for Optimal Educational and Clinical Use
When choosing cerebrovascular simulation technologies like the circle of willis brain model, medical institutions have a wide range of alternatives, from simple two-dimensional diagrams to intricate three-dimensional copies with pathological aspects. These models differ significantly in terms of material composition, structural complexity, and functional capabilities, which affects their appropriateness for particular therapeutic and educational purposes. To find solutions that maximize training value while staying within cost restrictions, procurement experts must negotiate these disparities.
Material Selection and Tactile Realism
Model performance during practical training sessions is significantly impacted by the decision between silicone and plastic materials. For anatomical illustration in classroom settings where students must visualize spatial relationships, rigid plastic models are appropriate since they are durable and hold their shape even after frequent handling. Nevertheless, the compliance required for the use of interventional devices is absent from these models. The tactile feedback provided by silicone-based models, especially those made with Shore 40A durometer silicone, is tissue-like and closely resembles the sensation of passing catheters through real blood arteries. When teaching interventional neurologists and neurosurgeons methods like aneurysm coiling, where catheter manipulation calls for realistic resistance and flexibility, this material feature becomes essential. Because silicone construction is more realistic, trainers can improve their technique and muscle memory, which immediately correlates to patient care situations.
Structural Complexity and Pathological Features
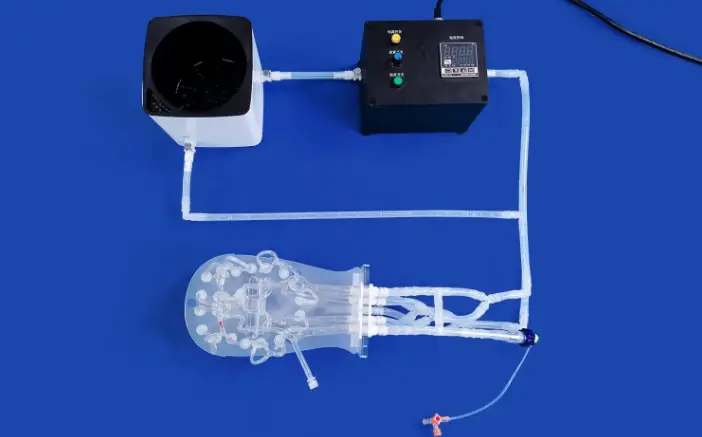
Basic anatomical models serve as fundamental teaching tools in medical schools when students first study cerebrovascular anatomy. They show normal vascular architecture free of disease disorders. Single pathologies, like an isolated aneurysm, may be included in intermediate models, offering targeted teaching possibilities for particular procedures. Advanced simulation platforms create thorough training settings by combining several pathological aspects at once, such as stenotic segments, different aneurysm diameters and locations, and realistic vascular tortuosity. This advanced category is best represented by Trandomed's Circle of Willis Aneurysm II model (Product No. SJL001D), which includes the stenosis lesioned M1 segment of the right middle cerebral artery along with three separate aneurysms on the basilar artery, the ophthalmic segment of the left carotid artery, and the left middle cerebral artery. This degree of pathological information enables surgical teams to practice complicated patients prior to entering the operating room by simulating cerebral thrombectomy and aneurysm tamponade procedures.
Integration of Supporting Anatomical Structures
The degree to which models help various training objectives depends on whether neighboring neuroanatomical structures are included or excluded. Learners who need to become proficient in artery identification and catheter navigation will profit from isolated vascular models, which concentrate all attention on arterial linkages and diseases. Trainees can better grasp anatomical links related to surgical techniques and problem avoidance by using comprehensive models that include the brainstem, cranial base, and surrounding neural tissue. Knowing how the circle of Willis interacts to nearby structures is essential for safe technique execution when planning endoscopic or open surgical procedures. The choice of structural inclusion should be in line with the particular training competencies and curricular objectives that each institution is developing.
Practical Guide to Procuring Circle of Willis Brain Models for B2B Clients
When purchasing cerebrovascular simulation tools such as the circle of willis brain model, procurement specialists must weigh a number of factors to ensure models that provide the best return on investment for instruction. Successful purchase decisions that meet institutional training objectives are influenced by a number of factors, including quality evaluation, customisation capabilities, supplier reliability, and total cost of ownership.
Quality Criteria and Validation Standards
Effective medical simulation models are built on anatomical accuracy, which must be confirmed against recognized medical imaging data. Superior manufacturers use reverse three-dimensional reconstruction technology to assure accurate replication of vascular anatomy and base their designs on large genuine human CT and MRI datasets. Consistency and detail replication are affected by the manufacturing process itself; complicated interior geometries and smooth luminal surfaces that are impossible with traditional manufacturing are made possible by proprietary three-dimensional printing molding technology. Procurement teams should ask for documentation about the anatomical data sources utilized for model development, manufacturing quality control procedures, and validation test outcomes when assessing possible vendors. Purchase justification is strengthened by the added credibility of models that have been used in published research studies or approved by medical specialty groups.
Customization Options and Patient-Specific Modeling
Although standard anatomical models are useful for general education, some training scenarios benefit from specially designed configurations that take into account unique institutional requirements or uncommon disease presentations. Customization services are provided by progressive manufacturers, who can alter aneurysm number, size, and location to meet unique needs. Targeted training situations can be created by incorporating additional cerebrovascular pathologies such as arteriovenous malformations, varying degrees of stenosis, and cerebral embolism. Advanced customization options also include patient-specific modeling, which allows for the actual replication of institutional CT, CAD, STL, STP, or STEP format data files for preoperative planning of especially complicated situations. When surgical teams encounter uncommon anatomical configurations that call for practice prior to patient intervention, this skill comes in quite handy. Financial obstacles that could ordinarily keep institutions from obtaining customized simulation solutions for particular training requirements are eliminated by Trandomed's acceptance of customization requests without imposing design fees.
Supplier Evaluation and Procurement Channels
Choosing trustworthy suppliers guarantees consistent product quality, prompt customer service, and predictable fulfillment dates that coincide with training program and academic calendars. Reputable producers with a wealth of medical simulation experience show a stronger comprehension of clinical needs and educational applications. distinct departments within healthcare organizations can have distinct simulation preferences and budget levels thanks to companies that keep a variety of material inventories. Procurement planning is impacted by lead time considerations. While longer manufacturing timelines necessitate advance planning, models with seven to ten day production schedules allow responsive ordering that adapts to changing curriculum needs. Tracking visibility and delivery dependability are provided by international shipment operations employing reputable carriers like FedEx, DHL, EMS, UPS, and TNT. Bank transfer agreements provide security for both parties. In order to safeguard institutional investments throughout an extended service life, procurement experts should build partnerships with suppliers who offer full after-sales support, including technical advice, replacement part availability, and warranty coverage.
Conclusion
As healthcare institutions place a greater emphasis on competency-based education and patient safety measures, high-fidelity cerebrovascular simulation models have evolved from educational luxury to training essentials. Unrivaled chances for neurovascular skill development are offered by the circle of Willis brain model, which offers secure settings where trainees can gain competence prior to treating patients. Premium simulation solutions differ from basic teaching tools in terms of anatomical accuracy, disease complexity, material realism, and customisation capabilities. Procurement specialists who thoroughly assess these variables put their organizations in a position to provide excellent training results, which immediately increase clinical performance and the standard of patient care.
FAQs
By what standards are cerebrovascular simulation models considered to be of high quality?
High-quality cerebrovascular models use materials that offer realistic tactile feedback when manipulating devices, incorporate clinically relevant pathological features, maintain structural integrity through repeated training sessions, and exhibit anatomical accuracy confirmed against medical imaging data. Better models are produced utilizing cutting-edge methods that replicate the smooth luminal surfaces and fine vascular features necessary for realistic catheter navigation.
What effects does material choice have on the lifespan and usability of models?
Training realism and product longevity are both significantly impacted by material selection. Realistic interventional device practice is made possible by silicone formulations such as Shore 40A, which offer tissue-like compliance that replicates real vascular properties. When properly maintained, these materials can survive repeated catheter insertion and manipulation without deteriorating. Although rigid plastics have a longer lifespan for demonstrations, they don't have the haptic qualities needed for practical procedural instruction. Training goals and expected use cases determine the best content.
What procedure must to be followed by organizations when placing orders for personalized models?
The first step in customization is the creation of a thorough specification that includes the desired clinical characteristics, anatomical variations, size specifications, and educational goals. For patient-specific modeling, institutions can supply medical imaging data files in CT, CAD, STL, STP, or STEP formats. Manufacturers submit design concepts for approval after reviewing specifications to ensure viability. Production schedules usually surpass those of normal models, necessitating prior planning. Trandomed makes unique models affordable for organizations with particular training requirements by providing customisation without design cost fees.
Can educational and device testing applications be supported by these models?
Advanced neurovascular models are useful for both goals. Anatomy education, procedure practice, and competency evaluation for medical students, residents, and practicing physicians are examples of educational applications. At the same time, these models give makers of medical devices that are creating neuro-interventional tools including stents, catheters, flow diverters, and embolic materials realistic testing platforms. Valid gadget performance evaluation and design verification testing are also made possible by the anatomical precision and material qualities that help learners.
Partner with a Trusted Circle of Willis Brain Model Manufacturer
To learn more about our extensive neurovascular simulation portfolio, Trandomed extends an invitation to procurement specialists from medical schools, hospital training departments, research labs, and product development firms. The anatomical accuracy, pathological complexity, and material realism that set successful training aids apart from simple anatomical displays are all provided by our Circle of Willis Aneurysm II model (Product No. SJL001D). As a supplier of circle of willis brain model products with more than two decades of specialist experience, we offer unparalleled knowledge to every standard product and bespoke configuration. We accept requests for patient-specific modeling projects, large institutional orders, and advice on the best simulation options for your unique learning goals. To explore customization options, obtain comprehensive product specs, or schedule demonstrations that highlight how our models may improve your neurovascular training programs, get in touch with jackson.chen@trandomed.com.
References
Alpers, B.J., Berry, R.G., & Paddison, R.M. (1959). Anatomical studies of the circle of Willis in normal brain. Archives of Neurology and Psychiatry, 81(4), 409-418.
Hartkamp, M.J., van Der Grond, J., van Everdingen, K.J., Hillen, B., & Mali, W.P. (1999). Circle of Willis collateral flow investigated by magnetic resonance angiography. Stroke, 30(12), 2671-2678.
Krabbe-Hartkamp, M.J., van der Grond, J., de Leeuw, F.E., de Groot, J.C., Algra, A., Hillen, B., Breteler, M.M., & Mali, W.P. (1998). Circle of Willis: morphologic variation on three-dimensional time-of-flight MR angiograms. Radiology, 207(1), 103-111.
Lindegaard, K.F., Bakke, S.J., Aaslid, R., & Nornes, H. (1986). Doppler diagnosis of intracranial artery occlusive disorders. Journal of Neurology, Neurosurgery, and Psychiatry, 49(5), 510-518.
Rinaldo, L., McCutcheon, B.A., Murphy, M.E., Bydon, M., Rabinstein, A.A., Lanzino, G., & Cloft, H.J. (2017). Relationship of circle of Willis configuration to aneurysm formation and outcome. Journal of Stroke and Cerebrovascular Diseases, 26(10), 2181-2186.
van Raamsterdam, M.M., Meijer, F.J., Bastiaansen, J.A., Prokop, M., & Bor, A.S. (2015). Accuracy of 3D CT angiography in visualizing the anatomical variation of the circle of Willis. European Radiology, 25(7), 1910-1918.








