Endovascular Intervention Trainer vs Traditional Training Models: Which Prepares You Better?
2025-08-18 09:00:02
When it comes to preparing for complex endovascular procedures, the choice of training model can significantly impact a practitioner's skill development and confidence. Endovascular intervention trainers have emerged as a revolutionary alternative to traditional training methods, offering unparalleled realism and hands-on experience. These advanced simulators provide a safe, controlled environment for mastering intricate techniques without patient risk.
While traditional models have long been the standard, endovascular trainers offer distinct advantages in anatomical accuracy, real-time feedback, and the ability to replicate diverse pathologies. The immersive experience they provide allows trainees to develop muscle memory and decision-making skills that closely mirror real-world scenarios. However, the effectiveness of any training model ultimately depends on how it's integrated into a comprehensive educational program. Let's explore the key differences between these approaches to determine which better equips future vascular specialists for the challenges that lie ahead.
What Are the Key Differences in Anatomical Realism and Device Response?
Fidelity of Vascular Structures
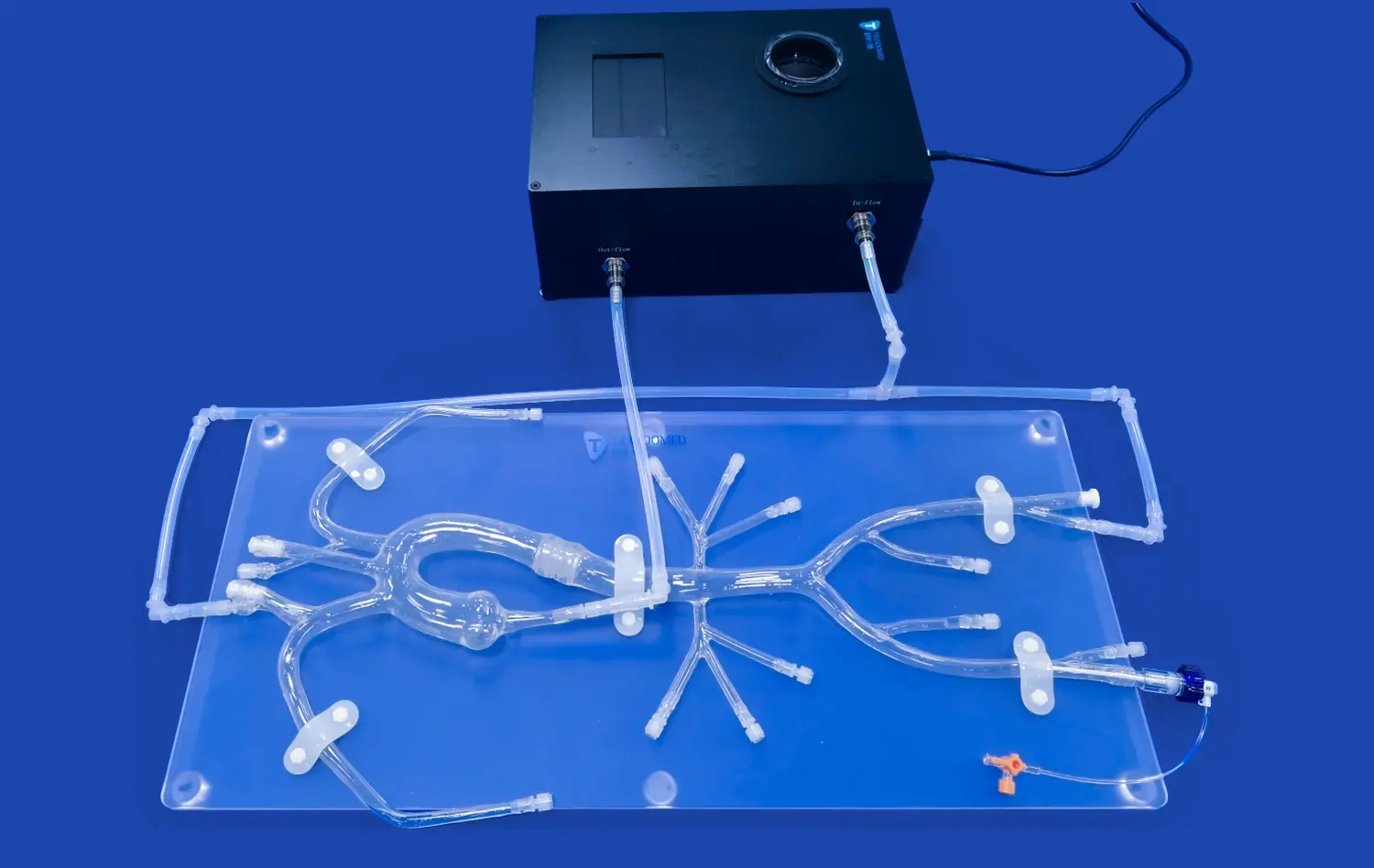
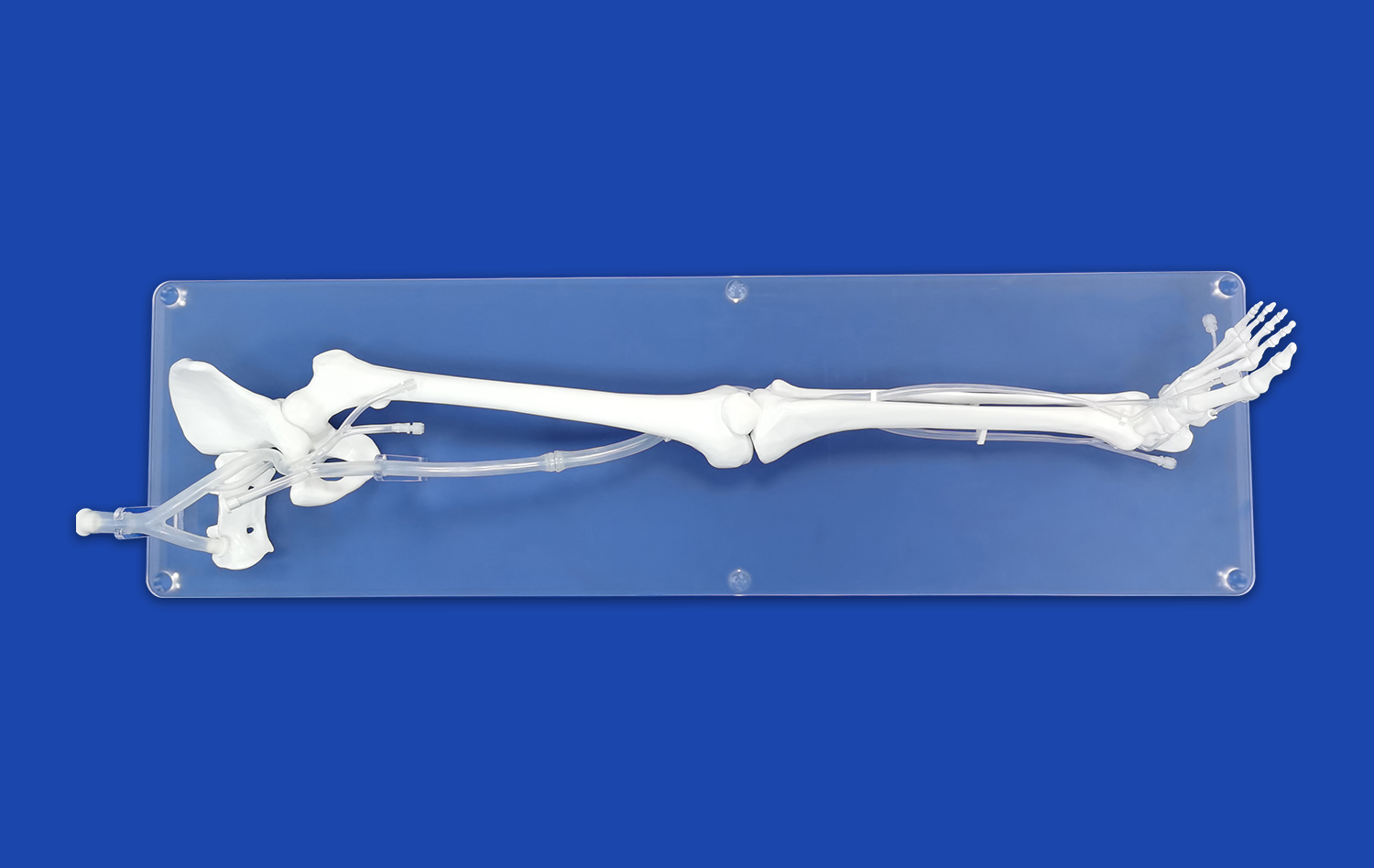
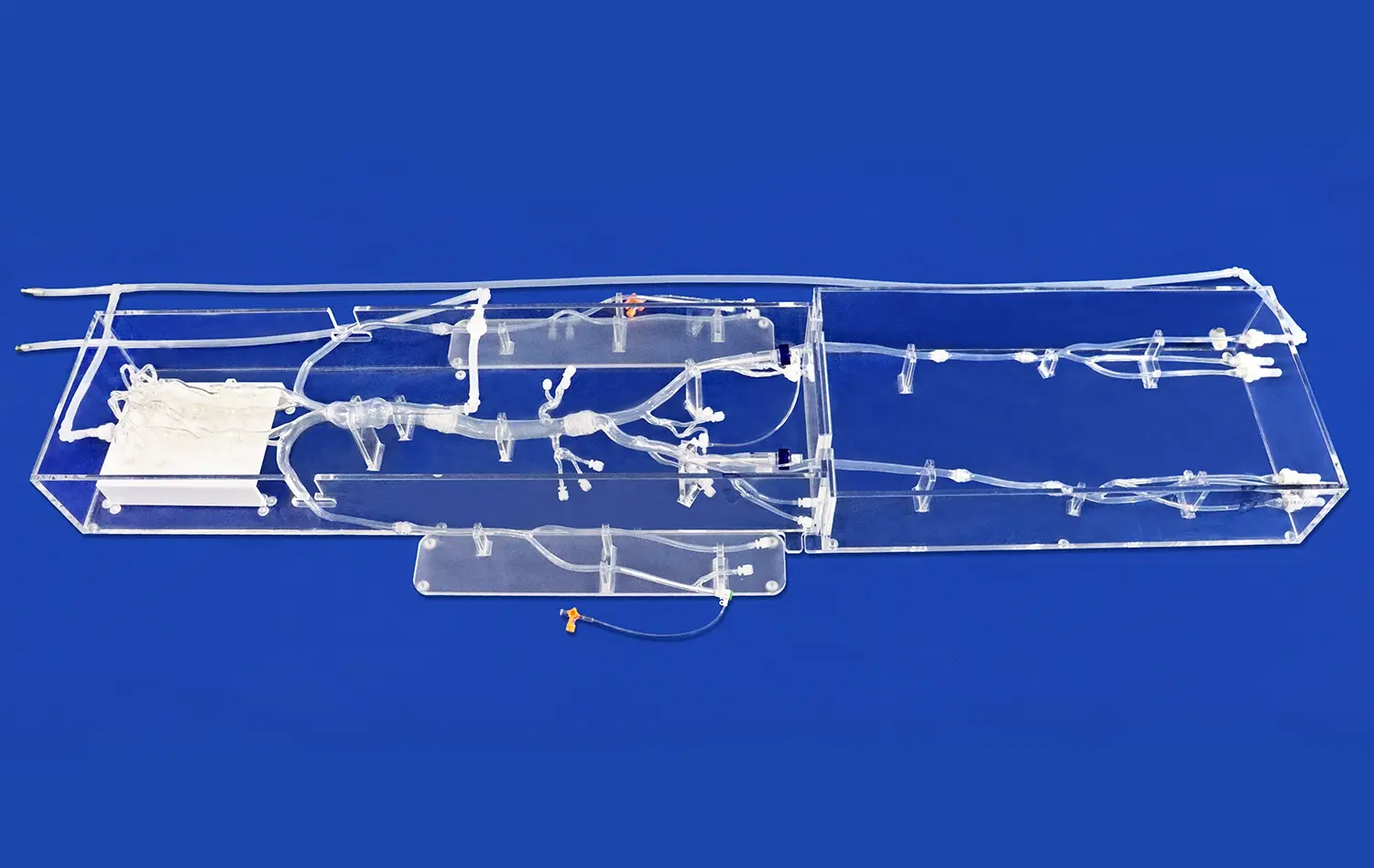
Endovascular intervention trainers excel in replicating the intricate network of blood vessels with remarkable precision. These simulators utilize advanced 3D printing and silicone molding techniques to create anatomically correct models based on real patient data. The result is a highly realistic representation of the vascular system, complete with accurate vessel diameters, branching patterns, and tortuosity.
Traditional bench models, while useful for basic skill acquisition, often lack the nuanced details found in human anatomy. They may oversimplify vessel geometry or omit critical anatomical variations, potentially leaving trainees underprepared for the complexities encountered in actual patients.
Tactile Feedback and Haptics
One of the most significant advantages of modern endovascular intervention trainers is their ability to provide realistic tactile feedback. These simulators incorporate materials that closely mimic the elasticity and friction coefficients of human blood vessels. This allows trainees to experience the subtle resistance and "feel" of navigating catheters and guidewires through the vasculature.
In contrast, traditional models often use rigid materials that fail to capture the delicate interactions between devices and vessel walls. This discrepancy can lead to a disconnect between training experiences and real-world procedures, potentially hindering the development of fine motor skills crucial for successful interventions.
Dynamic Response to Interventions
Advanced endovascular trainers feature dynamic simulation capabilities that respond in real-time to trainee actions. For instance, when deploying a stent or performing angioplasty, the simulated vessel will react accordingly, showing changes in blood flow or potential complications like dissection or perforation.
Traditional static models lack this interactivity, limiting their ability to prepare trainees for the dynamic nature of endovascular procedures. The absence of immediate feedback on intervention outcomes can hinder the development of critical decision-making skills and procedural finesse.
Comparative Outcomes in Training for Complex Vascular Pathologies
Replication of Diverse Pathological Conditions
Endovascular intervention trainers shine in their ability to simulate a wide array of vascular pathologies. From intricate cerebral aneurysms to complex aortic dissections, these simulators can be customized to represent virtually any vascular condition. This versatility allows trainees to gain experience with rare and challenging cases they may not encounter frequently during their clinical rotations.
Traditional training models are often limited in the range of pathologies they can accurately represent. While they may be suitable for practicing basic techniques, they struggle to capture the nuances of complex vascular diseases, potentially leaving gaps in a trainee's preparedness for advanced interventions.
Procedural Complexity and Skill Progression
Modern endovascular intervention trainers offer scalable difficulty levels, allowing educators to tailor the training experience to the learner's skill level. Novices can start with straightforward cases and gradually progress to more challenging scenarios as their proficiency improves. This structured approach facilitates a smoother learning curve and builds confidence incrementally.
Traditional models typically provide a more static learning experience. While they may be effective for teaching fundamental skills, they often lack the flexibility to accommodate the diverse learning needs of trainees at different stages of their careers. This limitation can result in a less efficient and potentially frustrating learning process for some practitioners.
Multi-disciplinary Team Training
Endovascular intervention trainers excel in facilitating team-based learning scenarios. These simulators can incorporate multiple roles, allowing trainees to practice not only as primary operators but also as assistants, nurses, or technicians. This collaborative approach mirrors the real-world environment of an interventional suite, fostering better communication and coordination among team members.
Traditional bench models are generally more focused on individual skill development and may not provide the same opportunities for team-based training. This limitation can leave trainees less prepared for the collaborative nature of complex endovascular procedures, where effective teamwork is often crucial for success.
Decision-Making Under Simulated Risk: Trainer vs Traditional Bench Models
Real-time Complication Management
One of the most valuable aspects of advanced endovascular trainers is their ability to simulate procedural complications in real-time. Trainees can experience scenarios such as vessel dissection, embolization, or contrast-induced nephropathy, requiring them to make quick decisions and take appropriate actions. This feature helps develop critical thinking skills and prepares practitioners for high-stress situations they may encounter in clinical practice.
Traditional bench models typically lack the capability to simulate dynamic complications. While they may allow for practice of basic techniques, they do not challenge trainees to respond to unexpected events or make rapid decisions under pressure. This limitation can leave practitioners less prepared for managing complications when they arise in real patients.
Quantitative Performance Metrics
Modern endovascular intervention trainer often incorporates sophisticated tracking systems that provide objective measurements of trainee performance. These metrics can include procedure time, fluoroscopy usage, contrast volume, and accuracy of device placement. Such data allows for detailed performance analysis, enabling both trainees and instructors to identify areas for improvement and track progress over time.
Traditional endovascular intervention trainer models typically rely on subjective assessments or basic time measurements, which may not capture the nuances of procedural efficiency and safety. The lack of comprehensive performance metrics can make it challenging to provide targeted feedback and assess a trainee's readiness for independent practice accurately.
Simulated Patient Outcomes
Advanced endovascular trainers can simulate long-term patient outcomes based on the decisions made during the procedure. This feature allows trainees to see the potential consequences of their actions beyond the immediate intervention. For example, they might observe the impact of incomplete stent apposition on restenosis rates or the effects of embolic protection device usage on stroke risk.
Traditional bench models are limited in their ability to demonstrate the downstream effects of procedural decisions. This shortcoming can result in a narrower perspective on the overall impact of endovascular interventions, potentially leading to a focus on short-term technical success rather than long-term patient outcomes.
Conclusion
While both endovascular intervention trainers and traditional models have their place in medical education, the advanced capabilities of modern simulators offer distinct advantages in preparing practitioners for the complexities of real-world procedures. The anatomical realism, dynamic responses, and diverse pathology simulations provided by endovascular trainers create a more comprehensive and immersive learning experience.
These systems enable trainees to develop not only technical skills but also critical decision-making abilities and team coordination - essential components for success in the challenging field of endovascular interventions.
Contact us
Are you ready to elevate your endovascular training program with cutting-edge simulation technology? Trandomed offers state-of-the-art endovascular intervention trainers that provide unparalleled realism and versatility. Our customizable solutions can be tailored to meet the specific needs of your institution, ensuring your trainees are well-prepared for the challenges of modern vascular care.
To learn more about how our advanced simulators can enhance your training outcomes, contact us at jackson.chen@trandomed.com. Take the next step in revolutionizing your endovascular education today!
References
1. Chaer, R. A., et al. (2019). "Simulation in vascular surgery: A systematic review and meta-analysis." Journal of Vascular Surgery, 70(4), 1379-1389.
2. Gould, D., et al. (2017). "Virtual reality simulation for the operating room: Proficiency-based training as a paradigm shift in surgical skills training." Annals of Surgery, 265(6), 1042-1050.
3. Lineberry, M., et al. (2018). "The impact of patient-specific vascular models in planning endovascular aortic repair." Journal of Vascular Surgery, 67(4), 1168-1174.
4. Nesbitt, C., et al. (2020). "Endovascular skills training and assessment." British Journal of Surgery, 107(8), e131-e141.
5. Rolls, A. E., et al. (2016). "A systematic review of 3-D printing in cardiovascular and interventional radiology." Cardiovascular and Interventional Radiology, 39(8), 1041-1055.
6. Willems, M. C., et al. (2018). "Effectiveness of endovascular simulation training: A systematic review." Journal of Vascular Surgery, 67(4), 1330-1339.e1.
1_1732869849284.webp)