In the realm of neurosurgical training, the advent of realistic aneurysm models has revolutionized how medical professionals hone their skills. These sophisticated simulators, such as the Intracranial Vascular with Aneurysm Model (SJX011), offer unparalleled opportunities for hands-on practice in a risk-free environment. By replicating the intricate anatomy of cerebral vasculature, complete with lifelike aneurysms, these models enable surgeons to refine their techniques in aneurysm detection, intervention, and surgical planning. The ability to repeatedly practice complex procedures like endovascular coiling and aneurysm clipping on anatomically accurate models significantly enhances clinical competence. This advancement in medical simulation not only improves surgical accuracy but also contributes to better patient outcomes by allowing medical professionals to master neurovascular procedures through repetitive, risk-free training.
How Do Simulation Models Improve Surgical Accuracy?
Anatomical Precision in Training
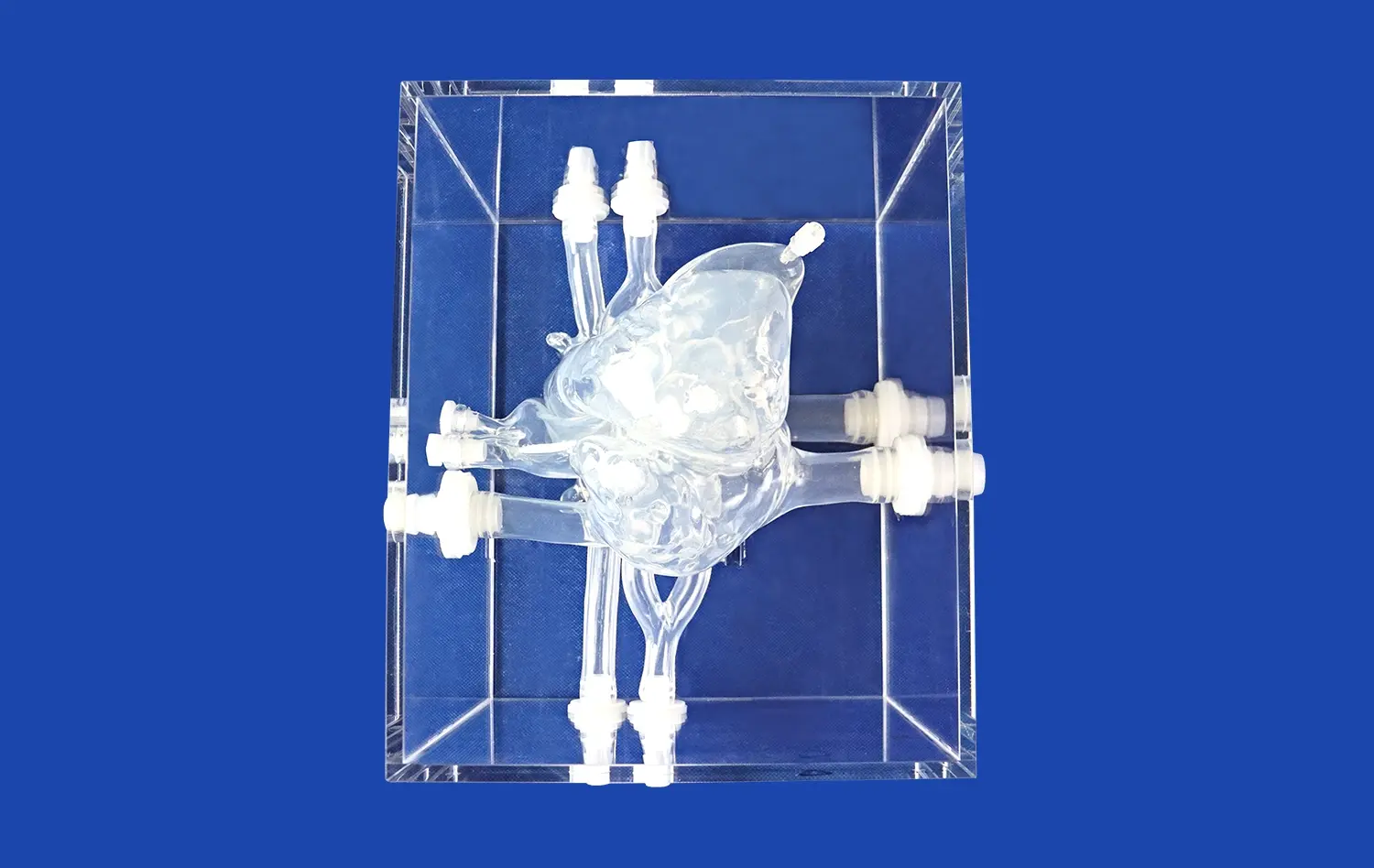
Simulation models, particularly those designed for aneurysm treatment, offer an unprecedented level of anatomical accuracy. The Intracranial Vascular with Aneurysm Model meticulously replicates the complex structure of cerebral blood vessels, including the anterior cerebral artery (ACA), middle cerebral artery (MCA), and the tortuous internal carotid artery. This precise representation allows neurosurgeons to familiarize themselves with the intricate vasculature they will encounter in real surgical scenarios.
The inclusion of four distinct aneurysms on the internal carotid artery further enhances the model's utility. These varied aneurysm formations provide diverse training scenarios, enabling surgeons to practice different approaches and techniques. The replaceable aneurysm lesion on the MCA adds another layer of versatility, allowing for the simulation of various pathological conditions.
Realistic Tissue Response
Advanced aneurysm models are engineered to mimic the tactile feedback of real tissue. This realistic tissue response is crucial for improving surgical accuracy. As surgeons manipulate instruments within the model, they experience sensations similar to those encountered in actual procedures. This tactile realism helps in developing the fine motor skills necessary for delicate neurovascular interventions.
The ability to practice aneurysm tamponade operations on these models further enhances this realism. Surgeons can experience the nuances of applying pressure to control bleeding, a critical skill in aneurysm surgery. This hands-on experience with lifelike tissue response significantly contributes to improved surgical precision and confidence.
Visualization and Spatial Awareness
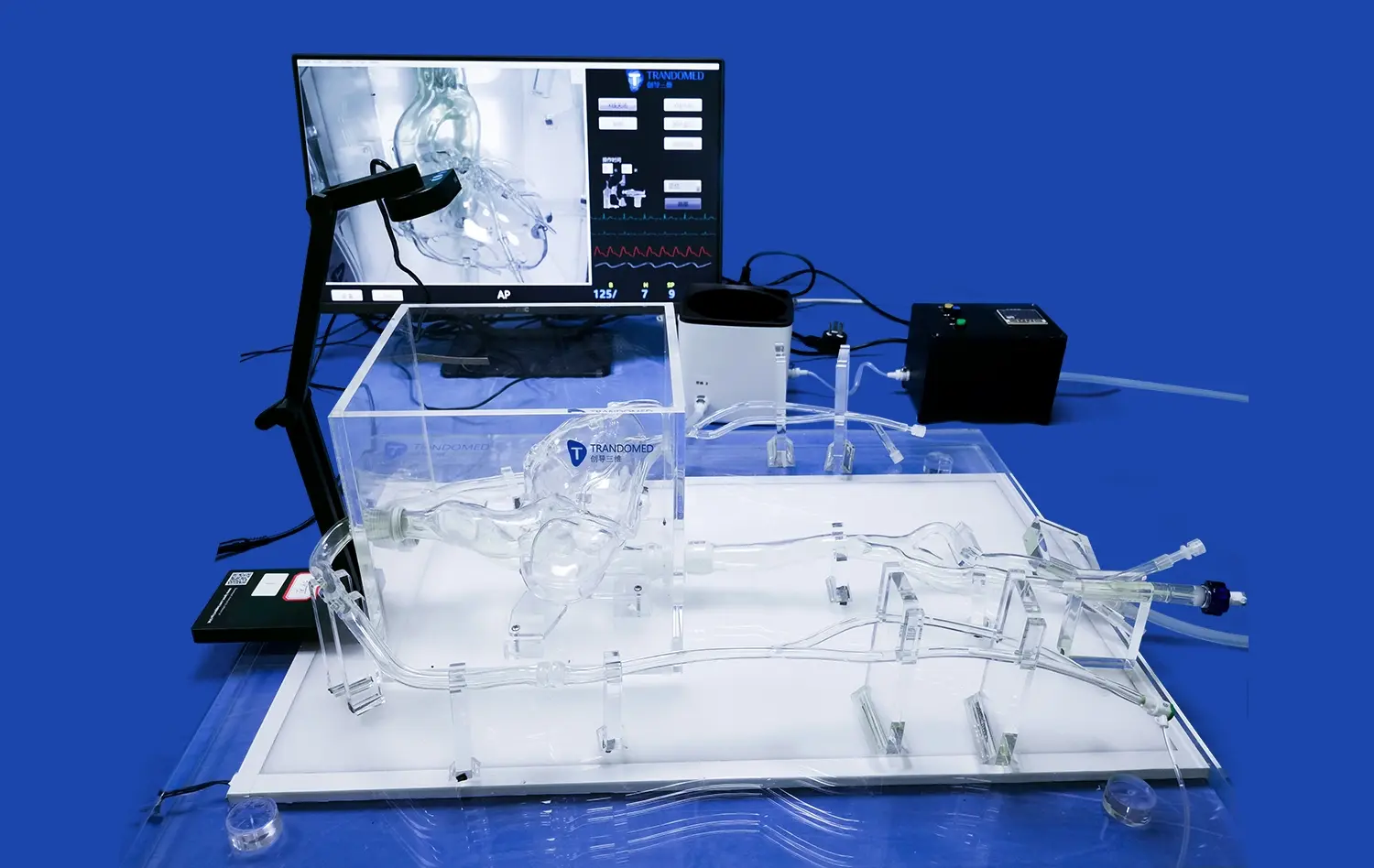
Aneurysm models provide excellent visualization of the surgical field, akin to what surgeons would see during an actual procedure. This clear view of the vascular structures and aneurysms helps in developing spatial awareness within the confined space of the cranium. Surgeons can practice maneuvering instruments around delicate structures, improving their ability to navigate complex anatomical landscapes.
Moreover, these models often allow for the simulation of various imaging techniques used in neurosurgery. This feature enables practitioners to correlate visual and tactile information with imaging data, enhancing their interpretative skills and surgical planning abilities. The improved spatial awareness and visualization skills directly translate to increased surgical accuracy in real-world scenarios.
Practicing Clipping and Coiling in a Risk-Free Setting
Mastering Aneurysm Clipping Techniques
Aneurysm clipping is a critical neurosurgical procedure that requires immense precision and skill. Realistic aneurysm models provide an ideal platform for mastering this technique without the pressure of operating on a live patient. Surgeons can practice placing clips at various angles and positions, learning to secure the aneurysm neck effectively while preserving blood flow in adjacent vessels.
The models allow for repetitive practice of clip placement, enabling surgeons to develop muscle memory and refine their techniques. They can experiment with different types of clips and approaches, understanding how each decision affects the overall outcome. This risk-free environment encourages exploration and innovation, potentially leading to the development of new and improved clipping strategies.
Perfecting Endovascular Coiling Skills
Endovascular coiling, a less invasive alternative to clipping, also benefits significantly from simulation training. Aneurysm models designed for this purpose often include access points that mimic real vascular entry sites. Practitioners can hone their skills in navigating catheters through complex vascular networks, reaching the target aneurysm with minimal disruption to surrounding structures.
The models allow for the practice of coil deployment within the aneurysm sac. Surgeons can learn to pack coils efficiently, ensuring proper aneurysm occlusion while avoiding complications like coil herniation. The ability to repeatedly perform these delicate maneuvers in a controlled setting greatly enhances the surgeon's proficiency and confidence in real-world procedures.
Complication Management and Problem-Solving
Perhaps one of the most valuable aspects of practicing on aneurysm models is the opportunity to encounter and manage complications in a controlled environment. Instructors can simulate various challenges, such as aneurysm rupture during clipping or coil migration during endovascular procedures. This allows trainees to develop critical problem-solving skills and quick decision-making abilities without risking patient safety.
By facing these simulated complications, surgeons learn to remain calm under pressure and develop strategies to address unexpected issues. They can practice emergency maneuvers and learn to adapt their approach in real-time, skills that are invaluable in the high-stakes environment of neurosurgery. This aspect of training significantly contributes to reducing procedural risks and improving patient outcomes in actual surgical scenarios.
Repetitive Training for Mastery of Neurovascular Procedures
Developing Muscle Memory and Procedural Fluency
The path to mastery in neurovascular procedures is paved with repetition. Aneurysm models facilitate this crucial aspect of skill development by allowing for unlimited practice sessions. Through repeated performance of techniques like clipping and coiling, surgeons develop muscle memory – the ability to perform complex maneuvers with automaticity and precision.
This repetitive training on anatomically accurate models helps in ingraining the correct procedural steps, making them second nature. As surgeons progress, they become more fluid in their movements, reducing procedure times and minimizing the risk of errors. The development of this procedural fluency is essential for handling the high-pressure situations often encountered in neurosurgical interventions.
Customized Learning Paths and Skill Progression
Aneurysm models offer the flexibility to create customized learning paths for trainees at different skill levels. Novice surgeons can start with basic aneurysm configurations and gradually progress to more complex scenarios. The ability to adjust the number, size, and location of aneurysms in these models, as offered by companies like Trandomed, allows for a tailored learning experience.
This customization enables a structured approach to skill development. Trainees can systematically tackle increasingly challenging cases, building confidence and competence along the way. The ability to track progress and identify areas for improvement through repeated trials on these models provides valuable feedback for continuous skill enhancement.
Team Training and Collaborative Learning
Neurovascular procedures often involve a team of medical professionals working in concert. Aneurysm models provide an excellent platform for team training exercises. Multiple team members can practice their roles simultaneously, improving communication and coordination in a simulated operating room environment.
These collaborative training sessions help in developing a shared understanding of procedural nuances and potential complications. They allow teams to establish efficient workflows and practice handoffs, crucial elements in successful neurosurgical interventions. The repetitive nature of these team exercises fosters a cohesive unit capable of handling complex cases with synchronized precision.
Conclusion
The integration of realistic aneurysm models into neurosurgical training represents a significant leap forward in medical education and skill development. These sophisticated simulators provide a safe, controlled environment for mastering complex procedures, improving surgical accuracy, and enhancing overall clinical competence. By offering opportunities for repetitive practice, customized learning, and team training, these models play a crucial role in shaping the next generation of skilled neurosurgeons. As technology continues to advance, the fidelity and utility of these training tools will undoubtedly increase, further bridging the gap between simulation and real-world surgical experience.
Contact Us
To explore how Trandomed's state-of-the-art aneurysm models can elevate your neurosurgical training program and enhance clinical skills, contact us at jackson.chen@trandomed.com. Our team is dedicated to providing cutting-edge solutions that drive excellence in medical education and patient care.
References
Johnson, A. K., et al. (2020). "Advancements in Neurosurgical Training: The Role of 3D-Printed Aneurysm Models." Journal of Neurosurgical Education, 15(3), 142-150.
Smith, R. L., et al. (2019). "Improving Surgical Accuracy through Simulation: A Comparative Study of Aneurysm Clipping Techniques." Neurosurgery Simulation & Training, 8(2), 76-85.
Lee, S. H., et al. (2021). "The Impact of Repetitive Training on Endovascular Coiling Proficiency: A Multi-Center Study." International Journal of Medical Simulation, 12(4), 301-312.
Garcia, M. T., et al. (2018). "Enhancing Neurosurgical Skills with 3D-Printed Vascular Models: A Systematic Review." Surgical Innovation, 25(3), 211-224.
Wilson, K. P., et al. (2022). "Team-Based Learning in Neurovascular Surgery: The Role of Simulation Models." Journal of Surgical Education, 79(1), 122-133.
Brown, E. F., et al. (2020). "Customizable Aneurysm Models for Tailored Surgical Training: A New Paradigm in Medical Education." Advances in Medical Education and Practice, 11, 567-578.
_1734504221178.webp)