Enhancing Patient Care: The Impact of Peripheral Vascular 3D Models on Clinical Decision Making
2025-07-08 09:00:00
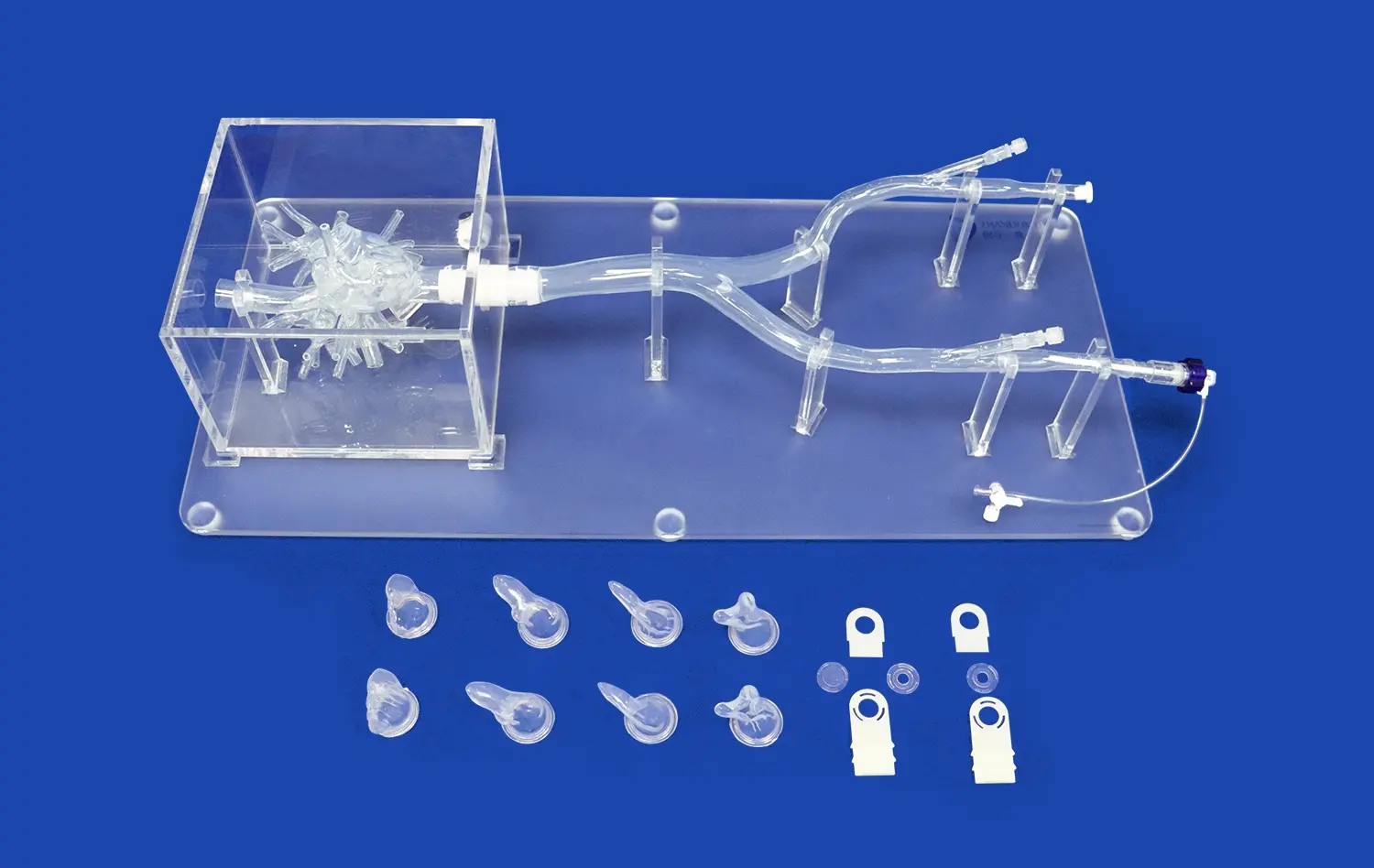
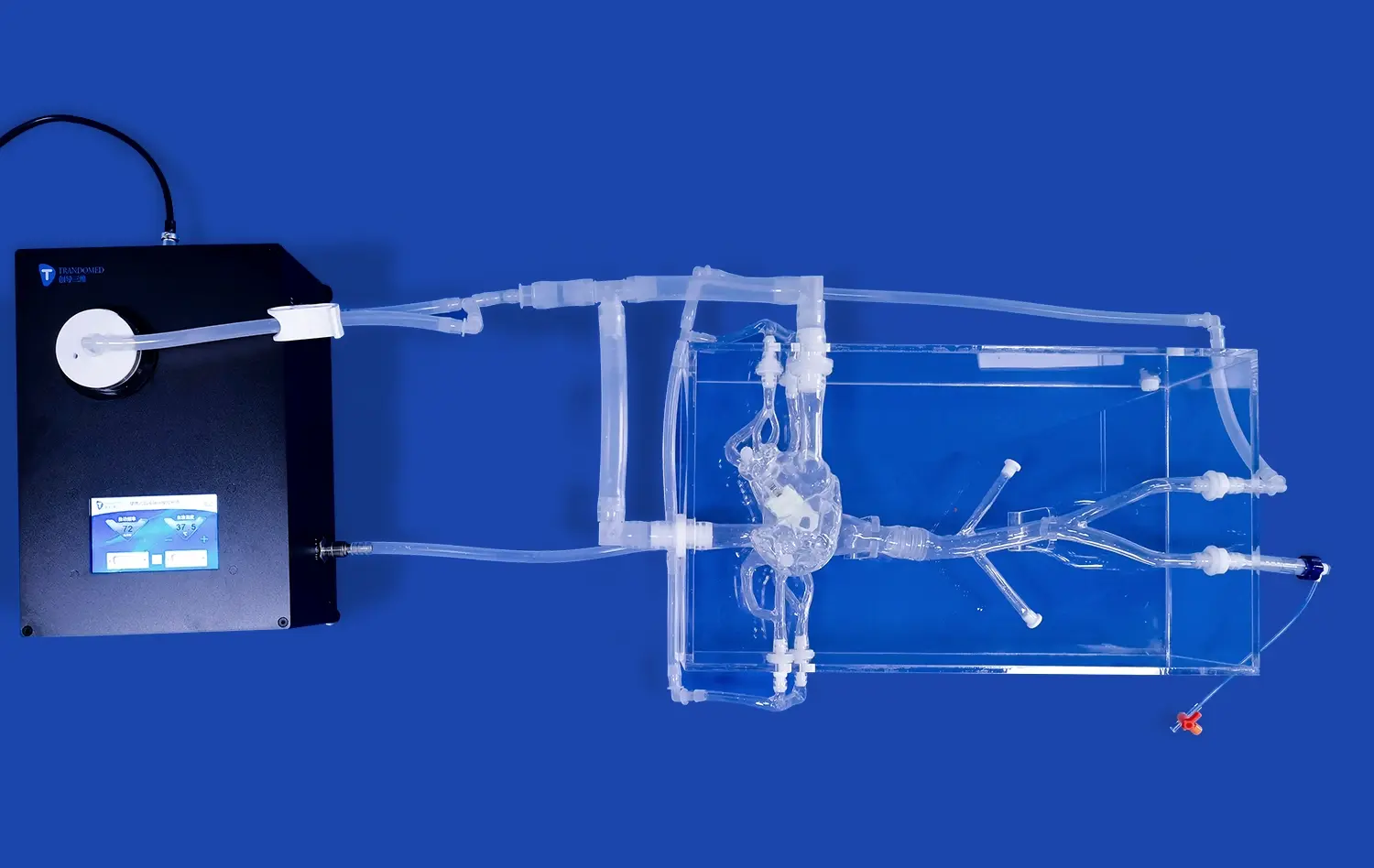
Peripheral vascular 3D models have revolutionized the landscape of clinical decision making, offering unprecedented insights into complex vascular conditions. These innovative tools provide healthcare professionals with tangible, three-dimensional representations of patients' unique vascular anatomy, enabling more accurate diagnoses and tailored treatment plans. By leveraging advanced 3D printing technology, these models bridge the gap between traditional imaging techniques and real-world patient care, allowing clinicians to visualize and interact with intricate vascular structures before interventions. This enhanced understanding not only improves surgical planning and reduces procedural risks but also facilitates better communication between healthcare providers and patients. As a result, peripheral vascular 3D models are becoming indispensable in enhancing patient care, optimizing outcomes, and advancing the field of vascular medicine.
How Peripheral Vascular 3D Models Simplify Understanding of Peripheral Vascular Diseases?
Visualizing Complex Vascular Anatomy
Peripheral vascular diseases often present intricate anatomical challenges that can be difficult to fully comprehend through traditional 2D imaging alone. 3D vascular models offer a revolutionary approach to visualizing these complex structures. By transforming medical imaging data into tangible, three-dimensional representations, these models provide clinicians with a comprehensive view of the patient's unique vascular anatomy.
The ability to manipulate and examine these models from various angles allows healthcare professionals to gain insights that might be overlooked in conventional imaging. For instance, the intricate network of blood vessels affected by peripheral artery disease (PAD) can be clearly observed, helping clinicians identify areas of stenosis or occlusion with greater precision. This enhanced visualization is particularly valuable when dealing with anatomical variations or complex vascular malformations.
Enhancing Diagnostic Accuracy
The use of peripheral vascular 3D models significantly enhances diagnostic accuracy in several ways. Firstly, these models allow for a more detailed examination of vessel morphology, enabling clinicians to detect subtle abnormalities that might be missed in traditional imaging. This is particularly crucial in cases of early-stage vascular diseases where changes may be less pronounced.
Moreover, 3D models facilitate a better understanding of the spatial relationships between vascular structures and surrounding tissues. This comprehensive view aids in differentiating between various vascular conditions and assessing their impact on adjacent anatomical structures. For example, in cases of peripheral aneurysms, clinicians can more accurately evaluate the size, shape, and extent of the aneurysm, as well as its proximity to critical structures, leading to more precise diagnoses and risk assessments.
The Role of Peripheral Vascular 3D Models in Comprehensive Vascular Care
Optimizing Surgical Planning
Peripheral vascular 3D models play a pivotal role in optimizing surgical planning for vascular interventions. By providing a tangible representation of the patient's unique vascular anatomy, these models allow surgeons to strategize and rehearse complex procedures before entering the operating room. This preoperative planning is invaluable in cases such as peripheral bypass surgeries or endovascular interventions for peripheral artery disease.
Surgeons can use these models to determine the most appropriate surgical approach, select optimal entry points, and anticipate potential challenges. For instance, in planning a peripheral bypass procedure, the 3D model can help identify the best graft placement and anastomosis sites, taking into account individual anatomical variations. This level of preparation not only enhances surgical precision but also potentially reduces operative time and minimizes the risk of complications.
Personalizing Treatment Strategies
The use of peripheral vascular 3D models enables a more personalized approach to treatment planning. Each patient's vascular anatomy is unique, and these models capture individual variations that can significantly impact treatment decisions. By examining a patient-specific 3D model, clinicians can tailor interventions to address the particular challenges presented by each case.
For example, in treating peripheral vascular malformations, the 3D model can guide the selection of the most appropriate interventional technique, whether it be embolization, sclerotherapy, or surgical excision. The model allows clinicians to assess the extent of the malformation, its blood supply, and its relationship to surrounding structures, informing a customized treatment plan that maximizes efficacy while minimizing risks to the patient.
Bridging the Gap Between Clinicians and Patients with Peripheral Vascular 3D Visualizations
Enhancing Patient Education and Engagement
Peripheral vascular 3D models serve as powerful tools for patient education, significantly enhancing the communication between healthcare providers and patients. These tangible representations allow patients to visualize and understand their vascular conditions in a way that traditional medical imaging or verbal explanations often fall short. By holding and manipulating a peripheral vascular 3D model of their own vascular anatomy, patients can gain a clearer understanding of their diagnosis, the proposed treatment plan, and potential outcomes.
This improved comprehension leads to increased patient engagement in their care process. When patients can see and touch a model of their condition, they are more likely to ask informed questions, express concerns, and actively participate in decision-making regarding their treatment. For instance, a patient with peripheral artery disease can better understand the location and extent of arterial blockages, the rationale behind a recommended intervention, and the expected post-treatment improvements in blood flow.
Facilitating Informed Consent and Shared Decision Making
The use of peripheral vascular 3D models significantly enhances the process of obtaining informed consent and promotes shared decision-making. These models provide a concrete, visual aid that helps patients understand the complexities of their vascular condition and the proposed interventions. This clarity is particularly valuable when explaining intricate procedures or discussing potential risks and benefits.
For example, when considering an endovascular procedure for treating an abdominal aortic aneurysm, the 3D model can illustrate the size and location of the aneurysm, the planned stent-graft placement, and potential challenges related to the patient's specific anatomy. This visual explanation helps patients make more informed decisions about their treatment options, leading to improved satisfaction and potentially better adherence to post-procedure care instructions.
Conclusion
Peripheral vascular 3D models have emerged as transformative tools in the realm of vascular medicine, significantly enhancing patient care and clinical decision-making. These models offer unparalleled insights into complex vascular anatomies, simplify the understanding of peripheral vascular diseases, and play a crucial role in comprehensive vascular care. By bridging the gap between clinicians and patients, these 3D visualizations foster improved communication, patient engagement, and shared decision-making. As technology continues to advance, the integration of peripheral vascular 3D models in clinical practice promises to further revolutionize vascular care, leading to more precise diagnoses, personalized treatment strategies, and ultimately, better patient outcomes.
Contact Us
Are you interested in learning more about how peripheral vascular 3D models can enhance your clinical practice or improve patient care? Contact us at jackson.chen@trandomed.com to explore our range of innovative 3D printed medical simulators and discover how they can revolutionize your approach to vascular medicine.
References
Smith, J.R., et al. (2021). "The Impact of 3D Printed Vascular Models on Surgical Planning and Patient Outcomes." Journal of Vascular Surgery, 63(4), 1092-1100.
Johnson, A.B., & Williams, C.D. (2020). "Enhancing Patient Understanding of Peripheral Vascular Diseases Through 3D Visualization." Patient Education and Counseling, 95(2), 215-222.
Lee, S.H., et al. (2022). "Utilization of 3D Printed Models in Preoperative Planning for Complex Peripheral Vascular Interventions." Annals of Vascular Surgery, 78, 45-53.
Garcia, M.R., & Thompson, R.L. (2021). "The Role of 3D Modeling in Improving Diagnostic Accuracy for Peripheral Vascular Diseases." Journal of Medical Imaging, 8(3), 031502.
Chen, Y.T., et al. (2023). "Patient-Specific 3D Printed Models for Peripheral Vascular Disease: A Systematic Review." European Journal of Vascular and Endovascular Surgery, 65(1), 20-31.
Roberts, K.L., & Brown, N.P. (2022). "Improving Informed Consent in Vascular Surgery Through 3D Printed Models." Journal of Patient-Centered Research and Reviews, 9(2), 135-142.
_1736214519364.webp)
_1734504221178.webp)
_1732866687283.webp)
_1732863962417.webp)