Why Is Bifurcation Lesion Training Critical for Interventional Cardiologists?
Complexity of Bifurcation Lesions
Coronary bifurcation lesions are inherently challenging due to their intricate anatomical structure and the critical risk of obstructing blood flow to side branches originating from the junction where a main vessel divides. This specific location creates natural turbulence and flow recirculation zones, promoting significant plaque buildup. The complex geometry, involving angulation and carina position, makes these lesions exceptionally susceptible to complications like restenosis (re-narrowing) and stent thrombosis (clot formation) following intervention. Consequently, standard percutaneous coronary intervention (PCI) approaches are often insufficient, demanding specialized techniques and strategies tailored to safely address both the main vessel and the side branch simultaneously to ensure optimal outcomes.
High-Stakes Decision Making
Performing PCI on bifurcation lesions requires interventional cardiologists to make crucial, real-time decisions that profoundly influence success. Key choices include determining the necessity of side branch treatment, selecting the most appropriate stenting technique (e.g., provisional, culotte, T-stenting), and meticulously planning stent positioning and expansion to avoid compromising either branch. Each decision carries significant weight, directly impacting immediate procedural results such as avoiding branch occlusion, and long-term patient prognosis, including risks of myocardial infarction or repeat revascularization. Training on neuro vascular simulators provides a vital, risk-free environment for practitioners to repeatedly practice these complex decisions and refine essential technical skills before performing high-pressure live procedures on patients.
Evolving Techniques and Technologies
The management of coronary bifurcation lesions is a rapidly advancing field, characterized by continuous innovation in dedicated bifurcation stent designs, specialized guidewires, imaging modalities like intravascular ultrasound (IVUS), and refined procedural algorithms. Keeping pace with these frequent advancements is essential for optimal patient care but requires substantial commitment to ongoing education and practical experience. Simulation platforms serve as a highly valuable, flexible, and cost-effective solution. They enable interventional cardiologists to safely gain familiarity and proficiency with novel devices, practice emerging techniques, and understand complex treatment protocols without exposing actual patients to the inherent risks of the learning curve associated with adopting new technologies.
Side Branch Access and Stent Optimization Techniques
Mastering Wire Manipulation
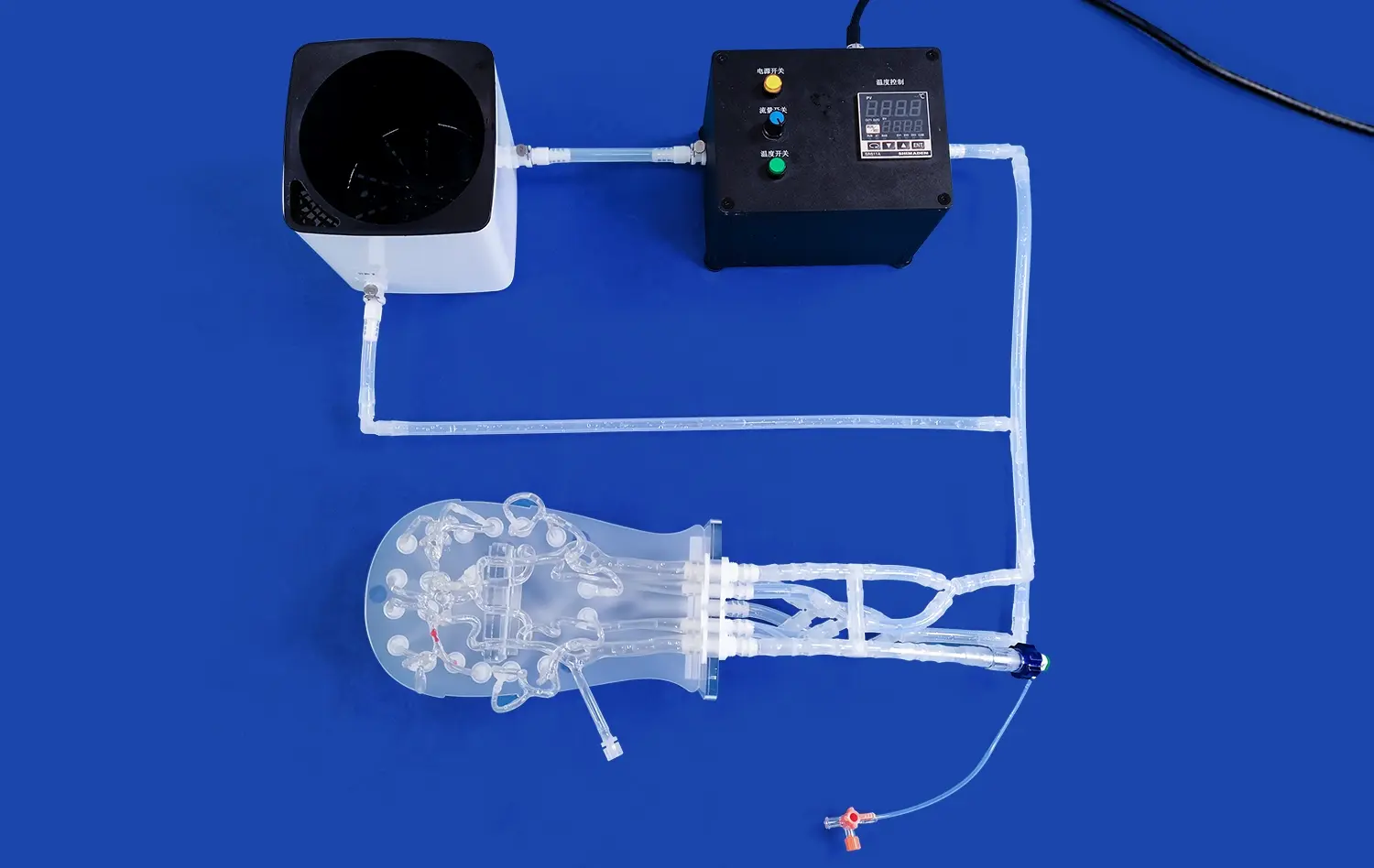
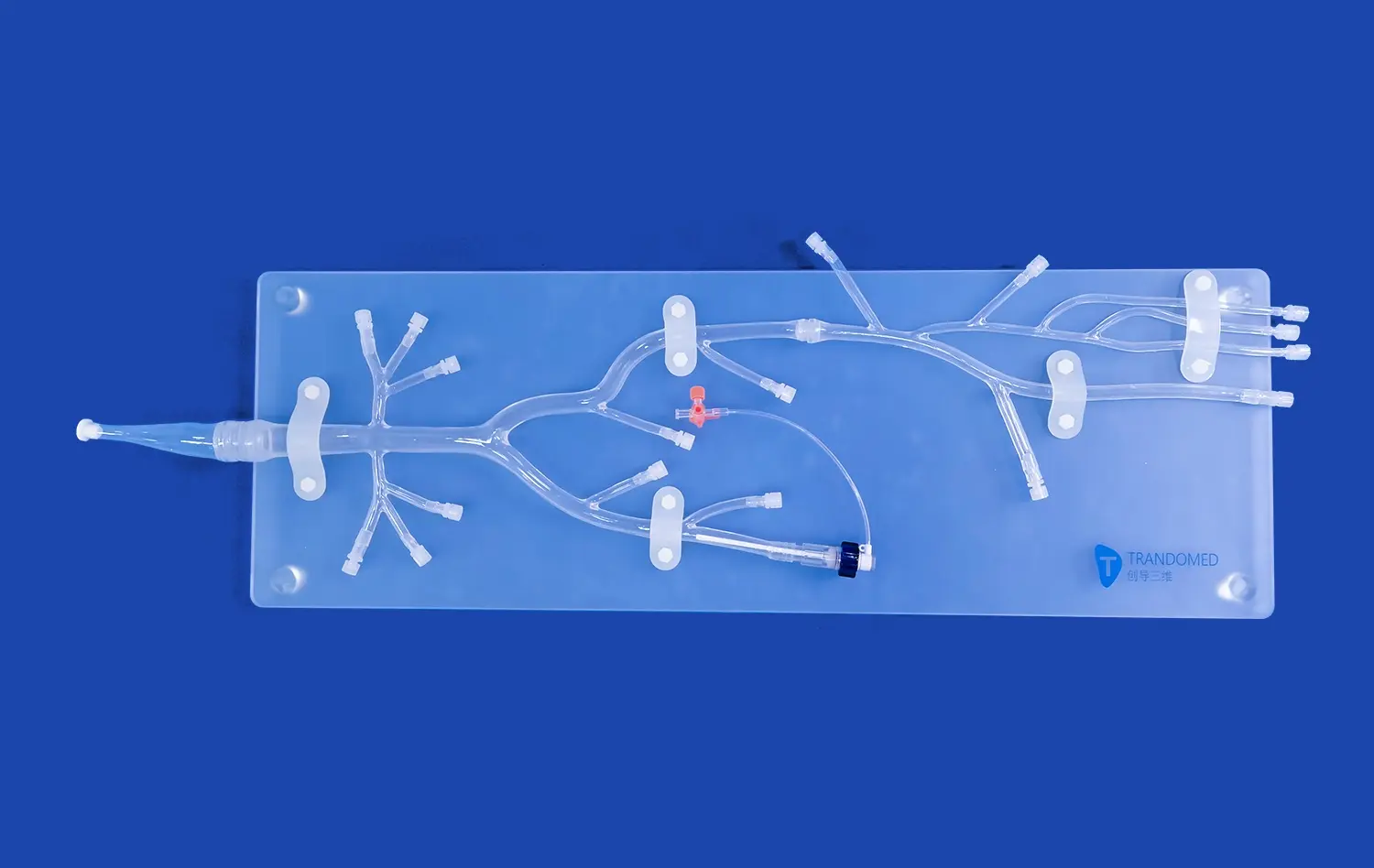
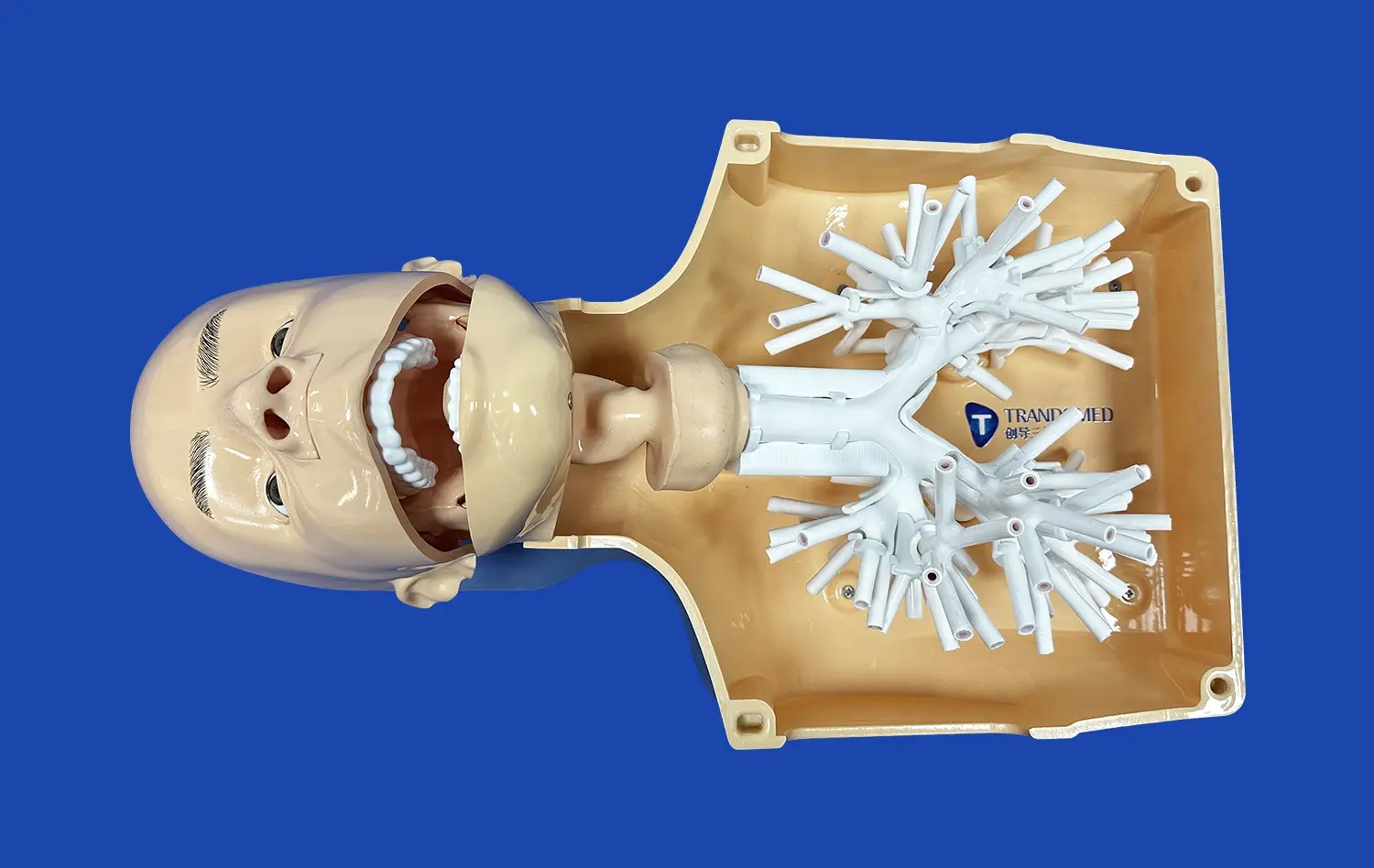
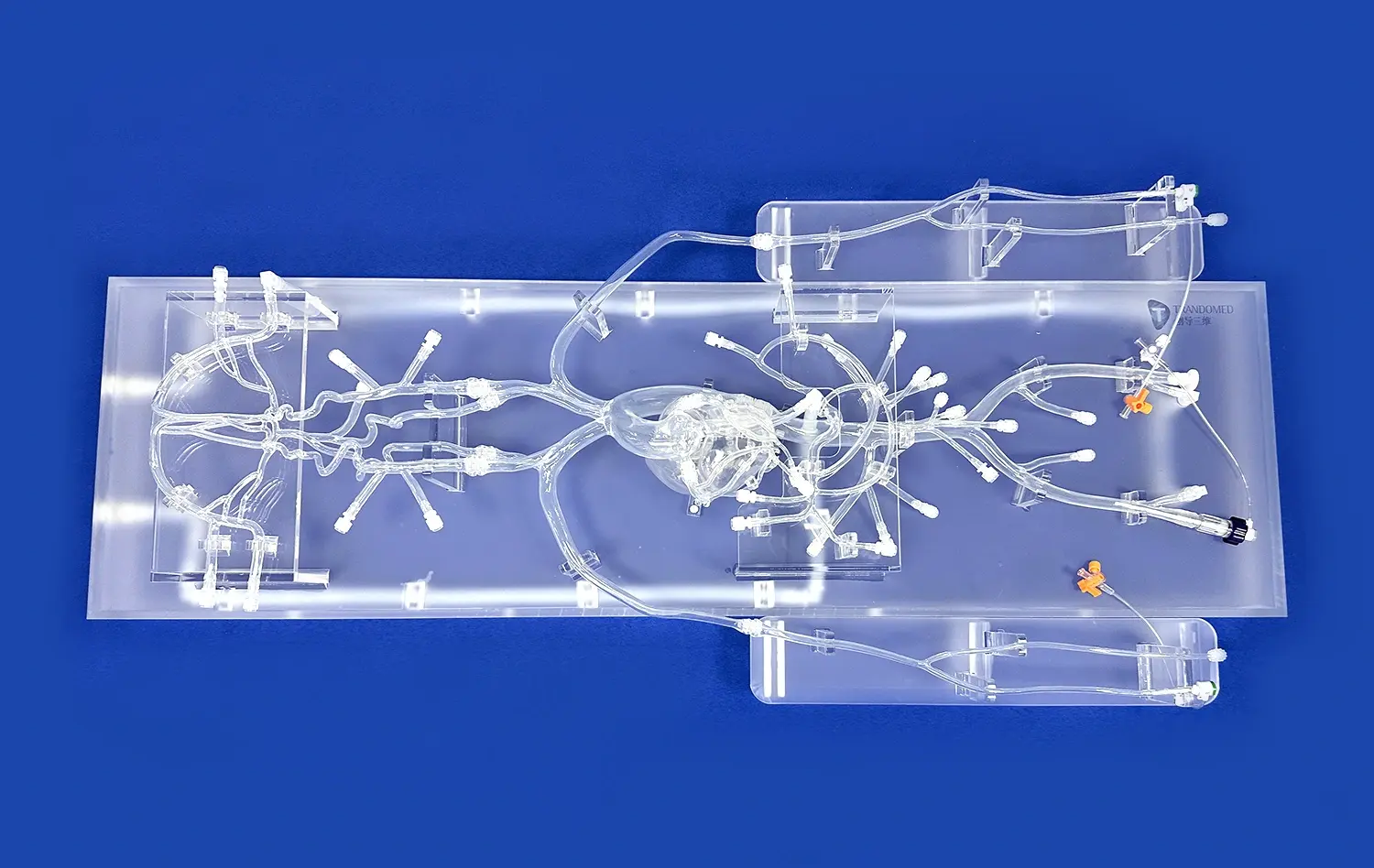
Accessing and protecting side branches during bifurcation PCI procedures demands exceptional wire manipulation skills. Advanced simulators, such as those incorporating neuro vascular simulator technology, provide a realistic environment for practitioners to perfect their wire navigation techniques. These platforms can replicate various bifurcation angles and vessel tortuosity, allowing cardiologists to practice negotiating challenging anatomies repeatedly.
Stent Positioning Strategies
Optimal stent positioning is crucial for successful bifurcation treatment. Simulation training with neuro vascular simulator enables interventional cardiologists to experiment with different stenting techniques, such as provisional stenting, T-stenting, crush techniques, and the more complex double kissing crush method. By practicing these approaches on anatomically accurate models, practitioners can develop a nuanced understanding of how stent placement affects both the main vessel and side branch patency.
Balloon Dilatation and Kissing Balloon Techniques
Proper balloon dilatation is essential for ensuring adequate stent expansion and apposition in bifurcation lesions. Advanced coronary simulators allow cardiologists to practice various balloon inflation strategies, including sequential and simultaneous kissing balloon techniques. These exercises help refine the timing and pressure application skills necessary for optimal stent deployment and side branch preservation.
Improving Procedural Outcomes Through Repeated Simulation Practice
Building Muscle Memory
Repeated practice on high-fidelity simulators helps interventional cardiologists develop the muscle memory and hand-eye coordination essential for smooth and efficient procedures. The tactile feedback provided by advanced simulation platforms, including those utilizing neuro vascular simulator technology, closely mimics the sensations experienced during actual interventions. This realism allows practitioners to internalize the subtle nuances of catheter and wire manipulation, translating to improved performance in the cardiac catheterization laboratory.
Scenario-Based Learning
Modern coronary bifurcation and neuro vascular simulators offer a wide range of scenario-based training modules. These scenarios can replicate various clinical situations, from straightforward cases to complex, high-risk interventions. By working through diverse case studies, interventional cardiologists can expand their problem-solving skills and learn to adapt their techniques to different anatomical and pathological presentations. This comprehensive approach to training prepares practitioners for the unpredictable nature of real-world procedures.
Performance Analysis and Feedback
Advanced simulation platforms often incorporate sophisticated analytics and performance tracking features. These tools provide objective measurements of procedural efficiency, accuracy, and outcomes. Interventional cardiologists can review their performance metrics, identify areas for improvement, and track their progress over time. This data-driven approach to skill development accelerates learning and helps practitioners refine their techniques with precision.
Conclusion
Realistic coronary bifurcation simulation represents a paradigm shift in interventional cardiology training. By providing a safe, repeatable, and highly realistic environment for skill development, these advanced platforms are elevating the standard of care in PCI procedures. As simulation technology continues to evolve, incorporating innovations like the neuro vascular simulator, the potential for enhancing interventional skills and improving patient outcomes grows exponentially. Embracing these cutting-edge training tools is essential for interventional cardiologists committed to excellence in treating complex coronary lesions.
Contact Us
To explore how Trandomed's state-of-the-art 3D printed medical simulators can revolutionize your interventional cardiology training program, contact us at jackson.chen@trandomed.com. Our customizable solutions offer unparalleled realism and versatility, helping you stay at the forefront of medical education and patient care.

_1732863713705.webp)