How Do Models Improve Catheter Navigation and Clot Removal Skills?
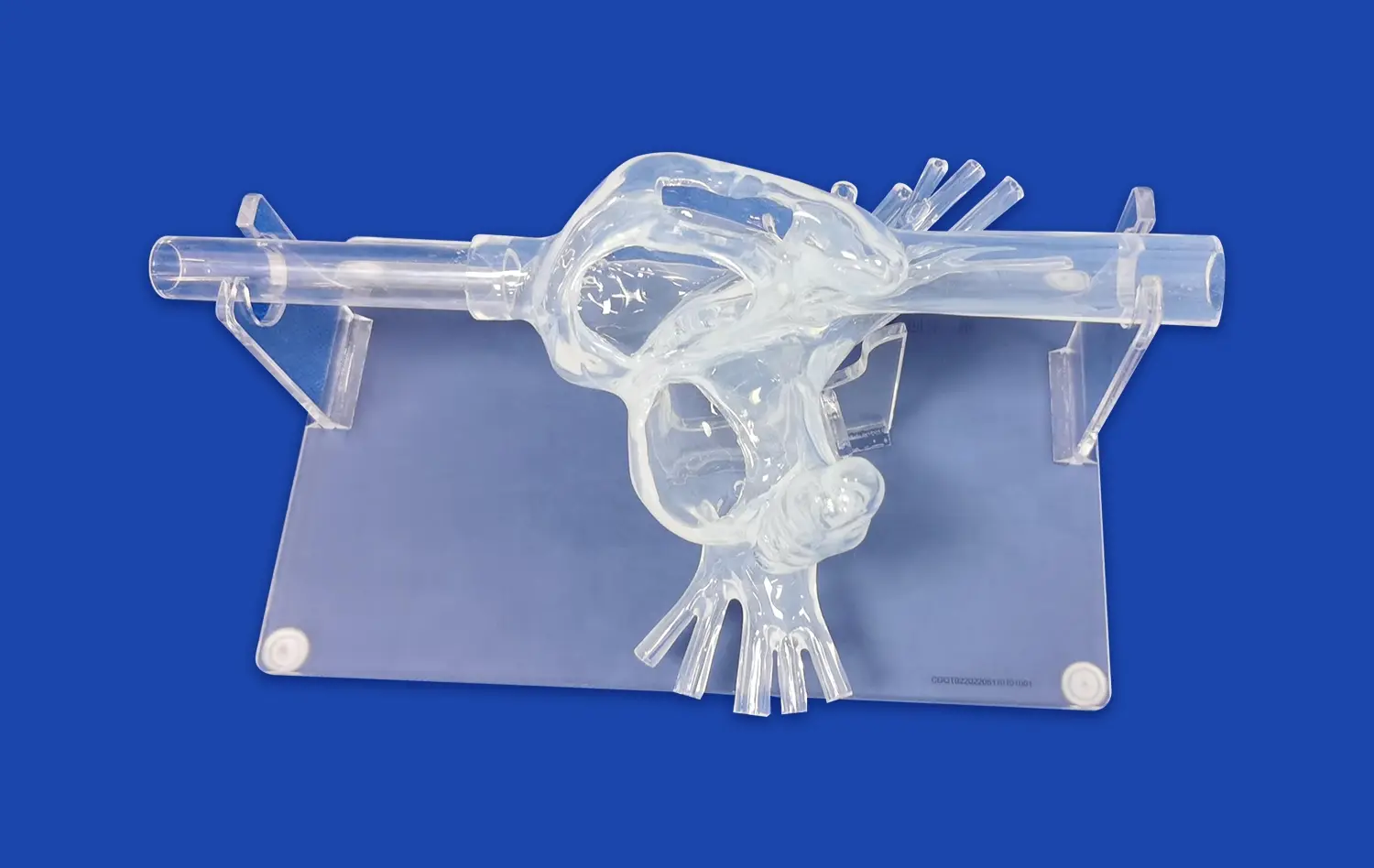
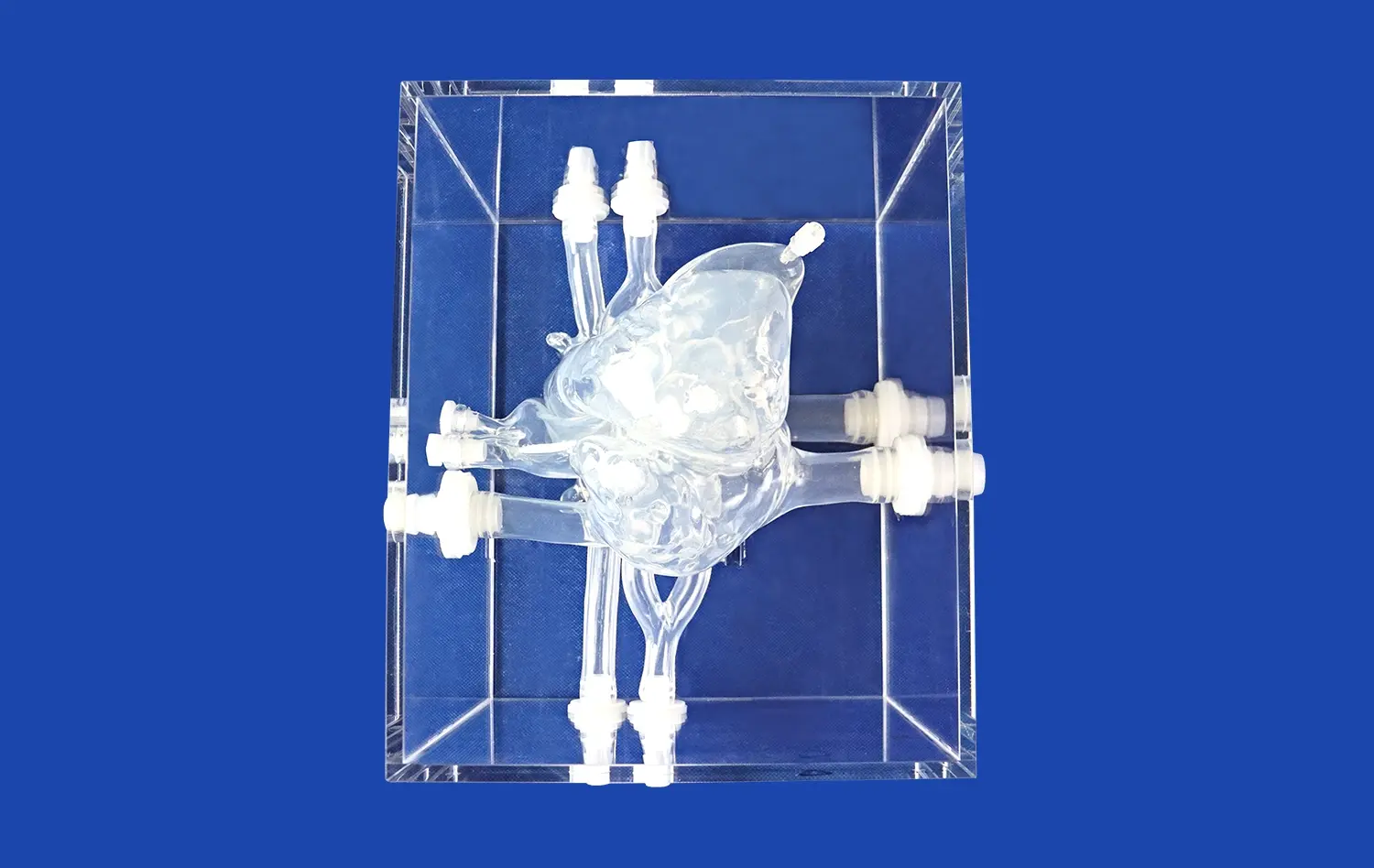
Anatomical Accuracy for Realistic Training
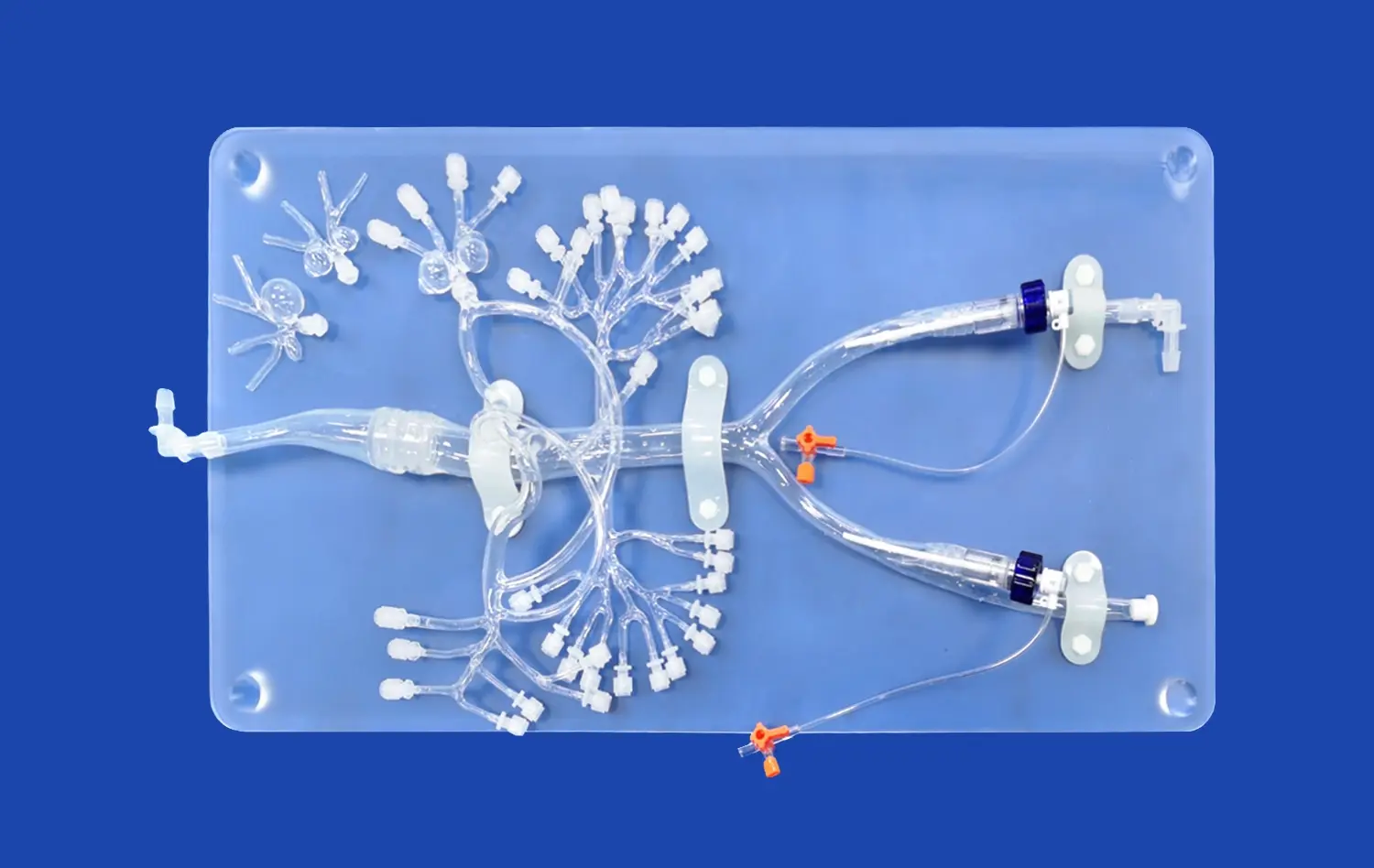
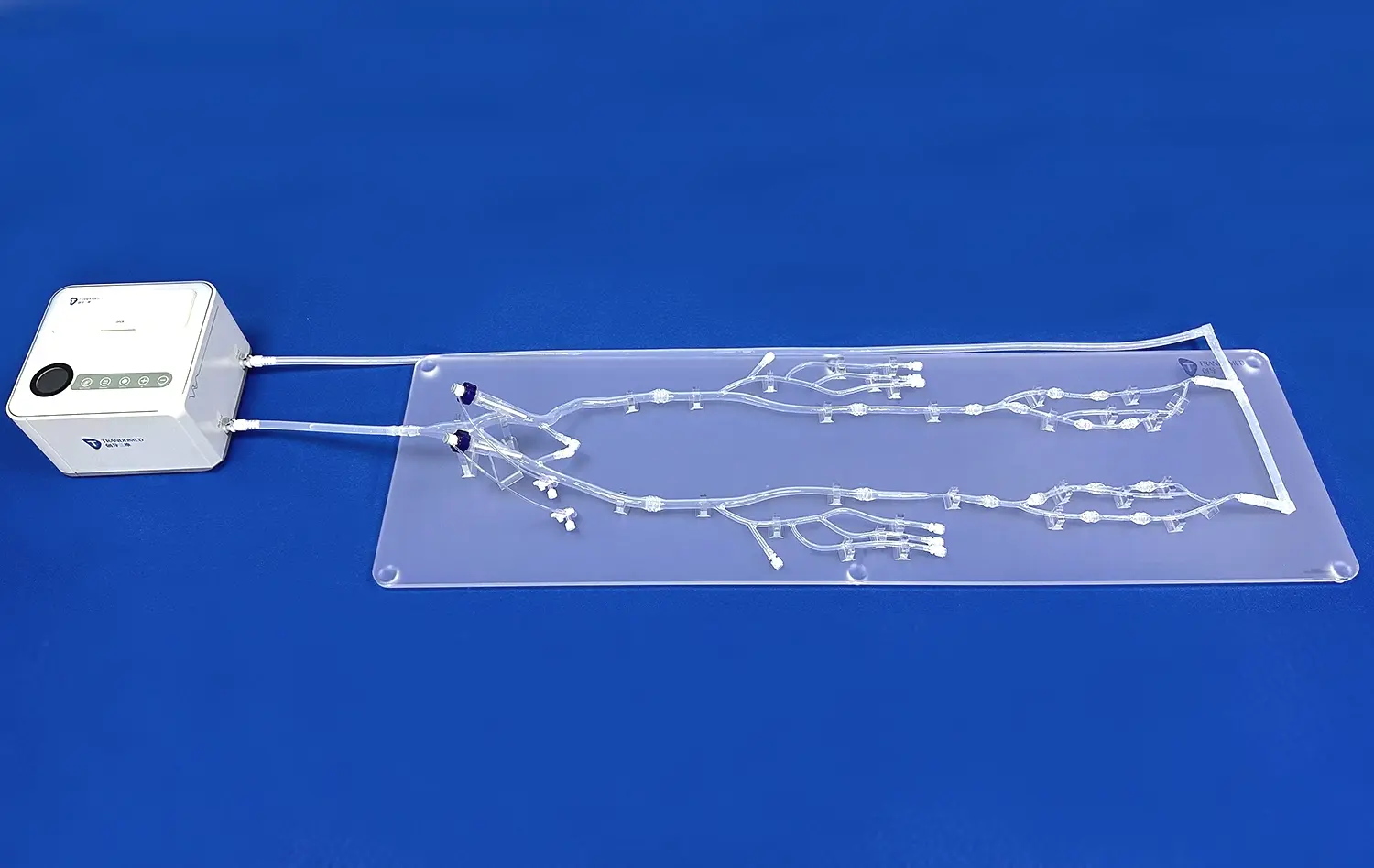
Pulmonary artery models provide an unparalleled level of anatomical accuracy, replicating the intricate network of blood vessels from the femoral vein to the pulmonary arteries. These models include detailed representations of the iliac vein, inferior vena cava, right atrium, right ventricle, and pulmonary artery branches. The inclusion of up to ten levels of bifurcation on both the left and right sides allows trainees to navigate the complex pulmonary vascular system with precision. This level of detail is crucial for developing the spatial awareness and dexterity required for successful catheter navigation during PE procedures.
Simulating Pathological Conditions
Advanced pulmonary artery models offer the ability to customize pathological conditions, such as embolisms, malformations, and tortuosity at the distal ends of the pulmonary arteries. This feature enables medical professionals to practice identifying and treating various PE scenarios. By encountering these simulated pathologies, practitioners can refine their diagnostic skills and develop effective strategies for clot removal in different anatomical contexts. The ability to repeatedly practice on models with varying degrees of complexity helps build confidence and competence in handling challenging cases.
Enhancing Procedural Techniques
Through repeated practice on pulmonary artery models, healthcare providers can perfect their catheter manipulation techniques and clot removal procedures. The models allow for the simulation of various interventional techniques, including catheter-directed thrombolysis and mechanical thrombectomy. By practicing these procedures in a controlled environment, medical professionals can optimize their hand-eye coordination, improve their ability to navigate tortuous vessels, and develop muscle memory for precise catheter control. This hands-on experience translates directly to improved performance in clinical settings, potentially leading to better patient outcomes.
Real-Time Feedback for Procedural Optimization
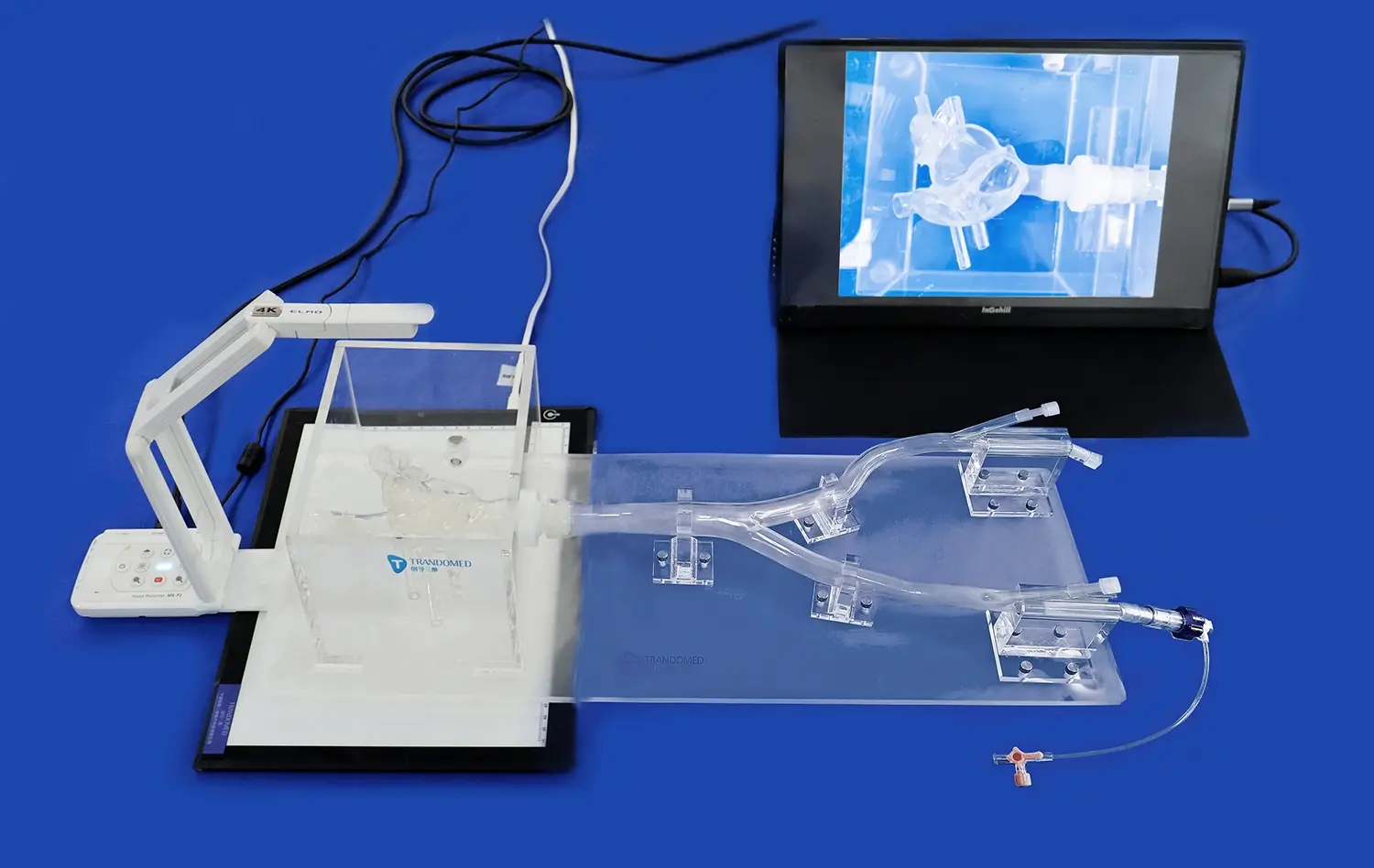
Visual Cues for Performance Assessment
Pulmonary artery models often incorporate transparent materials or imaging capabilities that provide immediate visual feedback during simulated procedures. This real-time visualization allows practitioners to observe the movement and positioning of catheters and devices within the vascular system. By seeing the direct results of their actions, healthcare providers can quickly identify areas for improvement and make necessary adjustments to their technique. This immediate feedback loop accelerates the learning process and helps develop a more intuitive understanding of catheter behavior within complex anatomical structures.
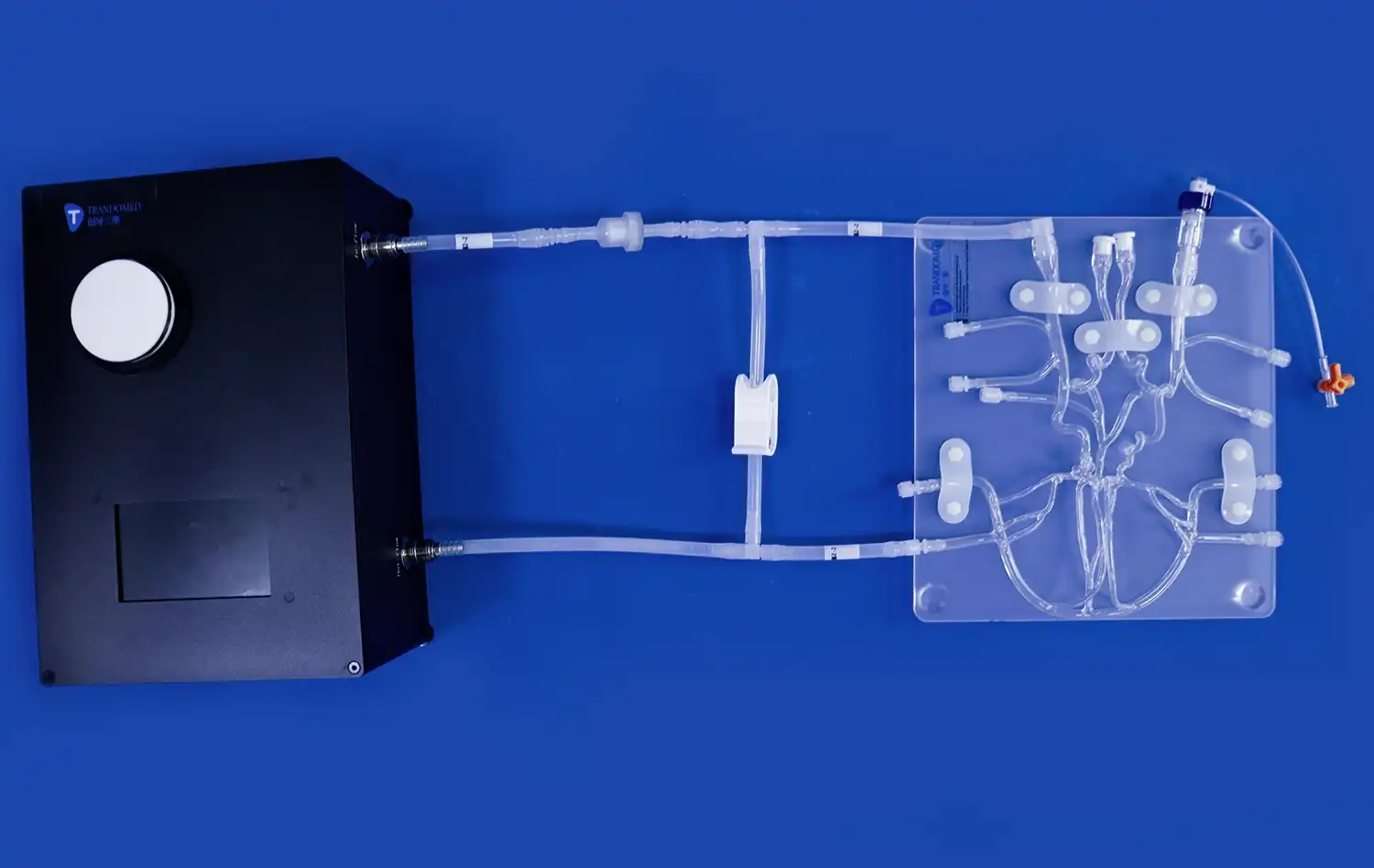
Quantitative Performance Metrics
Advanced pulmonary artery simulators incorporating detailed pulmonary artery models can be equipped with sensors and tracking systems that provide quantitative data on procedural performance. These metrics may include catheter insertion time, navigation accuracy, and success rates in reaching target locations within the pulmonary vasculature. By analyzing this data, medical professionals can objectively assess their progress and identify specific areas that require further refinement. This data-driven approach to skill development allows for targeted improvement strategies and helps track long-term progress in procedural proficiency.
Collaborative Learning and Peer Review
Pulmonary artery models facilitate collaborative learning environments where multiple practitioners can observe and critique each other's techniques. This peer review process, combined with expert guidance, provides valuable insights and alternative approaches to challenging scenarios. By sharing experiences and discussing strategies, healthcare providers can collectively optimize their procedures and develop best practices for PE interventions. This collaborative approach fosters a culture of continuous improvement and knowledge sharing within the medical community.
Increasing Operator Proficiency Before Clinical Procedures
Graduated Difficulty Levels
Pulmonary artery models can be designed with varying levels of complexity, allowing for a graduated approach to skill development. Beginners can start with simpler models that focus on basic catheter navigation and progressively move to more intricate scenarios involving complex pathologies. This step-by-step progression ensures that practitioners build a solid foundation of skills before tackling more challenging cases. By mastering each level of difficulty, healthcare providers can systematically increase their proficiency and confidence in performing PE procedures.
Repetitive Practice Without Patient Risk
One of the primary advantages of using pulmonary artery models is the ability to engage in repetitive practice without exposing patients to any risk. This risk-free environment allows medical professionals to experiment with different techniques, learn from mistakes, and perfect their skills without the pressure of live clinical situations. The opportunity for unlimited practice sessions enables practitioners to achieve a high level of procedural mastery before performing interventions on actual patients. This approach not only enhances operator proficiency but also contributes to improved patient safety and outcomes.
Customized Training Programs
Pulmonary artery models can be integrated into comprehensive training programs tailored to individual learning needs and institutional requirements. These customized programs may include structured curricula, performance benchmarks, and assessment protocols to ensure that practitioners achieve and maintain the necessary skill levels for PE procedures. By incorporating pulmonary artery simulations into formal training programs, healthcare institutions can standardize their approach to skill development and ensure consistent quality in PE interventions across their organization.
Conclusion
The integration of advanced pulmonary artery models into medical training and practice represents a significant leap forward in enhancing pulmonary embolism procedures. These sophisticated simulators provide a realistic and risk-free environment for healthcare providers to refine their catheter navigation and clot removal skills. Through anatomical accuracy, pathology simulation, and real-time feedback mechanisms, pulmonary artery models offer an unparalleled opportunity for skill development and procedural optimization. By increasing operator proficiency before clinical procedures, these models contribute to improved patient outcomes and safety in the challenging field of pulmonary embolism treatment.
Contact Us
To learn more about our cutting-edge pulmonary artery models and how they can elevate your PE procedure training, contact Trandomed today. Our expert team is ready to assist you in selecting the perfect model for your institution's needs. Discover how our advanced medical simulators can transform your training programs and contribute to better patient care. Reach out to us at jackson.chen@trandomed.com for personalized guidance and product information.