Enhancing Pulmonary Vein Ablation Device Testing with the Atrial Septal Puncture Model
2025-09-15 09:00:03
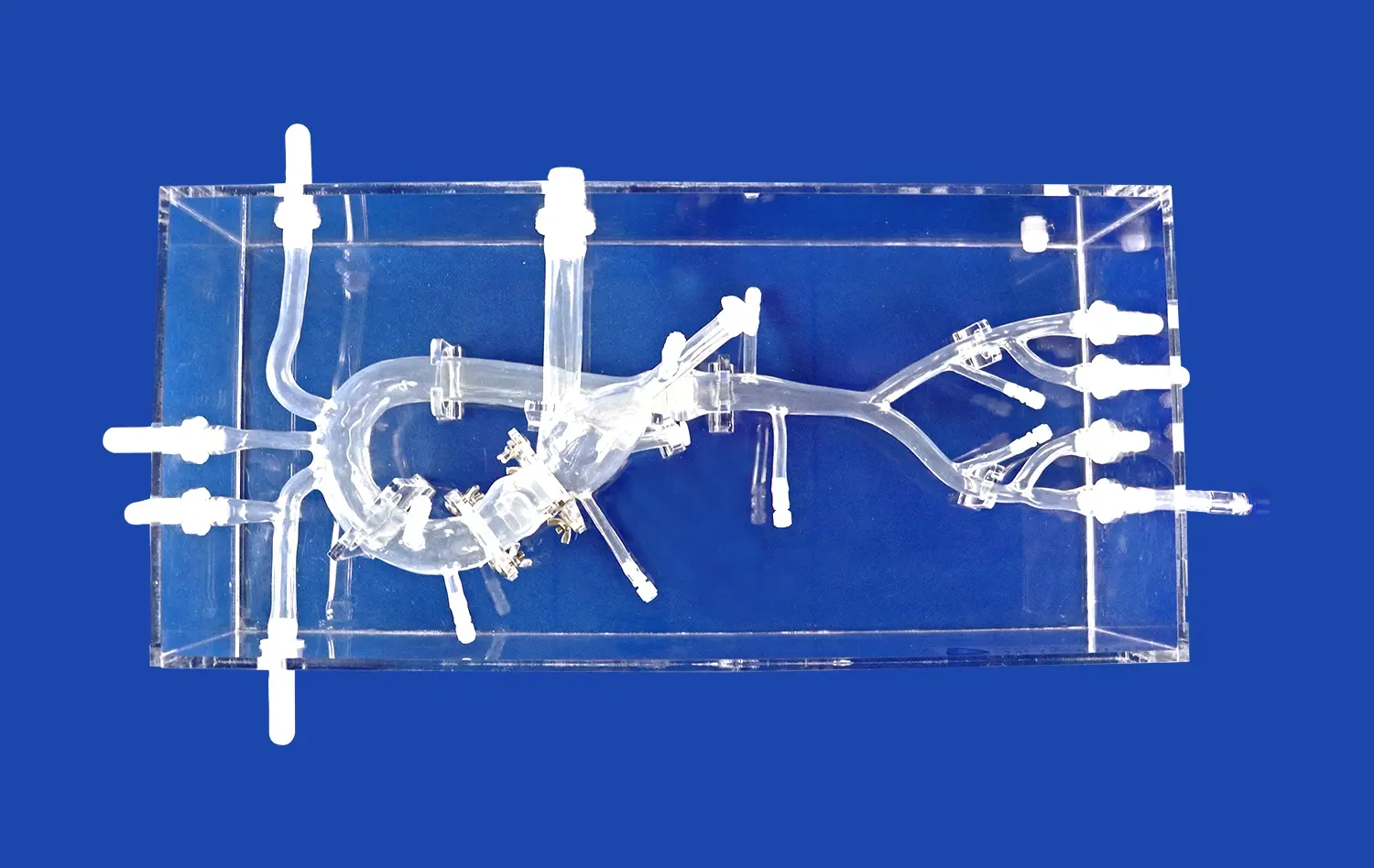
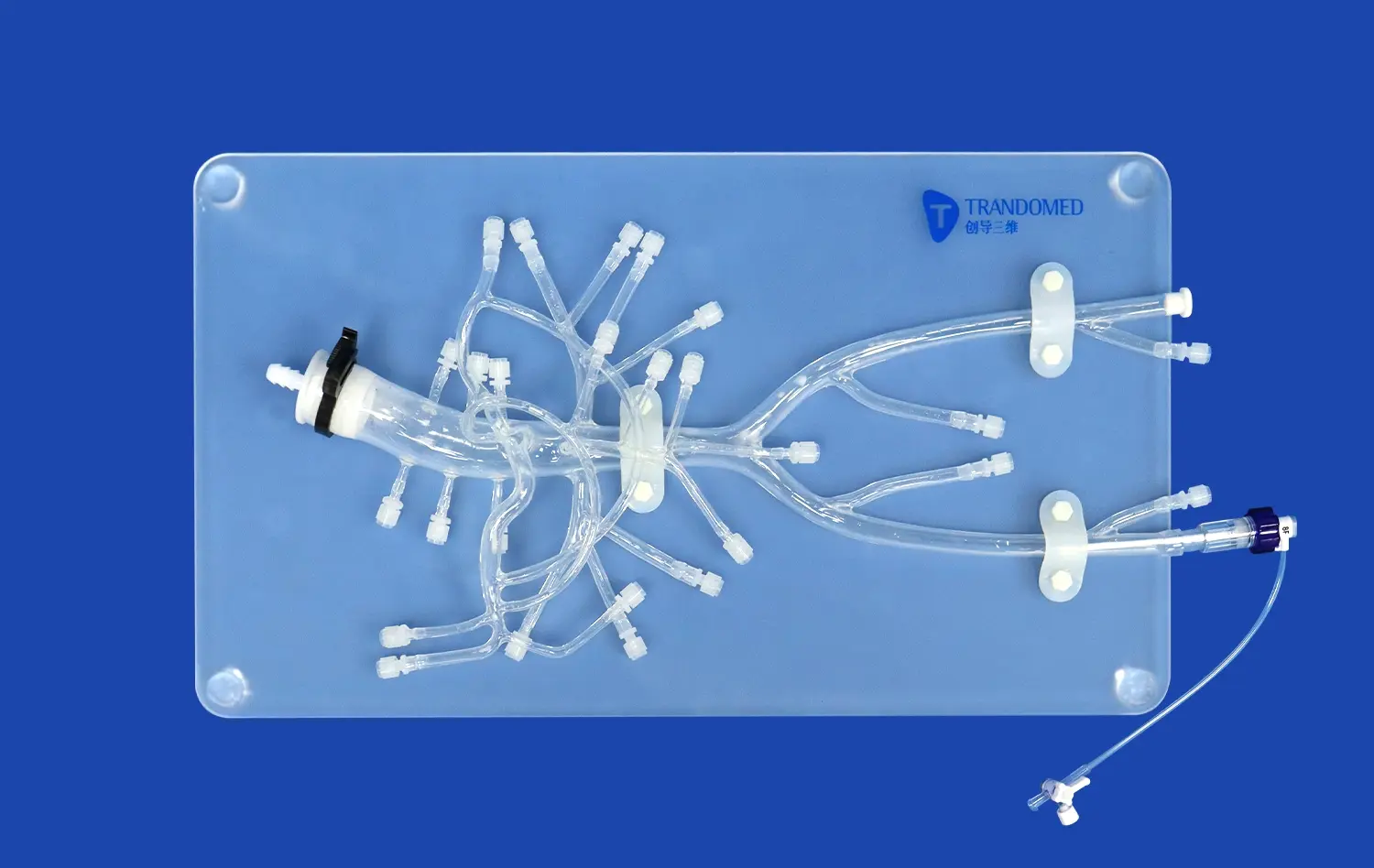
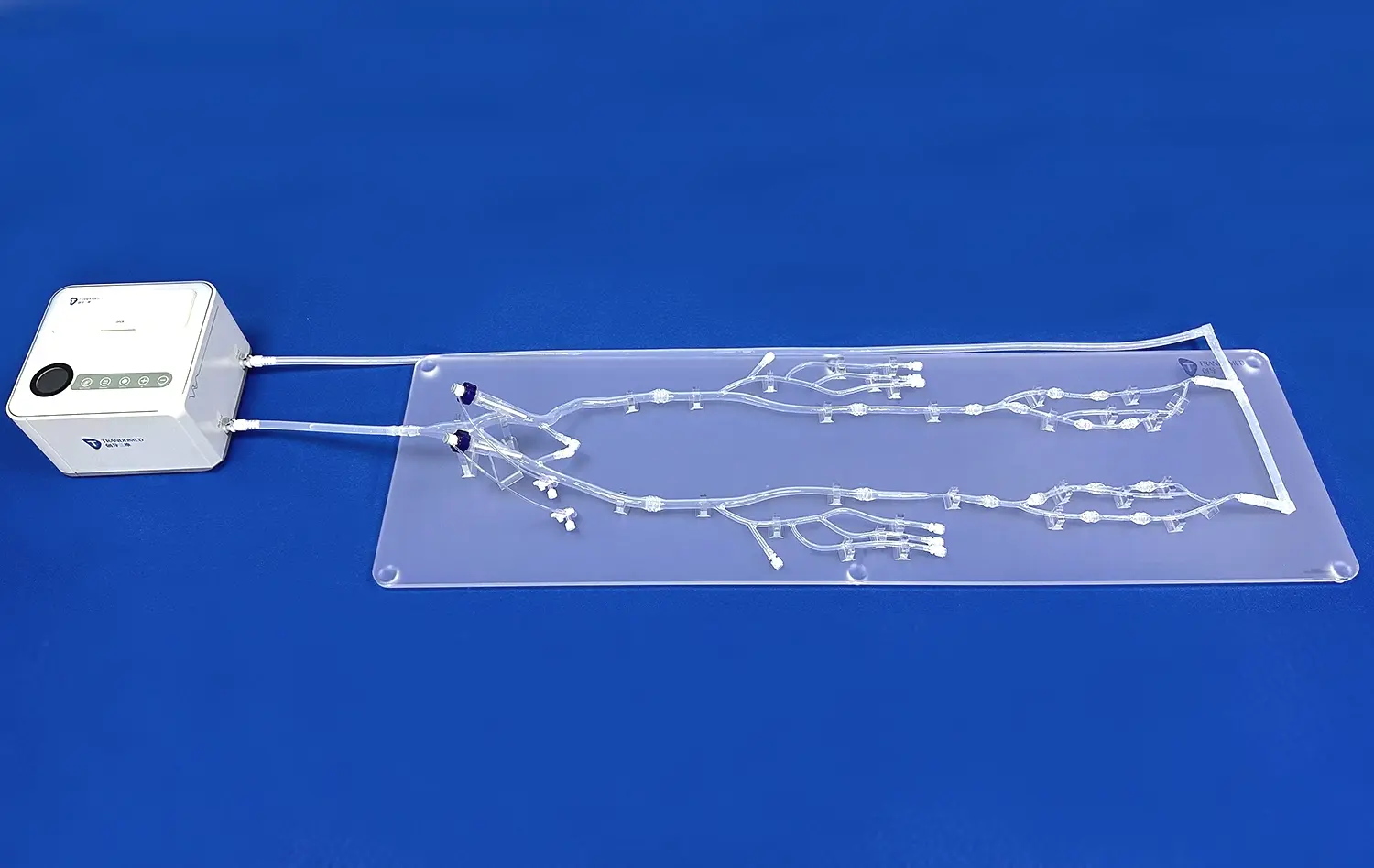
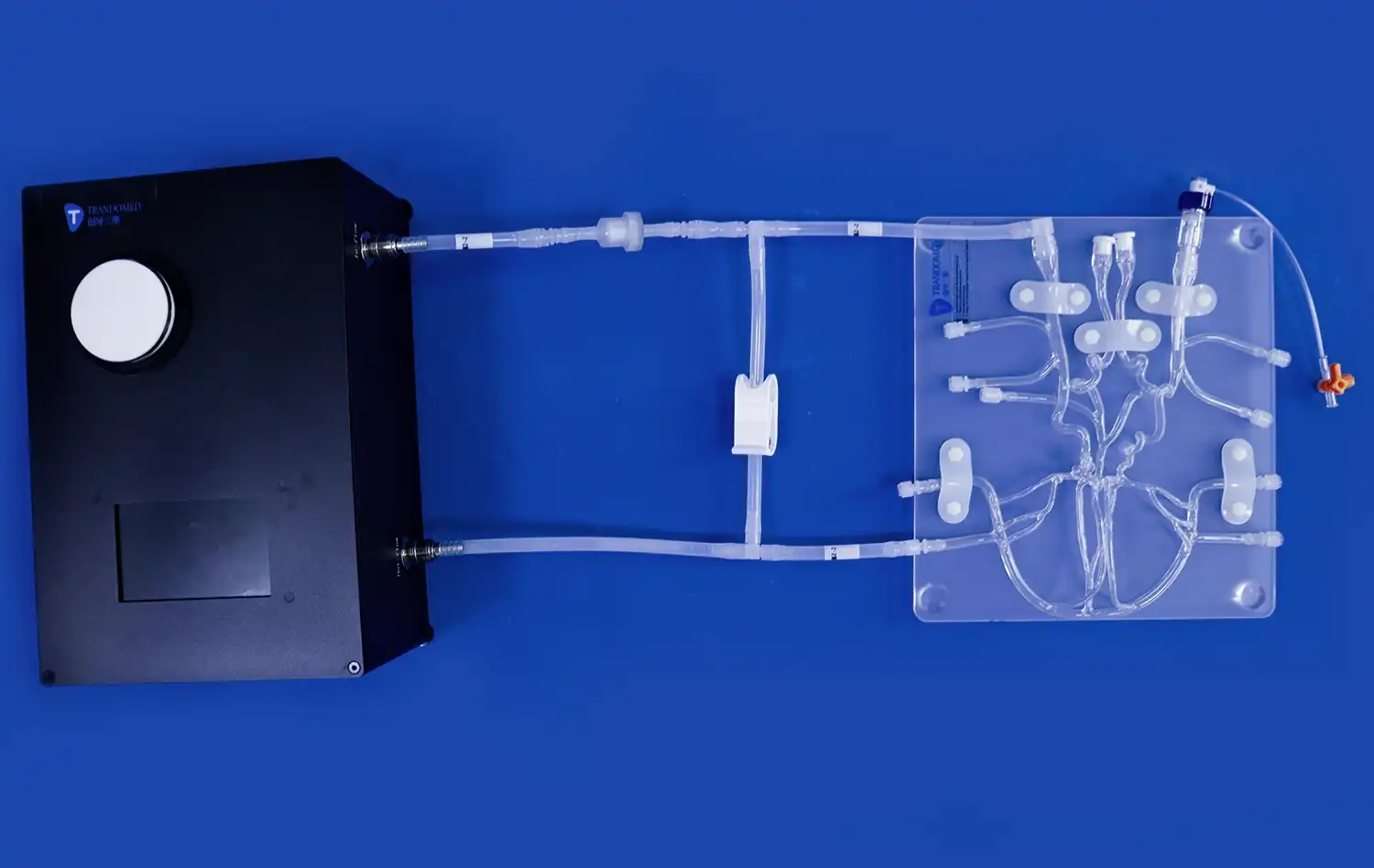
Pulmonary vein ablation is a critical procedure for treating atrial fibrillation, and the development of effective devices for this treatment relies heavily on accurate testing and simulation. The atrial septal puncture model has emerged as an invaluable tool in this field, offering a realistic platform for device testing and validation. By replicating the complex anatomy of the heart, including the atrial septum and pulmonary veins, this model allows researchers and medical device manufacturers to assess the performance, safety, and efficacy of ablation catheters and balloon systems. The model's ability to simulate various anatomical variations and pathological conditions provides a comprehensive testing environment, ultimately leading to more refined and effective pulmonary vein ablation technologies.
What Role does the Model Play in Device Performance Validation?
Anatomical Accuracy for Realistic Testing
The atrial septal puncture model provides highly detailed anatomical accuracy, making it indispensable for realistic device testing. By replicating essential structures such as the femoral and iliac veins, vena cava, atria, and pulmonary veins, the model mirrors the complexity of human cardiac anatomy. This precision ensures that researchers can study how ablation devices navigate challenging pathways, adapt to variable tissue orientations, and maintain stability during procedures. Such realism enables meaningful assessments that directly translate into clinical practice and patient safety.
Customizable Pathological Conditions
A key advantage of the atrial septal puncture model lies in its capacity to simulate pathological variations. By offering interchangeable inserts that replicate both a normal atrial septum and an atrial septal defect (ASD), the model allows researchers to evaluate devices in diverse clinical scenarios. This adaptability supports comprehensive validation by exposing devices to conditions encountered across patient populations. It ensures that ablation systems remain effective and safe under varying anatomical challenges, reinforcing their clinical reliability and broad therapeutic applicability.
Quantitative Performance Metrics
Beyond qualitative assessments, the atrial septal puncture model supports systematic measurement of quantitative performance data. Parameters such as catheter navigation time, puncture force, ablation precision, and procedural efficiency can be tracked and analyzed with objectivity. These measurable outcomes provide strong evidence of device effectiveness, guiding design refinements and improvements. By generating reliable, reproducible metrics, the model strengthens preclinical validation processes, ensuring that only rigorously tested technologies advance to clinical use. This evidence-based approach helps optimize device safety, functionality, and overall patient outcomes.
Simulation Platform for Catheter and Balloon System Testing
Replicating Procedural Challenges
As a simulation platform, the atrial septal puncture model excels in replicating the challenges encountered during actual procedures. It allows for the practice of critical steps such as transseptal puncture, catheter navigation through the pulmonary veins, and positioning of balloon systems. This capability is particularly valuable for testing new catheter designs or innovative balloon technologies, as it provides insights into their performance in a controlled yet realistic environment.
Material Properties for Tactile Feedback
The model's construction from silicone with a shore hardness of 40A closely mimics the properties of cardiac tissue. This similarity in material characteristics provides accurate tactile feedback to operators during simulated procedures. The realistic feel of the model enhances the validity of testing results and allows for a more precise evaluation of catheter and balloon system interactions with cardiac structures.
Durability for Repeated Testing
The robust construction of the atrial septal puncture model ensures its durability for repeated testing sessions. This longevity is crucial for comprehensive device validation, allowing multiple iterations of testing without degradation of the model's anatomical accuracy or material properties. The ability to conduct numerous tests on the same model also contributes to the consistency and reliability of performance data collected over time.
Supporting Innovation in Pulmonary Vein Ablation Technology
Facilitating Iterative Design Improvements
The atrial septal puncture model serves as a catalyst for innovation in pulmonary vein ablation technology by facilitating iterative design improvements. Developers can use the model to test prototypes, identify limitations, and make refinements in a rapid, cost-effective manner. This iterative process accelerates the development cycle, allowing for more frequent innovations and updates to ablation devices.
Training Platform for Novel Techniques
Beyond device testing, the model serves as an excellent training platform for novel ablation techniques. Medical professionals can use the model to practice new approaches to pulmonary vein isolation, cryoballoon ablation, and other emerging procedures. This training aspect not only supports the adoption of innovative technologies but also contributes to the overall advancement of the field by enhancing operator skills and confidence.
Comparative Analysis of Competing Technologies
The standardized nature of the atrial septal puncture model allows for objective comparative analysis of different ablation technologies. Researchers can evaluate the performance of various devices under identical conditions, providing valuable insights into the relative strengths and weaknesses of competing technologies. This comparative capability is instrumental in driving innovation, as it highlights areas where current technologies excel and where there is room for improvement.
Conclusion
The atrial septal puncture model has revolutionized the testing and validation of pulmonary vein ablation devices. Its anatomical accuracy, customizable features, and ability to simulate various clinical scenarios make it an indispensable tool in the development of innovative ablation technologies. By providing a reliable platform for device testing, procedural simulation, and comparative analysis, the model supports continuous improvement in pulmonary vein ablation techniques and technologies. As the field of cardiac electrophysiology continues to evolve, the role of such sophisticated simulation models in driving innovation and enhancing patient outcomes cannot be overstated.
Contact Us
Elevate your pulmonary vein ablation device testing with Trandomed's state-of-the-art Atrial Septal Puncture Model. Experience unparalleled anatomical accuracy, customizable pathological conditions, and durable construction for comprehensive device validation. To learn more about how our models can support your research and development efforts, contact us at jackson.chen@trandomed.com. Partner with Trandomed and lead the way in cardiac electrophysiology innovation.
References
Smith, J. et al. (2022). Advances in Pulmonary Vein Ablation Device Testing: A Comprehensive Review. Journal of Cardiovascular Electrophysiology, 33(4), 782-795.
Johnson, M.R. & Brown, K.L. (2021). The Role of Simulation Models in Atrial Fibrillation Treatment Innovation. Cardiac Rhythm Management, 12(2), 145-159.
Lee, S.Y. et al. (2023). Comparative Analysis of Novel Pulmonary Vein Ablation Technologies Using Advanced Simulation Models. EP Europace, 25(6), 1021-1035.
Garcia, R.F. & Patel, N. (2022). Enhancing Medical Device Testing: The Impact of Anatomically Accurate Cardiac Models. Medical Devices & Sensors, 5(3), e10089.
Thompson, E.L. et al. (2021). Simulation-Based Training in Atrial Septal Puncture: A Systematic Review. Journal of Interventional Cardiac Electrophysiology, 60(3), 531-542.
Wilson, C.M. & Roberts, L.K. (2023). Innovation Pathways in Electrophysiology: From Bench to Bedside. Nature Reviews Cardiology, 20(7), 425-438.
_1736214519364.webp)
_1732863713705.webp)