How Does Simulation Reduce Risks in High-Stakes Procedures?
Minimizing Patient Exposure to Potential Complications
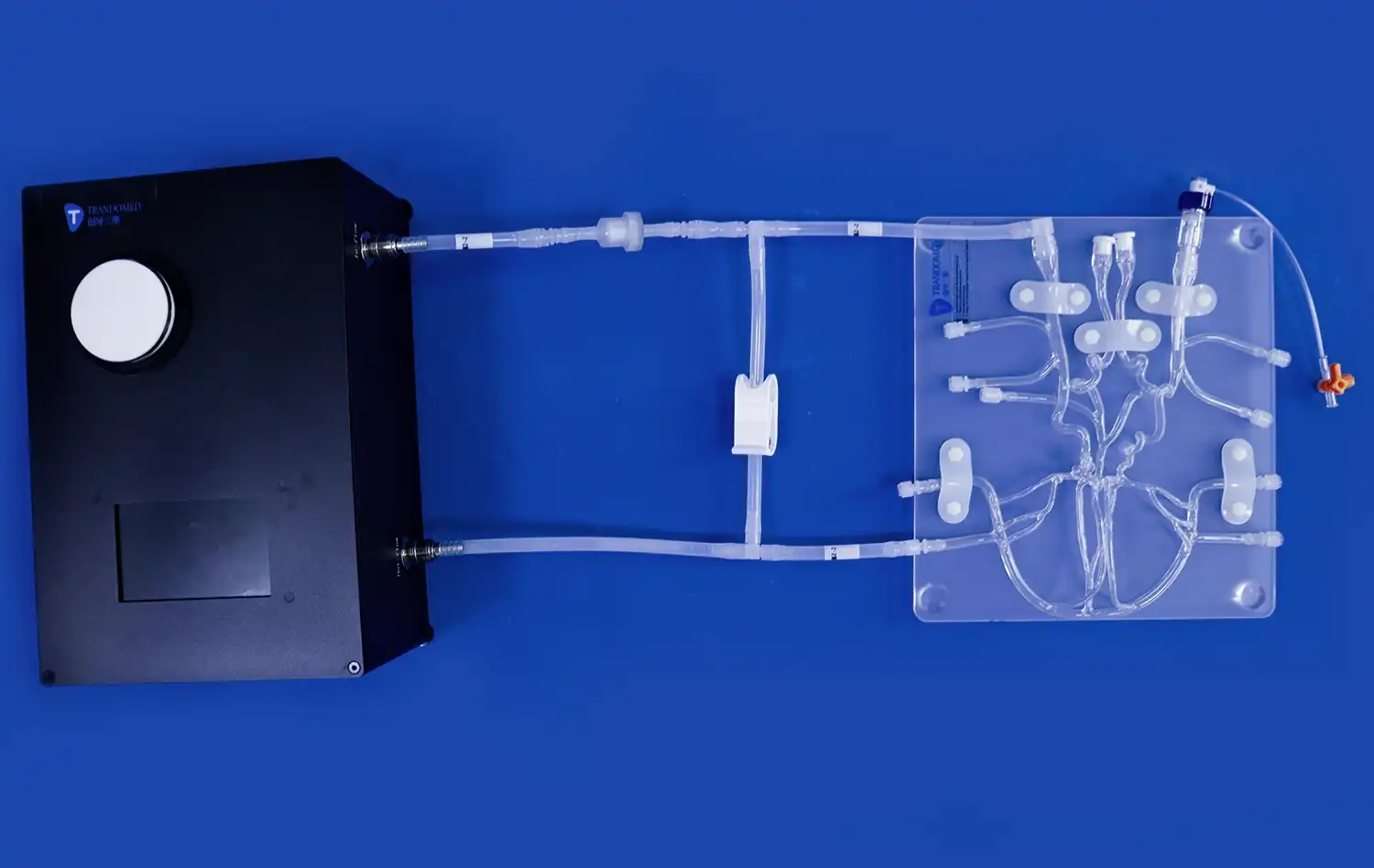
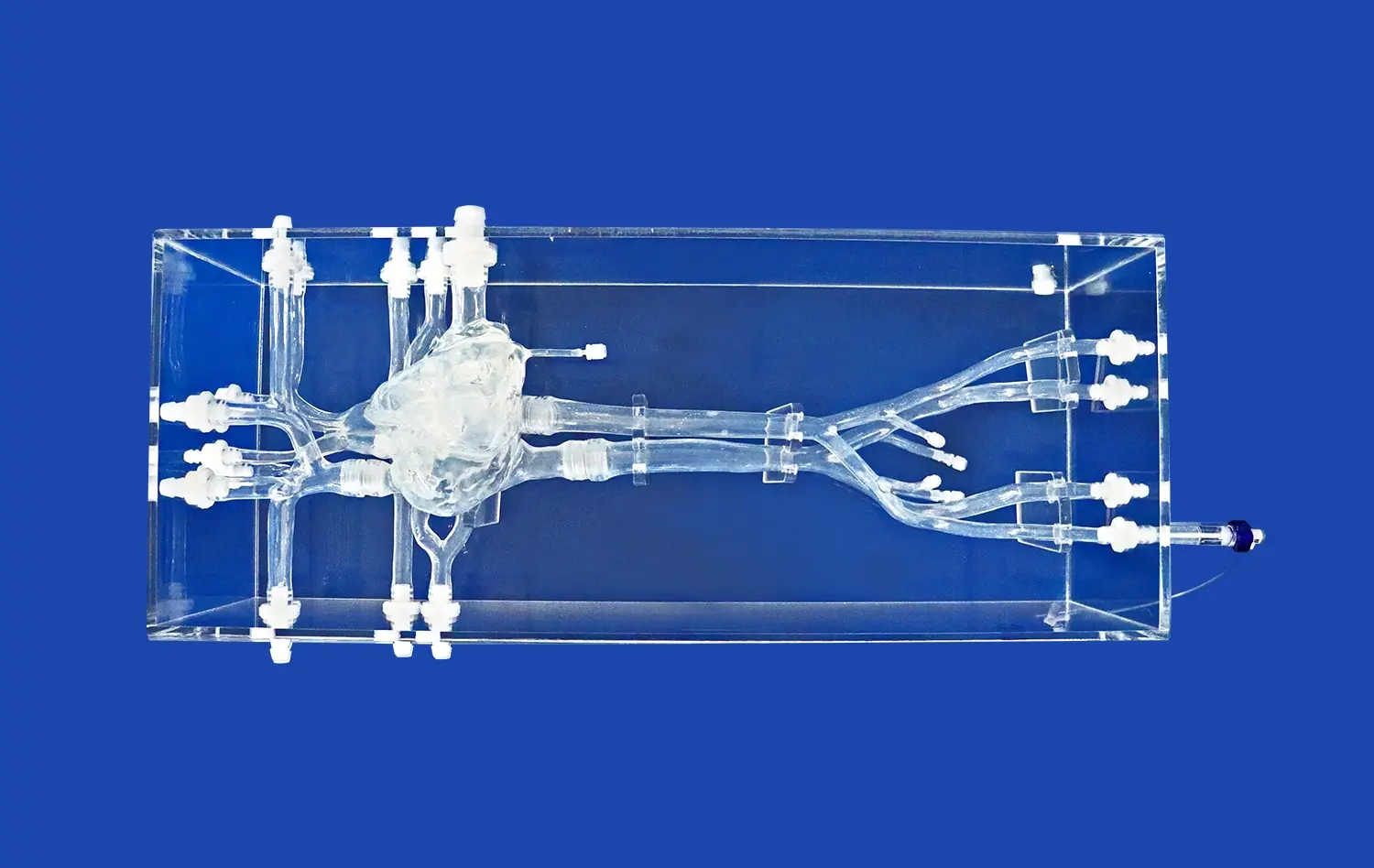
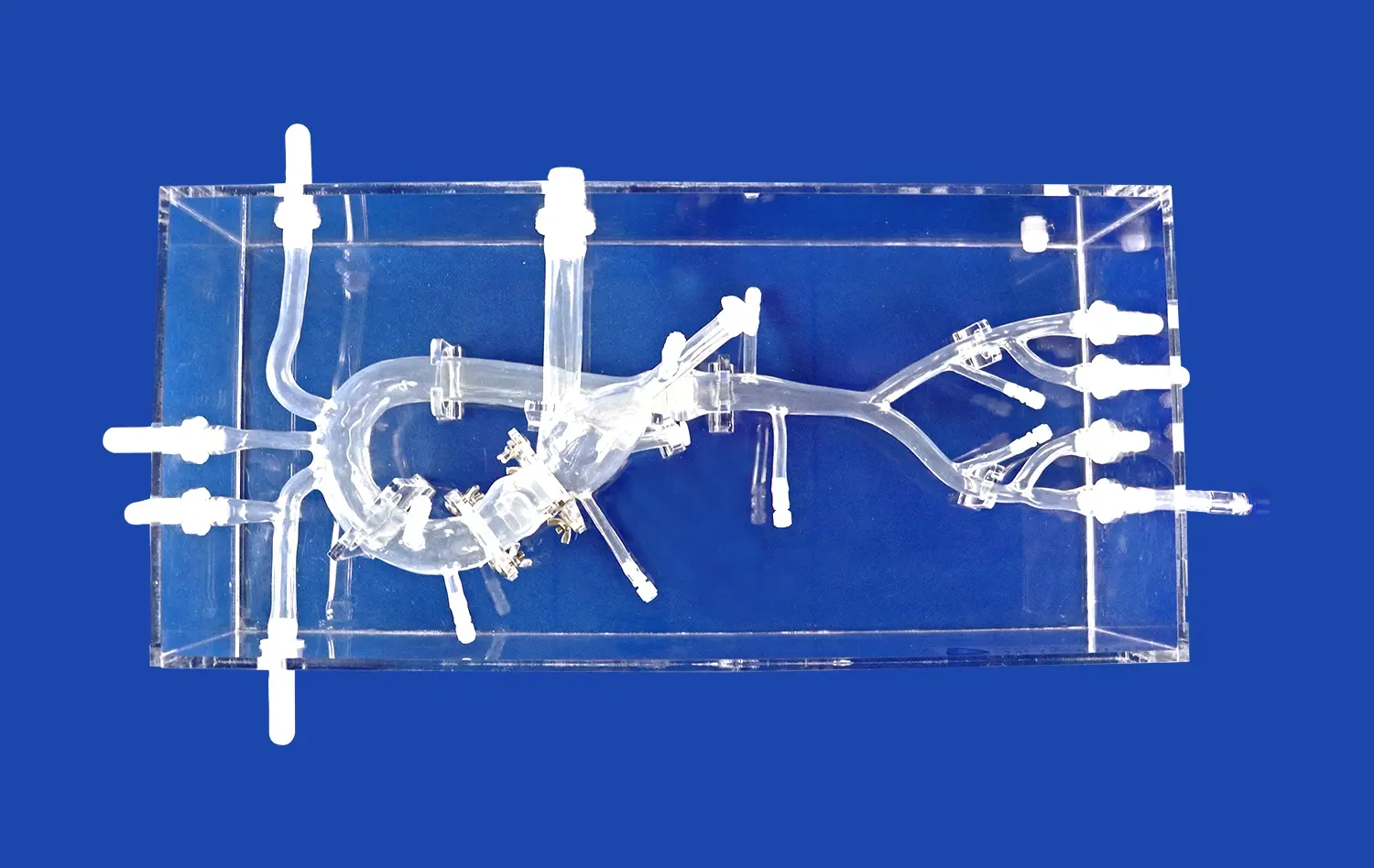
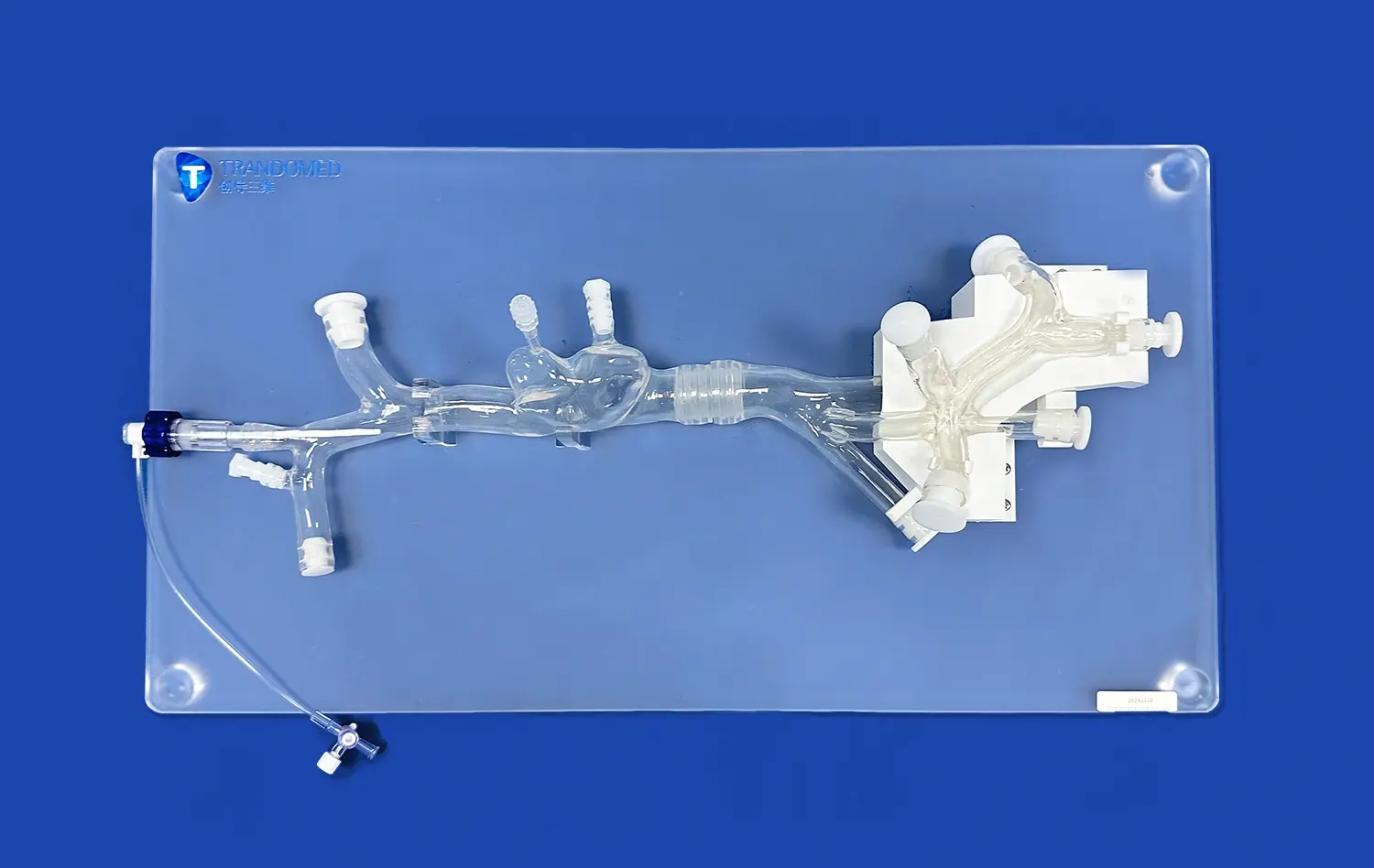
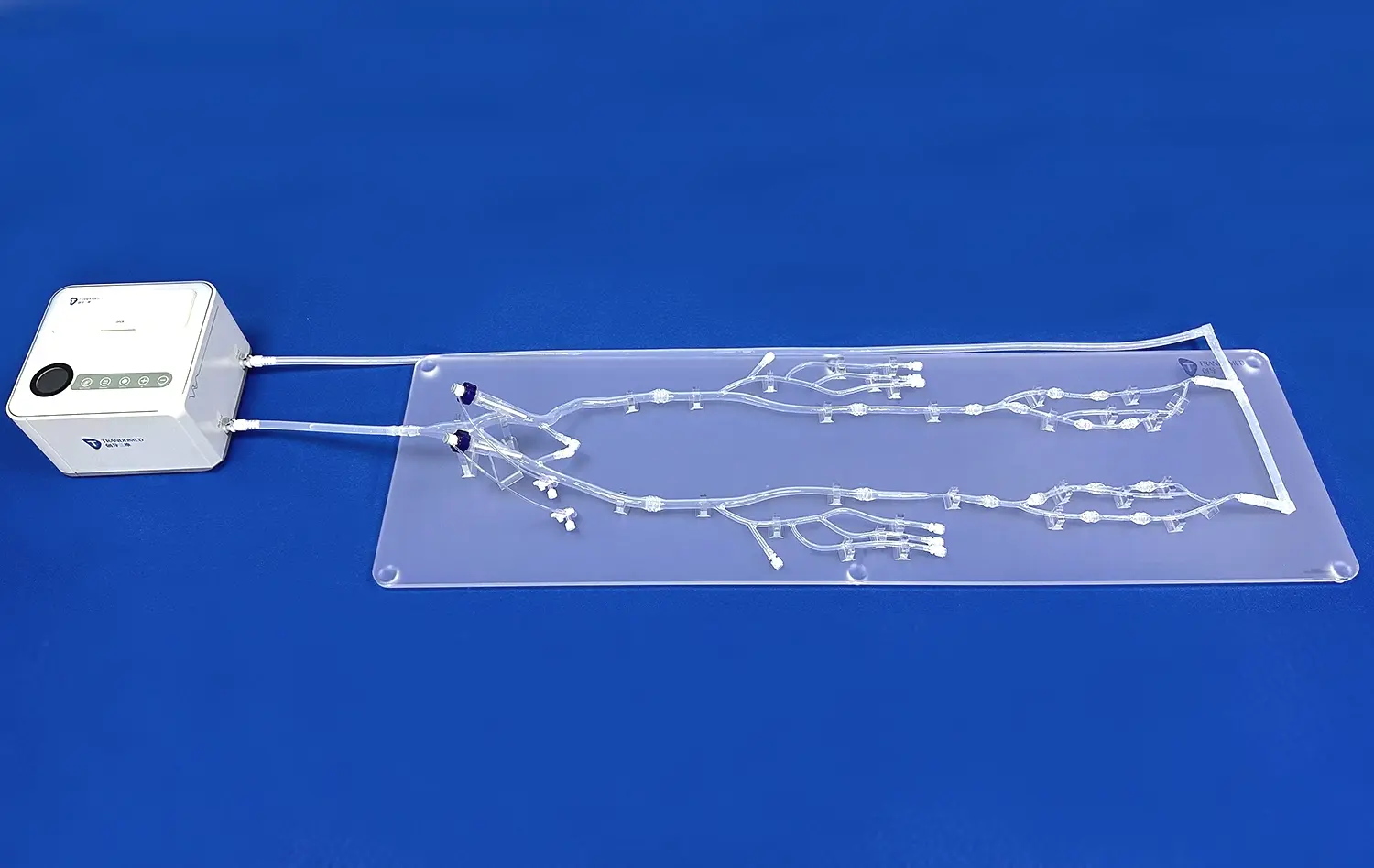
ERCP simulators play a crucial role in reducing risks associated with high-stakes procedures. By providing a realistic training environment, these simulators allow medical professionals to practice complex techniques without exposing patients to potential harm. The ERCP simulator II, for instance, replicates the intricate anatomy of the biliary and pancreatic ducts with remarkable accuracy. This level of detail enables trainees to familiarize themselves with various anatomical variations and potential challenges they might encounter during real procedures.
Enhancing Procedural Proficiency Through Repetition
One of the key advantages of simulation-based training is the ability to repeat procedures multiple times. Unlike real-life scenarios where each ERCP procedure is unique and irreversible, simulators allow for unlimited attempts. This repetition is crucial for developing muscle memory and refining techniques. The ERCP simulator II offers various scenarios and difficulty levels, allowing trainees to progressively build their skills from basic to advanced procedures. This graduated approach ensures that when faced with actual patients, healthcare professionals are well-prepared and confident in their abilities.
Creating a Low-Stress Learning Environment
High-stakes procedures can be stressful, especially for novice practitioners. ERCP simulators provide a low-stress environment where trainees can learn at their own pace without the pressure of real-time patient care. This relaxed atmosphere encourages experimentation and allows for mistakes, which are valuable learning opportunities. The ERCP simulator II, with its realistic tactile feedback and visual representations, creates an immersive experience that closely mimics real-world scenarios while eliminating the anxiety associated with potential patient harm.
Role of Replaceable Duct Models in Safe Operational Practice
Customizable Pathological Scenarios
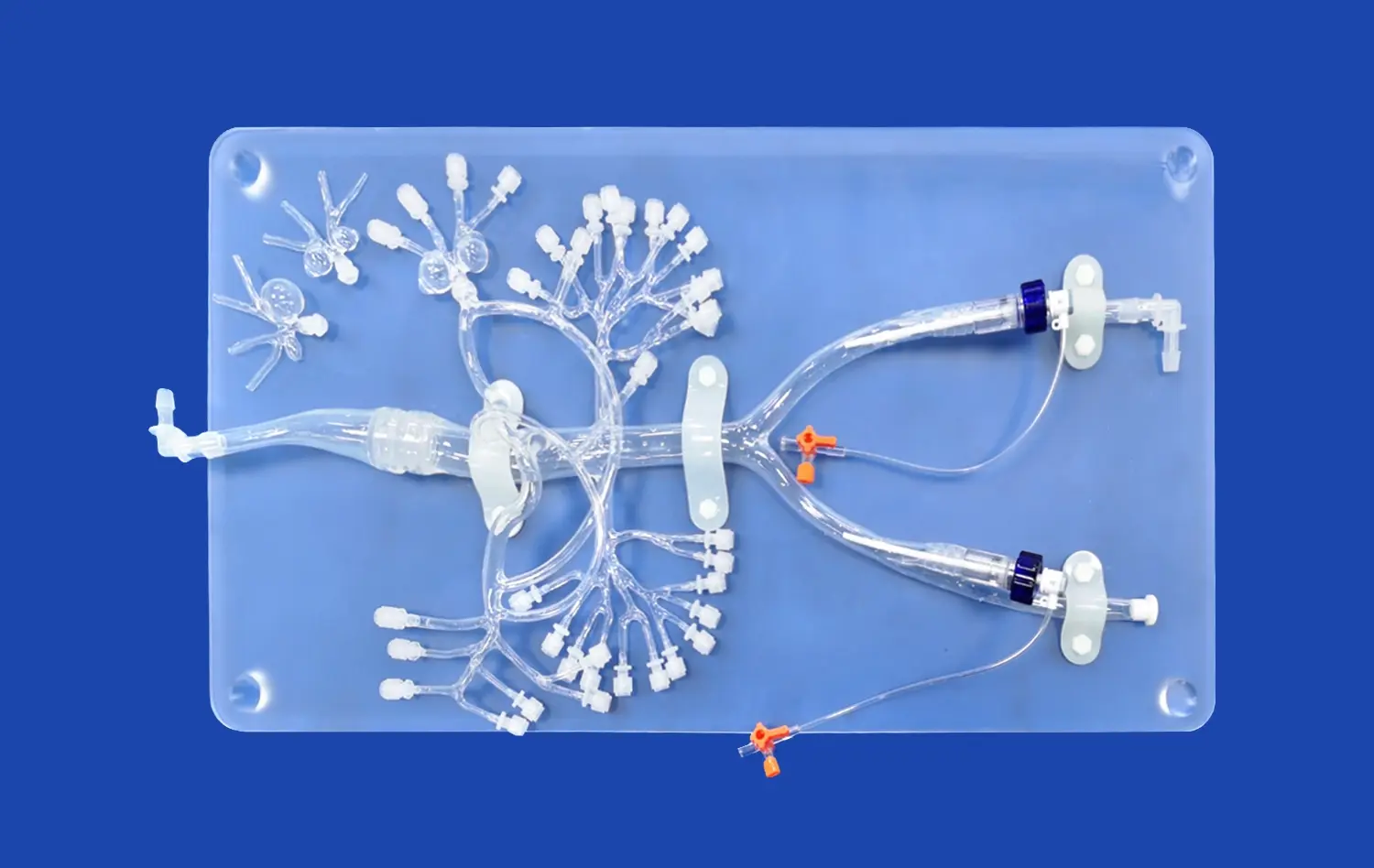
The ERCP simulator II features replaceable duct models that significantly enhance the training experience. These interchangeable components allow educators to create various pathological scenarios, mimicking different clinical conditions. From common bile duct stones to pancreatic tumors, trainees can encounter a wide range of cases. This versatility ensures that healthcare professionals are prepared for diverse situations they may face in their practice. The ability to swap out duct models also means that the simulator can be easily updated to reflect new pathological findings or rare conditions, keeping the training current and comprehensive.
Cost-Effective Skill Development
Replaceable duct models offer a cost-effective solution for medical institutions. Instead of purchasing multiple simulators for different scenarios, a single ERCP simulator II can be adapted to various training needs. This flexibility not only reduces the initial investment but also allows for ongoing updates and improvements. As medical knowledge advances, new duct models can be introduced, ensuring that the training remains cutting-edge without the need for complete system overhauls. This approach aligns with the sustainable practices of modern healthcare education, maximizing resources while providing high-quality training.
Facilitating Targeted Practice Sessions
The replaceable duct models in the ERCP simulator II enable targeted practice sessions. Instructors can focus on specific techniques or challenging anatomical variations by selecting appropriate duct models. This targeted approach allows for more efficient training, as learners can concentrate on areas that require improvement. For instance, a trainee struggling with stone extraction can practice repeatedly on a duct model simulating choledocholithiasis. This level of specificity in training is difficult to achieve with traditional methods and contributes significantly to the development of specialized skills.
Tracking Progress and Competency Without Patient Exposure
Objective Performance Metrics
One of the most significant advantages of the ERCP simulator II is its ability to provide objective performance metrics. Unlike subjective evaluations in real-world scenarios, the simulator offers quantifiable data on various aspects of the procedure. This includes metrics such as procedure time, accuracy of tool placement, and success rates in different scenarios. These objective measurements allow for a standardized assessment of competency, ensuring that all trainees meet the required skill levels before progressing to patient care. The data-driven approach also helps identify areas for improvement, enabling targeted feedback and personalized learning plans.
Longitudinal Skill Assessment
The ERCP simulator II facilitates longitudinal skill assessment, tracking a trainee's progress over time. This feature is particularly valuable in medical education, where the development of expertise is a gradual process. By regularly practicing on the simulator, learners can see their improvement in various aspects of the procedure. This visual representation of progress serves as a powerful motivator and helps maintain engagement in the learning process. Additionally, the ability to review past performance and compare it with current skills allows for a comprehensive understanding of one's growth trajectory.
Simulating Rare and Complex Cases
In real-world practice, exposure to rare or complex ERCP cases may be limited, especially for trainees. The ERCP simulator II bridges this gap by offering scenarios that mimic these uncommon situations. This exposure is crucial for developing a well-rounded skill set and preparing healthcare professionals for challenging cases they might encounter in their careers. By practicing on simulated rare cases, trainees can build confidence and competence without the risks associated with learning on actual patients. This approach ensures that when faced with similar situations in real life, practitioners are better equipped to handle them effectively.
Conclusion
The ERCP simulator II represents a significant advancement in medical training, offering a safe, effective, and comprehensive approach to learning complex endoscopic procedures. By providing a realistic environment for practice, it minimizes risks to patients while maximizing learning opportunities for healthcare professionals. The use of replaceable duct models and advanced tracking systems ensures that training remains relevant, targeted, and measurable. As medical education continues to evolve, tools like the ERCP simulator II will play an increasingly crucial role in shaping competent and confident healthcare practitioners, ultimately leading to improved patient outcomes and safety.
Contact Us
To learn more about how Trandomed's ERCP simulator II can revolutionize your medical training program and enhance patient safety, contact us at jackson.chen@trandomed.com. Discover the benefits of cutting-edge simulation technology and take the first step towards safer, more effective ERCP training today.