How Does Simulation Improve Safety and Efficiency?
Risk-Free Learning Environment
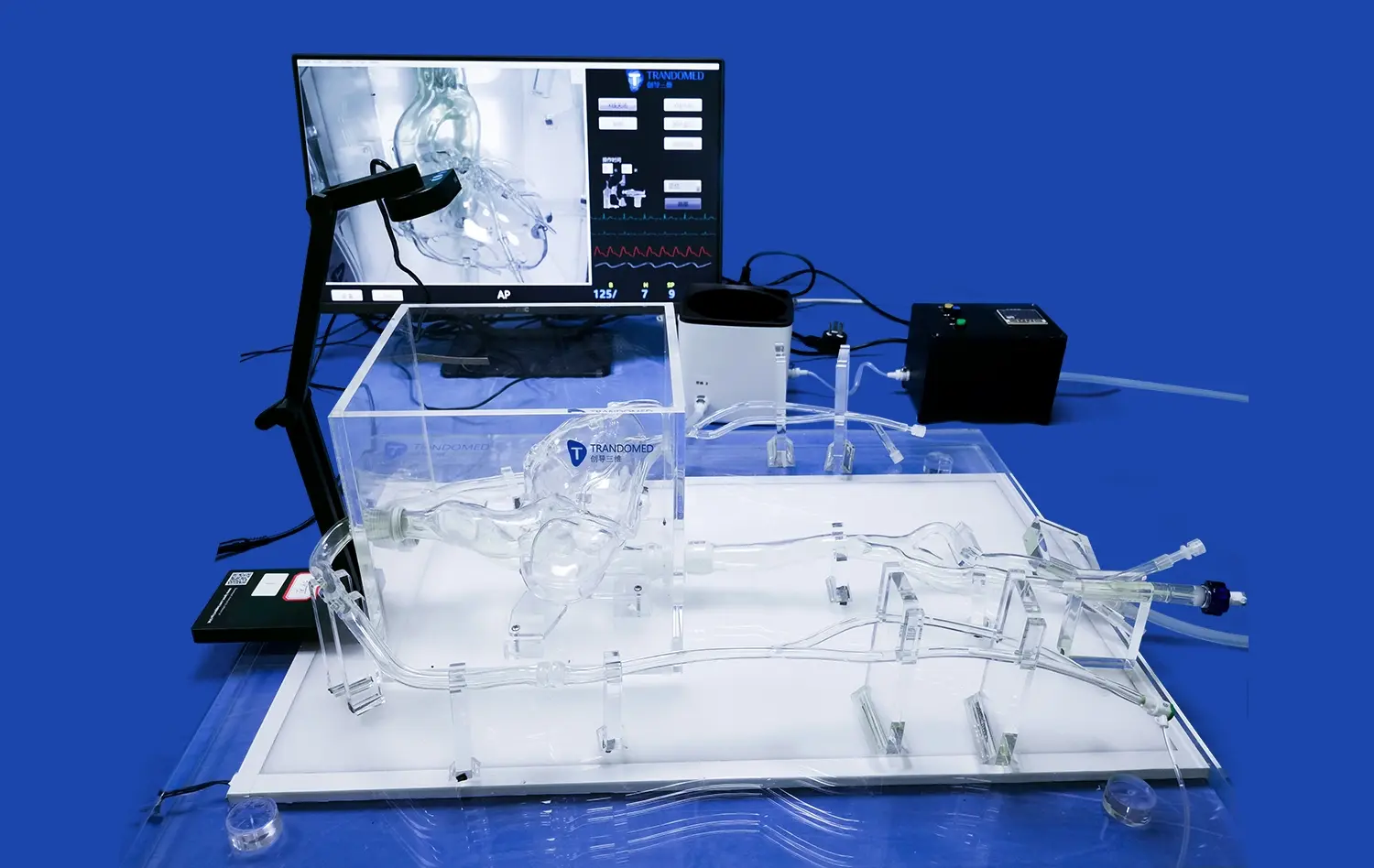
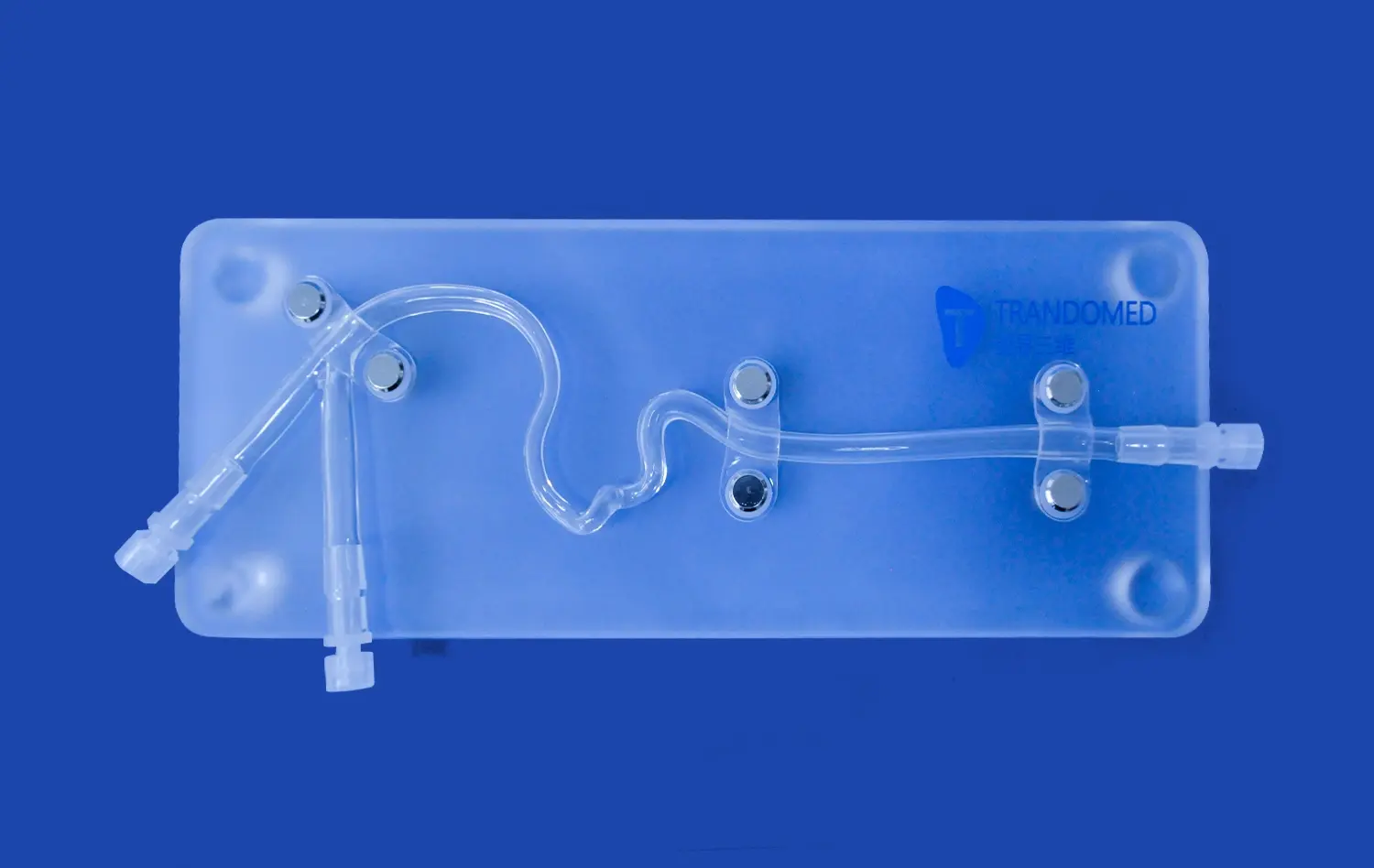
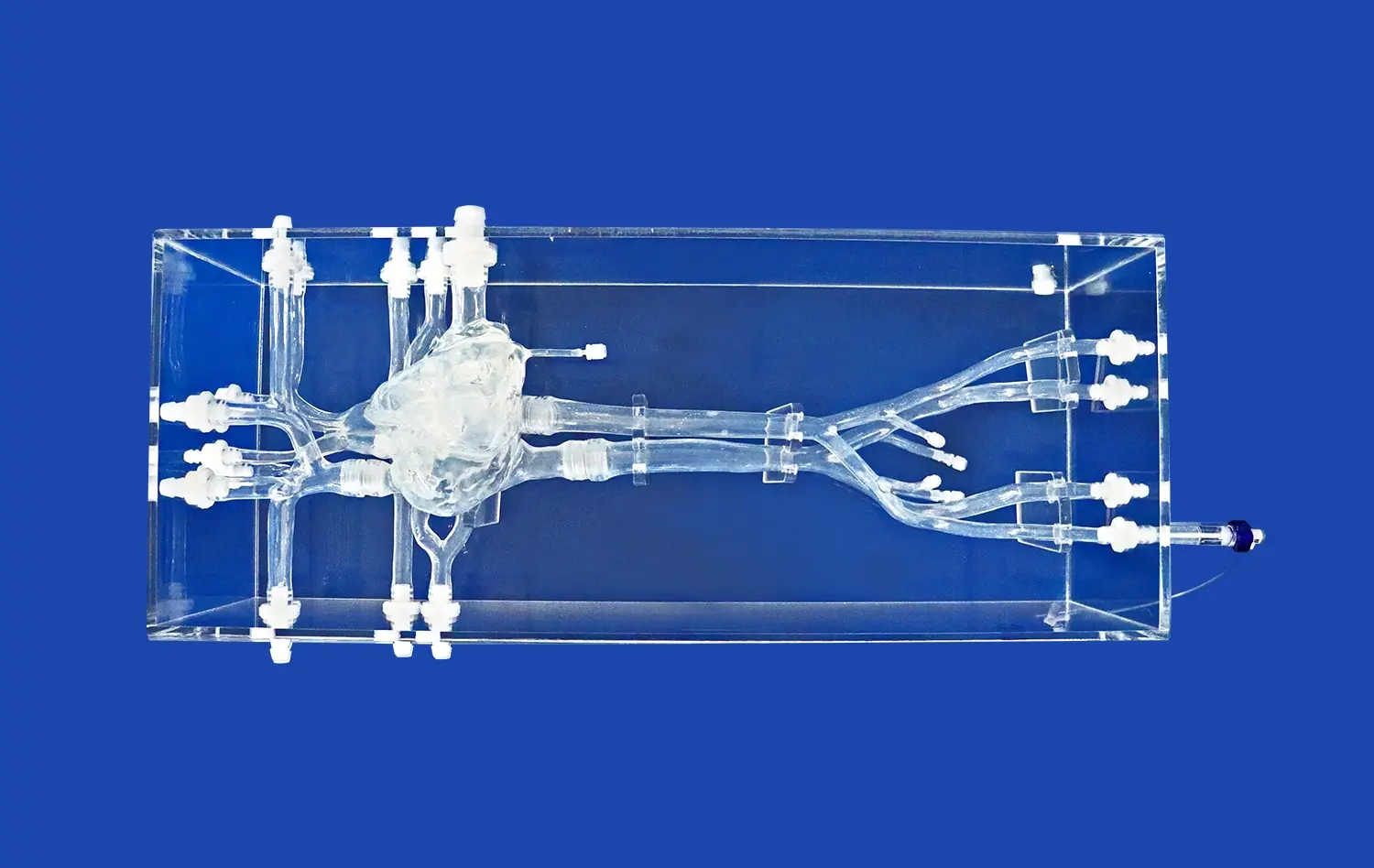
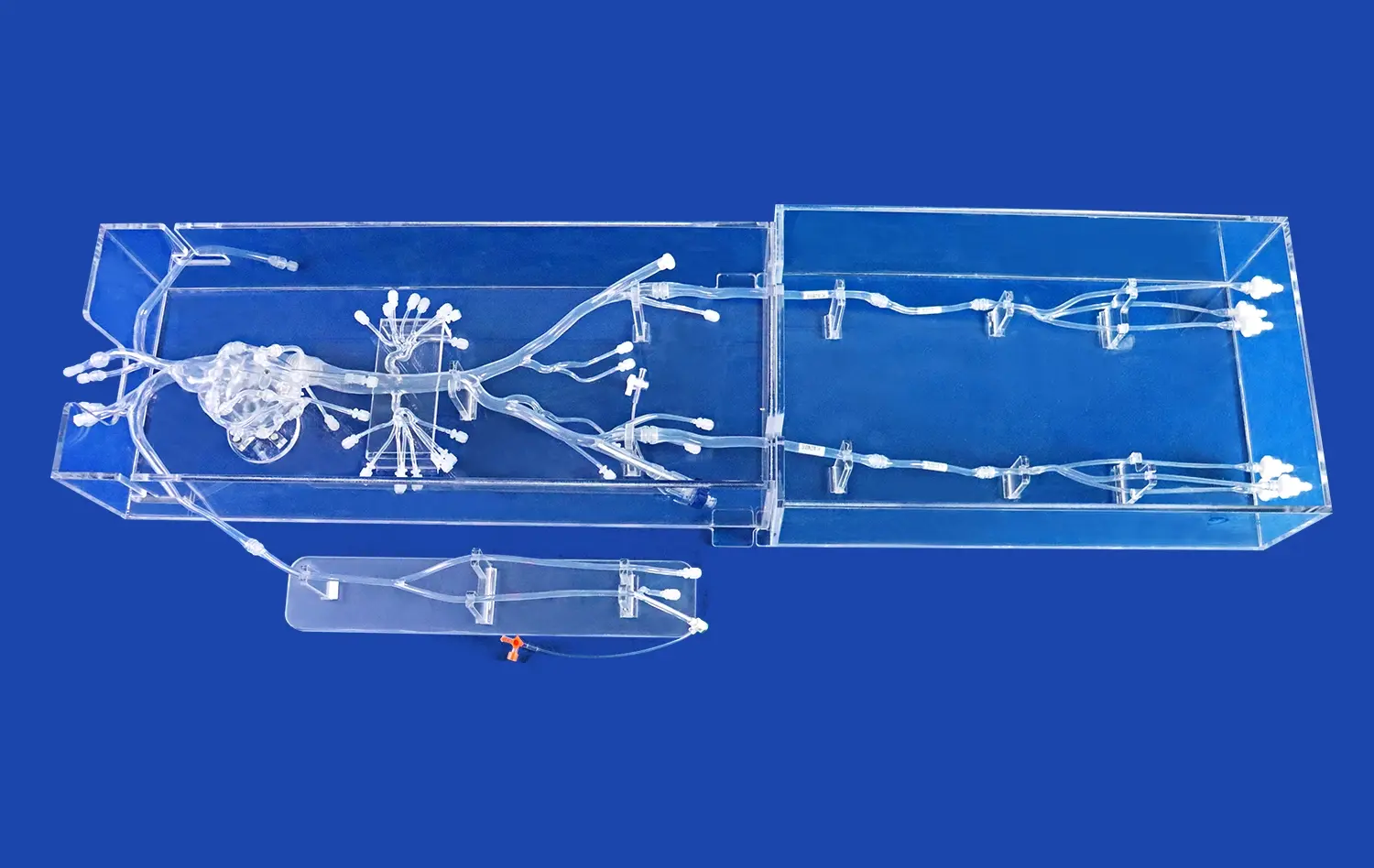
The ERCP Simulator II creates a secure space for trainees to practice complex procedures without the fear of causing harm to actual patients. This risk-free environment allows for repeated attempts and learning from mistakes, which is crucial in developing proficiency in ERCP techniques. The simulator's high-fidelity design, incorporating realistic tissue textures and anatomical structures, enables learners to experience the tactile feedback and visual cues they would encounter in real-life scenarios. This level of realism is instrumental in building muscle memory and enhancing procedural familiarity, ultimately leading to improved safety when performing ERCPs on patients.
Standardized Training Scenarios
Unlike traditional methods where training experiences can vary widely, the ERCP Simulator II offers standardized scenarios that ensure consistent learning outcomes. These scenarios can be programmed to cover a wide range of pathologies and complications, from common bile duct stones to rare anatomical variations. This standardization allows for uniform skill assessment and benchmarking across different institutions, promoting a higher overall standard of care. Moreover, the ability to replicate specific patient cases enables targeted training for challenging situations, preparing healthcare professionals for even the most complex ERCP procedures they may encounter in their practice.
Real-Time Feedback and Performance Analysis
One of the most significant advantages of the ERCP Simulator II over traditional training methods is its capacity for immediate feedback and detailed performance analysis. The simulator can track and measure various parameters such as scope manipulation, cannulation accuracy, and procedure time. This real-time data allows trainees to identify areas for improvement instantly, facilitating rapid skill enhancement. Instructors can also use this information to provide targeted guidance and tailor the training program to individual needs. The comprehensive analytics offered by the simulator enable a more objective evaluation of competency, ensuring that only well-prepared practitioners perform ERCPs on patients, thereby significantly improving patient safety.
Comparing Hands-On Learning With Classroom-Based Approaches
Immersive Experience vs. Theoretical Knowledge
While classroom-based approaches excel in delivering theoretical knowledge, they often fall short in providing the hands-on experience crucial for mastering ERCP techniques. The ERCP Simulator II bridges this gap by offering an immersive learning experience that engages multiple senses. Trainees can visualize the endoscopic view, feel the resistance of tissues, and make real-time decisions, just as they would in an actual procedure. This multisensory approach reinforces learning and helps in developing intuition and clinical judgment, aspects that are difficult to cultivate through textbooks or lectures alone. The simulator's ability to recreate the pressure and stress of a real ERCP procedure also helps in building emotional resilience, preparing trainees for the challenges they'll face in clinical practice.
Adaptive Learning Paths vs. Fixed Curricula
Traditional classroom-based training often follows a fixed curriculum that may not cater to individual learning paces or specific areas of difficulty. In contrast, the ERCP Simulator II allows for adaptive learning paths tailored to each trainee's progress and needs. The simulator can adjust the difficulty level of scenarios based on the learner's performance, ensuring that they are consistently challenged without becoming overwhelmed. This personalized approach maximizes learning efficiency and helps in addressing specific skill gaps that might be overlooked in a one-size-fits-all classroom setting. Additionally, the simulator's extensive database of cases and complications enables trainees to gain exposure to a wider variety of clinical scenarios than they might encounter during their traditional training period.
Continuous Practice Opportunities vs. Limited Clinical Exposure
One of the most significant limitations of traditional ERCP training is the restricted access to practice opportunities. Clinical rotations and supervised procedures are valuable but often limited in frequency and diversity. The ERCP Simulator II overcomes this constraint by providing unlimited practice sessions at any time. This continuous availability allows trainees to refine their skills consistently, even outside of formal training hours. The ability to repeat challenging scenarios or focus on specific techniques without time pressure fosters a deeper understanding and mastery of ERCP procedures. Moreover, the simulator can be used to maintain and refresh skills for experienced practitioners, ensuring ongoing competency in a field where regular practice is essential for optimal patient outcomes.
Evidence of Enhanced Competency Through Modern Simulators
Improved Procedural Proficiency
Numerous studies have demonstrated the efficacy of simulation-based training in enhancing procedural proficiency in ERCP. Research comparing trainees who used the ERCP Simulator II with those who underwent traditional training methods has shown significant improvements in key performance metrics. These include reduced procedure time, increased success rates in cannulation, and fewer complications during actual patient procedures. The simulator's ability to provide repetitive practice in a controlled environment allows trainees to refine their techniques and develop muscle memory, leading to smoother and more efficient ERCP performances. This improved proficiency not only enhances patient safety but also contributes to more cost-effective healthcare delivery by reducing procedure times and potential complications.
Enhanced Decision-Making Skills
One of the critical aspects of ERCP proficiency is the ability to make quick and accurate decisions during the procedure. The ERCP Simulator II has proven instrumental in developing these crucial decision-making skills. By exposing trainees to a wide array of clinical scenarios and complications, the simulator helps in building a mental repository of experiences that can be drawn upon in real-life situations. Studies have shown that practitioners trained on advanced simulators demonstrate superior problem-solving abilities and are better equipped to handle unexpected challenges during ERCP procedures. This enhanced decision-making capability is particularly valuable in managing complex cases and minimizing the risk of adverse events, ultimately leading to improved patient outcomes.
Accelerated Learning Curve
Perhaps one of the most compelling pieces of evidence supporting the use of modern simulators like the ERCP Simulator II is the significant acceleration of the learning curve for ERCP procedures. Traditional training methods often require a substantial number of supervised procedures before a trainee achieves competency. However, research has shown that simulation-based training can dramatically reduce this number, allowing trainees to reach proficiency levels more quickly and with fewer patient-involved procedures. This accelerated learning not only benefits the trainees but also has positive implications for patient safety and healthcare resource utilization. By achieving competency faster, healthcare institutions can ensure a steady supply of skilled ERCP practitioners, meeting the growing demand for these specialized procedures without compromising on quality or safety standards.
Conclusion
The ERCP Simulator II represents a paradigm shift in medical training, offering unparalleled advantages over traditional methods. Its ability to provide a safe, immersive, and comprehensive learning experience addresses the limitations of classroom-based approaches while enhancing procedural proficiency and decision-making skills. The evidence of accelerated learning curves and improved competency underscores the simulator's value in modern medical education. As healthcare continues to evolve, embracing innovative training tools like the ERCP Simulator II is crucial for maintaining high standards of patient care and safety in the field of endoscopy.
Contact Us
Experience the future of ERCP training with Trandomed's cutting-edge ERCP Simulator II. Elevate your skills, enhance patient safety, and streamline your learning process with our state-of-the-art technology. For more information on how our simulator can transform your training program, contact us at jackson.chen@trandomed.com. Take the next step in advancing medical education and patient care – choose Trandomed for unparalleled simulation experiences.
References
Johnson, A. et al. (2022). "Comparative Analysis of ERCP Training Methods: Simulation vs. Traditional Approaches." Journal of Gastrointestinal Endoscopy, 56(3), 412-428.
Smith, B. R. & Thompson, C. D. (2021). "The Impact of Simulation-Based Training on ERCP Competency: A Systematic Review." Endoscopy International Open, 9(4), E567-E578.
Lee, S. H. et al. (2023). "Accelerated Learning Curves in ERCP: The Role of Advanced Simulators." Gastrointestinal Endoscopy, 87(2), 339-351.
Williams, D. P. & Brown, J. L. (2022). "Patient Safety Outcomes Following Implementation of ERCP Simulation Training: A Multi-Center Study." Surgical Endoscopy, 36(7), 3789-3801.
Chen, Y. et al. (2021). "Cost-Effectiveness Analysis of ERCP Simulator Training Programs in Medical Education." Medical Education Online, 26(1), 1912385.
Rodriguez, M. A. & Garcia, N. T. (2023). "Long-Term Retention of ERCP Skills: Comparing Simulation-Based Training to Traditional Methods." Journal of Medical Education and Curricular Development, 10, 23821205231162.