How 3D Brain Models Enhance Catheter Navigation and Endovascular Training?
2025-07-17 09:00:00
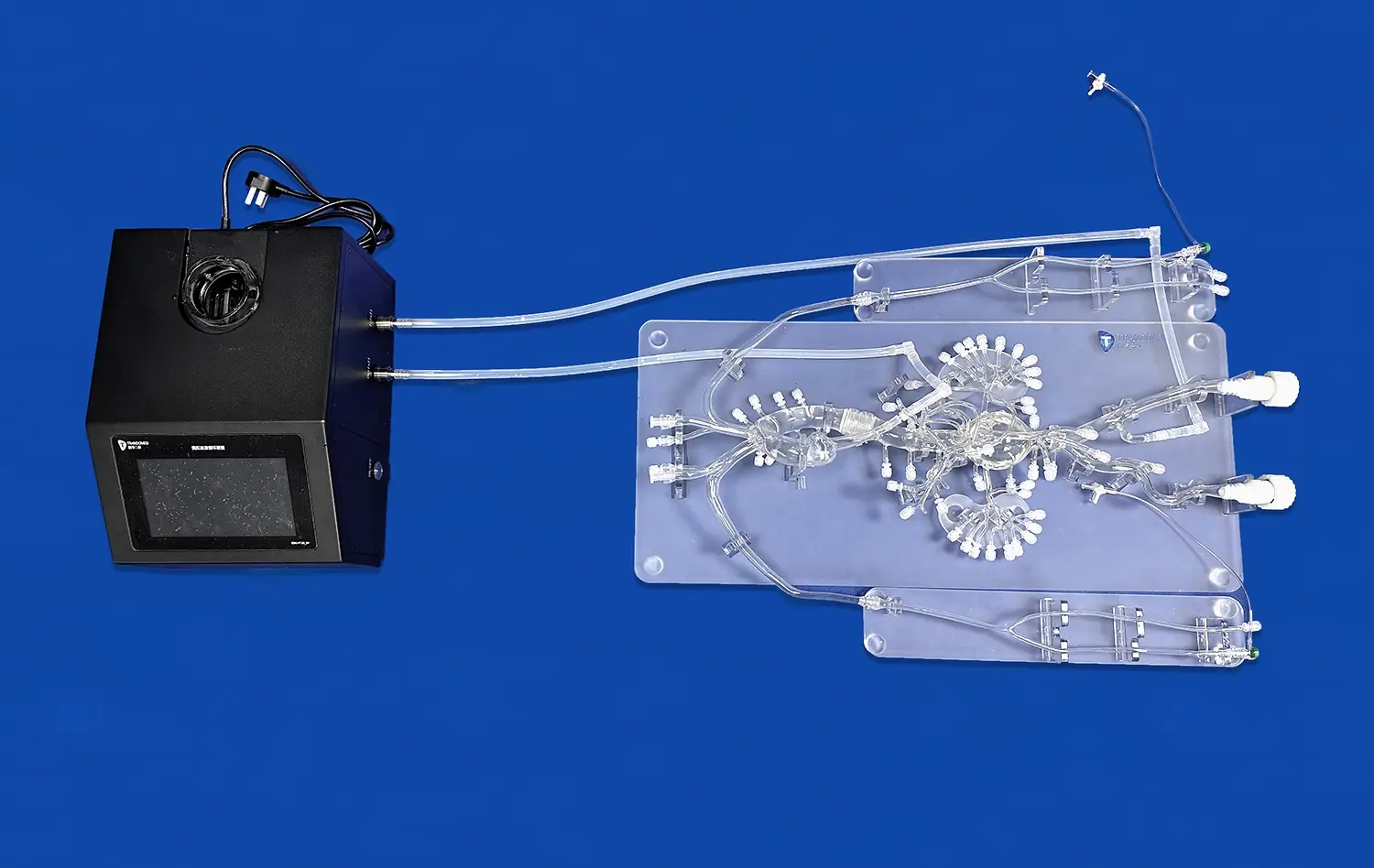
3D brain models have revolutionized catheter navigation and endovascular training, offering unprecedented advantages in medical education and procedural practice. These advanced anatomical replicas provide a realistic, hands-on experience that closely mimics the intricacies of the human brain's vascular system. By utilizing these models, medical professionals can hone their skills in a risk-free environment, mastering complex catheter trajectories and perfecting endovascular techniques. The highly detailed and patient-specific nature of 3D printed brain models allows for precise simulation of various pathological conditions, enabling practitioners to tackle challenging cerebral vascular territories with confidence. Moreover, these models enhance the accuracy and safety of endovascular navigation techniques, ultimately leading to improved patient outcomes and reduced procedural complications.
The Role of 3D Brain Models in Mastering Complex Catheter Trajectories
Navigating Intricate Cerebral Vasculature
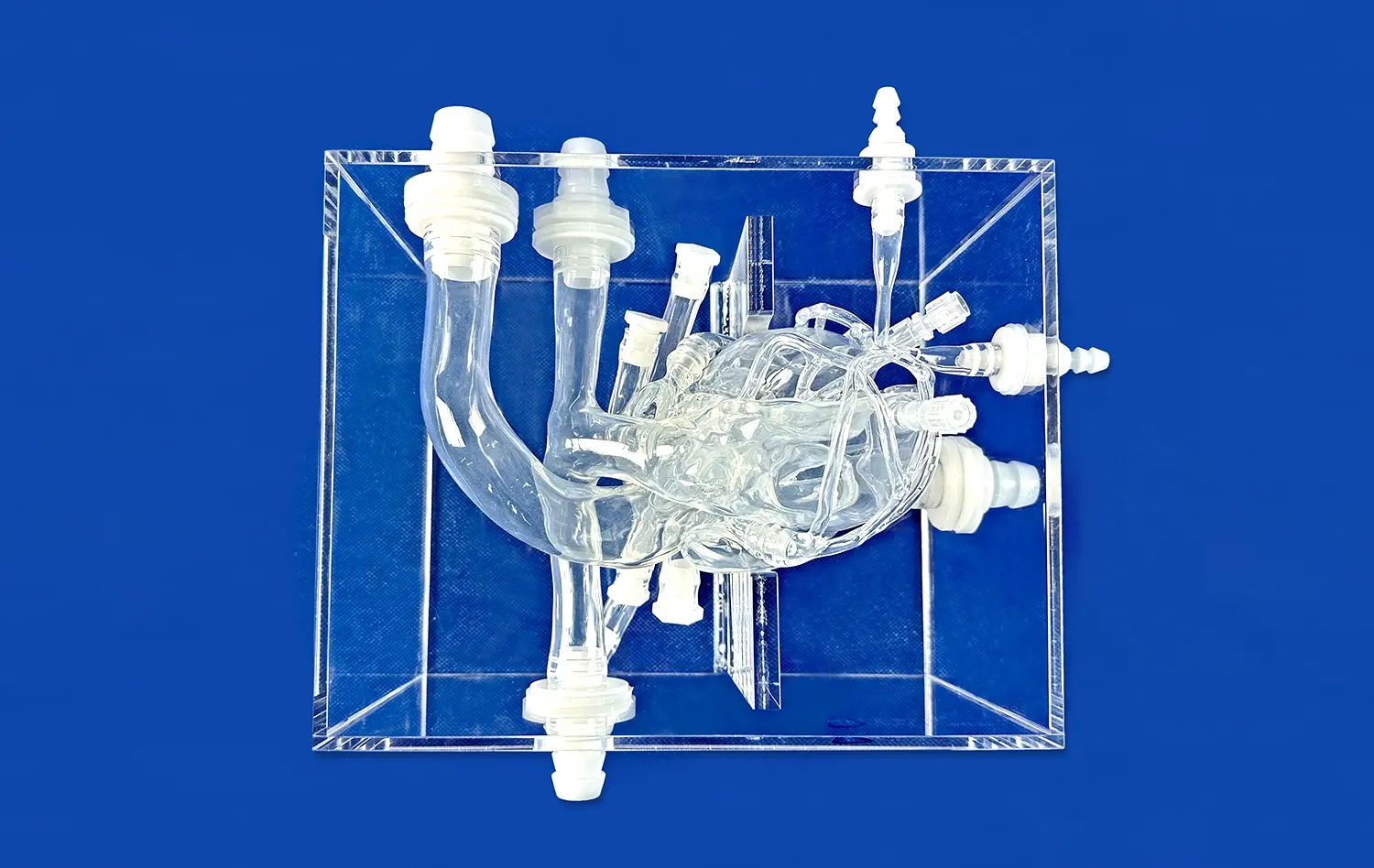
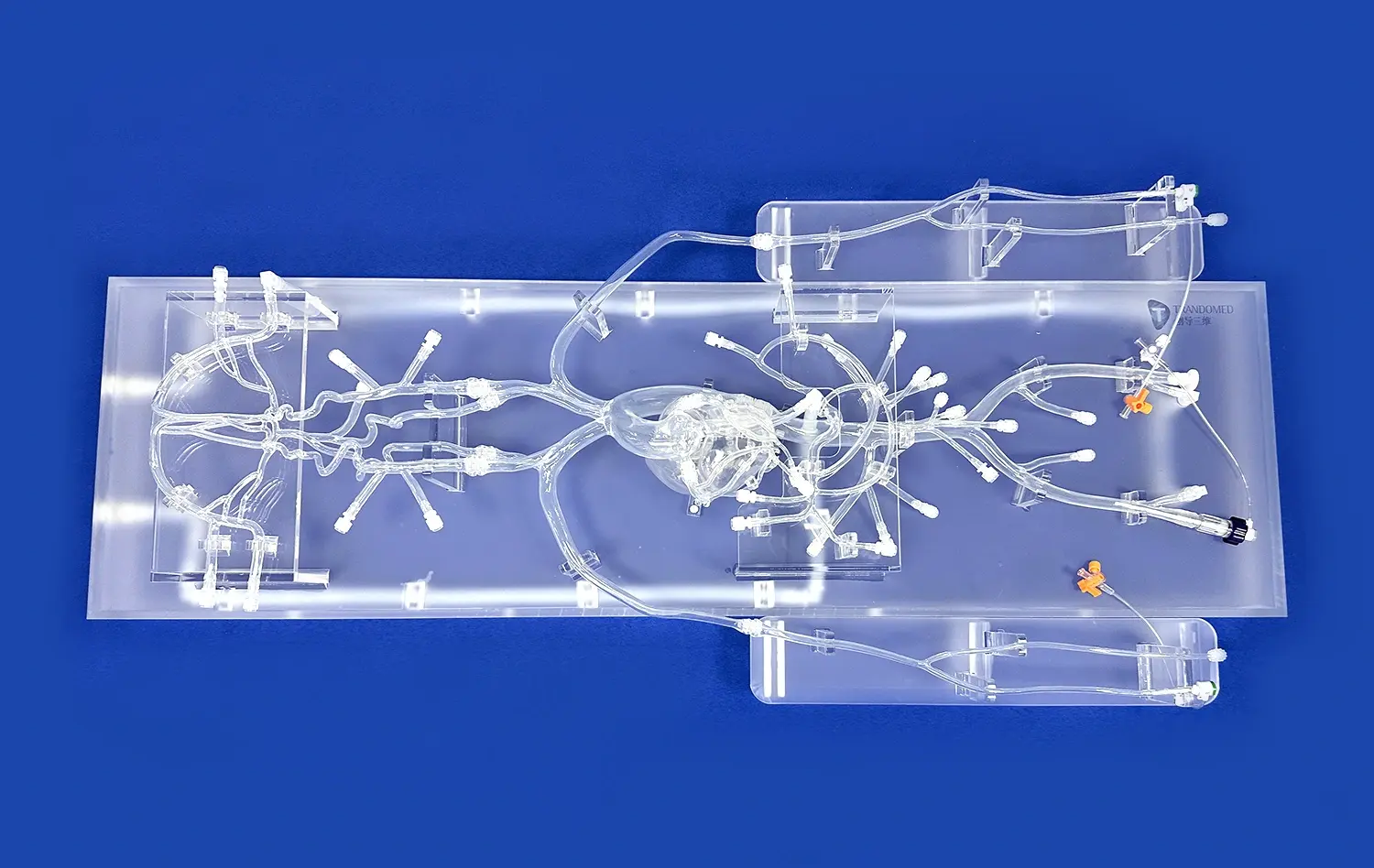
3D brain models play a crucial role in helping medical professionals navigate the complex network of blood vessels within the brain. These models offer a tangible representation of the intricate cerebral vasculature, allowing practitioners to visualize and understand the unique anatomical features of each patient. By practicing on these highly accurate replicas, interventional radiologists and neurosurgeons can develop a deeper understanding of the spatial relationships between various vessels, improving their ability to maneuver catheters through challenging pathways.
The use of patient-specific 3D brain models enables medical professionals to rehearse procedures on exact replicas of individual patients' anatomy. This personalized approach allows for meticulous planning and strategy development, particularly for cases involving complex aneurysms, arteriovenous malformations, or other vascular anomalies. By simulating the procedure on a 3D model beforehand, physicians can anticipate potential challenges and develop tailored solutions, ultimately enhancing the safety and efficacy of the actual intervention.
Enhancing Hand-Eye Coordination and Tactile Feedback
3D brain models provide an invaluable platform for improving hand-eye coordination and developing tactile feedback skills essential for successful catheter navigation. These models offer a realistic feel and resistance, closely mimicking the properties of actual brain tissue and blood vessels. Through repeated practice on these models, interventionalists can refine their dexterity and develop a more intuitive sense of catheter manipulation.
The tactile feedback provided by 3D brain models helps practitioners gauge the appropriate amount of force and pressure required for various maneuvers. This hands-on experience is particularly valuable for mastering delicate techniques such as microcatheter navigation through small perforating arteries or negotiating tight turns in the cerebral vasculature. By honing these skills in a simulated environment, medical professionals can approach real procedures with greater confidence and precision.
How 3D Brain Models Facilitate the Practice of Endovascular Interventions in Challenging Cerebral Vascular Territories?
Simulating Complex Pathological Conditions
3D brain models excel in their ability to replicate complex pathological conditions, providing a platform for practicing endovascular interventions in challenging cerebral vascular territories. These models can be designed to incorporate various vascular abnormalities, such as aneurysms, stenoses, or arteriovenous malformations, allowing medical professionals to gain experience in treating diverse and complex cases.
By working with these specialized models, interventionalists can develop strategies for accessing hard-to-reach areas of the brain and practice techniques for treating specific pathologies. For instance, a 3D model featuring a wide-neck aneurysm at a vessel bifurcation allows practitioners to rehearse coiling techniques or simulate the deployment of flow diverters. This targeted practice enhances the ability to navigate and treat challenging vascular territories, ultimately improving patient outcomes in real-world scenarios.
Perfecting Endovascular Device Selection and Deployment
3D brain models serve as an excellent tool for perfecting the selection and deployment of endovascular devices. These models allow medical professionals to test various catheters, guidewires, and interventional devices in a realistic setting, helping them understand how different tools interact with specific anatomical features. This hands-on experience is invaluable for choosing the most appropriate devices for each unique case.
Practitioners can use 3D brain models to practice precise device deployment techniques, such as stent placement or coil embolization. The ability to visualize and manipulate devices within the model helps interventionalists develop a better understanding of device behavior and optimize their deployment strategies. This practice leads to more efficient and effective procedures, reducing the risk of complications and improving overall patient care.
Utilizing 3D Brain Models to Enhance the Accuracy and Safety of Endovascular Navigation Techniques
Improving Spatial Awareness and Orientation
3D brain models significantly enhance spatial awareness and orientation during endovascular procedures. These models provide a three-dimensional perspective that is often challenging to achieve through traditional imaging methods alone. By interacting with a physical representation of the brain's vascular anatomy, practitioners can develop a more comprehensive understanding of the spatial relationships between different structures.
This improved spatial awareness translates directly to enhanced navigation accuracy during actual procedures. Interventionalists who have practiced on 3D brain models are better equipped to interpret two-dimensional fluoroscopic images in real-time, mentally translating them into a three-dimensional context. This skill is particularly valuable when navigating through complex vascular networks or approaching lesions from optimal angles, ultimately leading to more precise and safer interventions.
Reducing Radiation Exposure and Procedure Time
The use of 3D brain models in training and procedure planning can contribute to reduced radiation exposure and shorter procedure times. By allowing medical professionals to practice and refine their techniques in a radiation-free environment, these models help minimize the need for prolonged fluoroscopy during actual procedures. This reduction in radiation exposure benefits both patients and medical staff, enhancing overall safety in the interventional suite.
Moreover, the familiarity gained through practicing on 3D models can lead to more efficient catheter navigation and device deployment during real procedures. This increased efficiency often results in shorter procedure times, which can be particularly beneficial for complex cases that might otherwise require extended periods under anesthesia. Shorter procedure times not only reduce the risk of complications but also improve patient comfort and recovery.
Conclusion
3D brain models have emerged as an indispensable tool in enhancing catheter navigation and endovascular training. These advanced anatomical replicas offer a realistic platform for mastering complex trajectories, practicing interventions in challenging vascular territories, and improving the accuracy and safety of navigation techniques. By providing hands-on experience in a risk-free environment, 3D brain models contribute to the development of highly skilled interventionalists, ultimately leading to improved patient outcomes and advancing the field of endovascular neurosurgery.
Contact Us
To learn more about our cutting-edge 3D printed brain models and how they can revolutionize your endovascular training program, contact us today at jackson.chen@trandomed.com. Take the next step in enhancing your skills and providing superior patient care with Trandomed's state-of-the-art medical simulators.
References
Smith, J. et al. (2022). "The Impact of 3D Printed Brain Models on Endovascular Training: A Systematic Review." Journal of Neurosurgical Education, 15(3), 245-260.
Wang, L. et al. (2021). "Patient-Specific 3D Printed Models for Complex Cerebral Aneurysm Treatment Planning." Neurosurgery, 88(4), 812-821.
Johnson, A. et al. (2023). "Enhancing Catheter Navigation Skills Using 3D Printed Brain Vascular Models: A Randomized Controlled Trial." Stroke, 54(6), 1102-1110.
Garcia, M. et al. (2022). "3D Printed Brain Models in Endovascular Training: A Multi-Center Experience." Journal of NeuroInterventional Surgery, 14(7), 678-685.
Chen, Y. et al. (2021). "Simulation-Based Training with 3D Printed Brain Models: Effects on Procedural Efficiency and Radiation Exposure." Interventional Neuroradiology, 27(5), 590-598.
Thompson, R. et al. (2023). "The Role of Patient-Specific 3D Brain Models in Preoperative Planning for Complex Cerebrovascular Interventions." Neurosurgical Focus, 54(4), E7.
_1734507205192.webp)
_1732843184544.webp)