Aneurysm models have revolutionized neurosurgical training programs by providing a realistic, hands-on approach to learning complex cerebrovascular procedures. These sophisticated simulation tools allow neurosurgeons-in-training to practice critical skills in a safe, controlled environment before performing procedures on actual patients. By replicating the intricate anatomy of the brain's blood vessels, including the presence of aneurysms, these models enable trainees to develop spatial awareness, fine motor skills, and decision-making abilities crucial for successful neurosurgical interventions. The use of aneurysm simulators in training programs has been shown to significantly improve surgical outcomes, reduce procedural times, and enhance overall patient safety. As medical education continues to evolve, the integration of high-fidelity aneurysm models into neurosurgical curricula has become an indispensable component in preparing the next generation of skilled neurosurgeons.
Core Components of Neurosurgical Skill Development
Anatomical Precision and Spatial Awareness
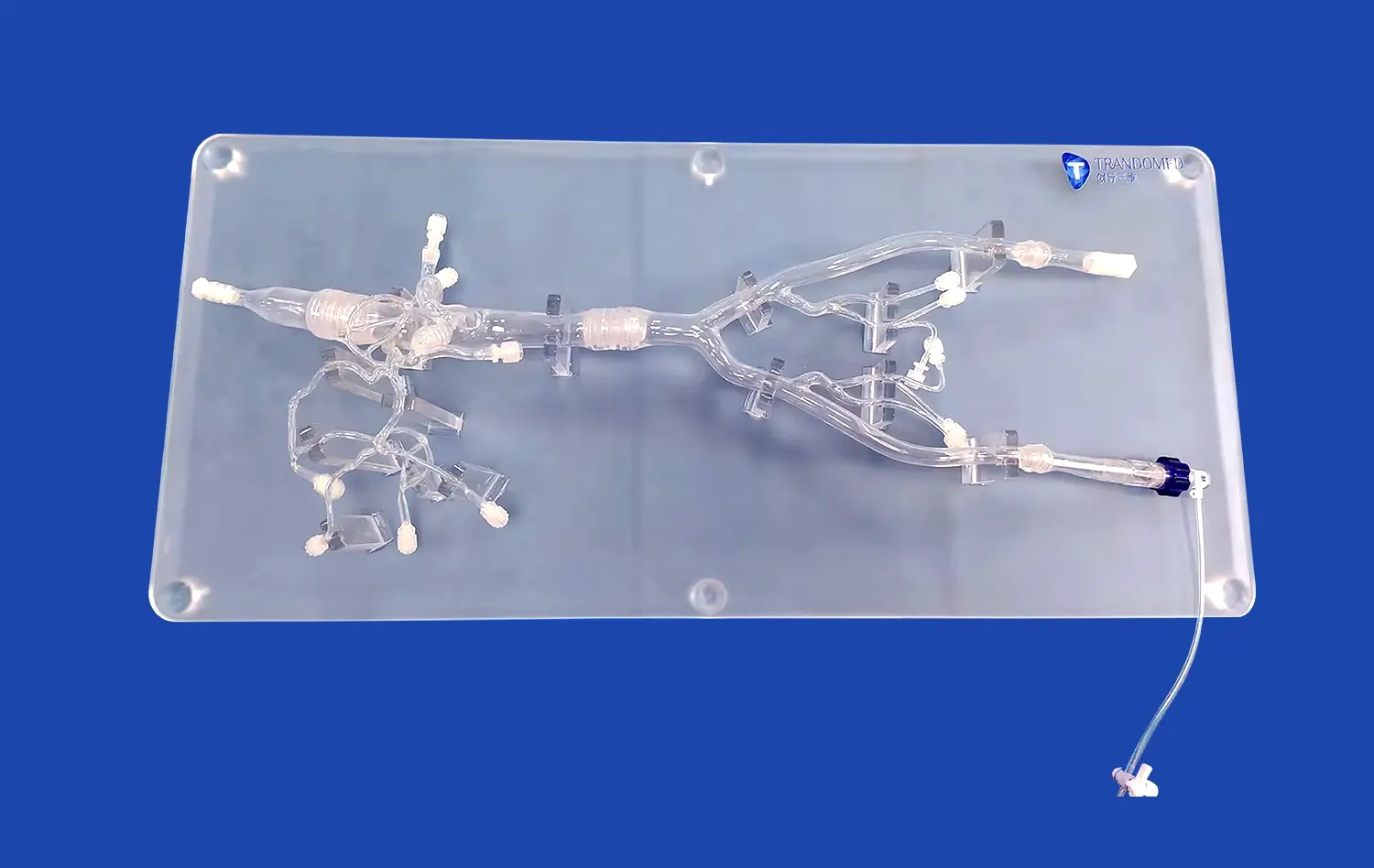
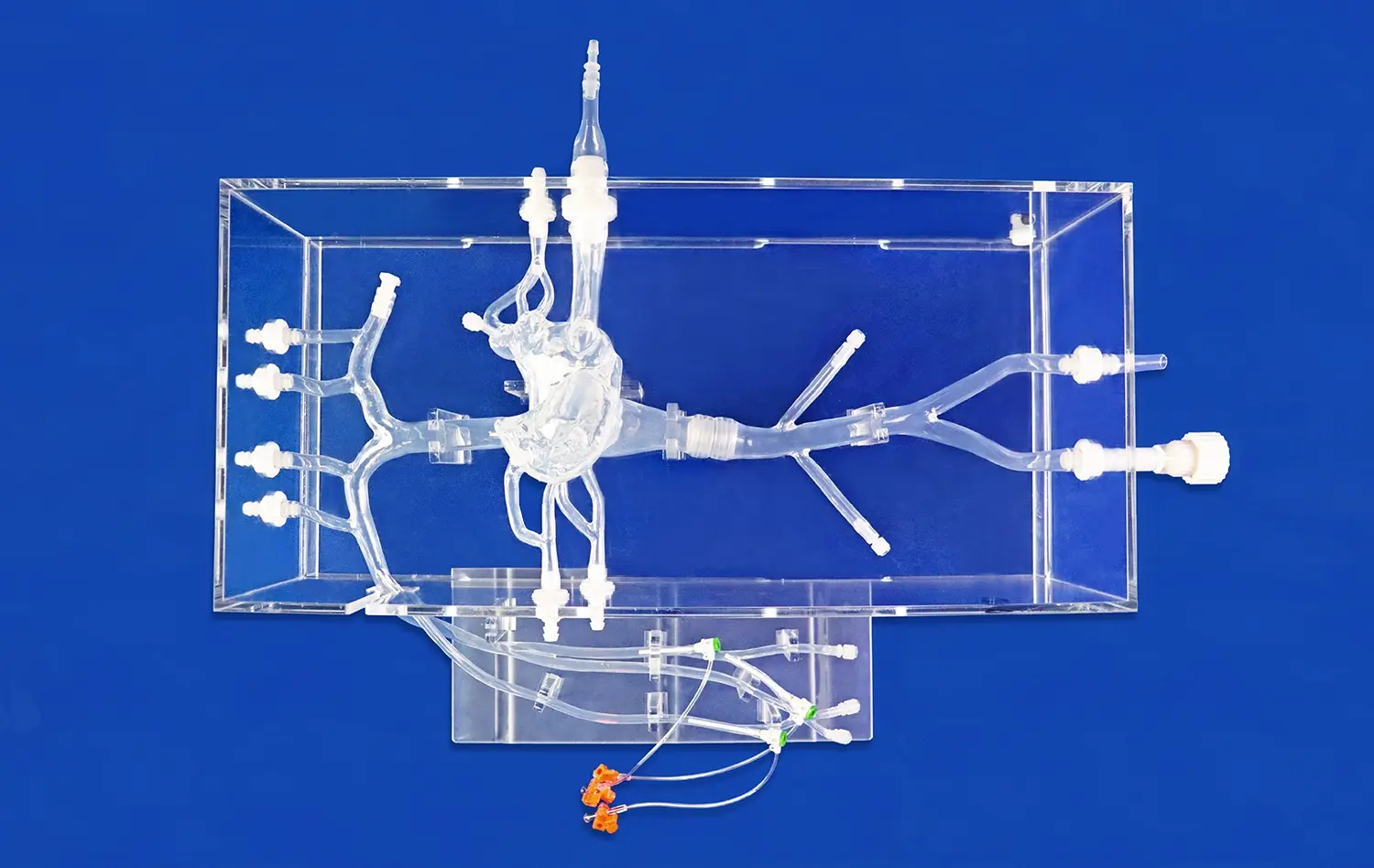
Neurosurgical training demands an intimate understanding of cerebral anatomy. Aneurysm models, such as the SJX011 Intracranial Vascular with Aneurysm Model, offer an unparalleled opportunity for trainees to visualize and interact with accurate representations of the brain's vascular structures. These models meticulously recreate the anterior cerebral artery (ACA), middle cerebral artery (MCA), and the tortuous internal carotid artery, complete with realistic aneurysms. By manipulating these models, neurosurgeons develop a three-dimensional understanding of vascular relationships, crucial for navigating the complex landscape of the brain during actual surgeries.
Procedural Proficiency and Technique Refinement
The journey to becoming a proficient neurosurgeon involves mastering a wide array of techniques. Aneurysm simulators provide a platform for repeated practice of critical procedures such as endovascular coiling and aneurysm clipping. The replaceable aneurysm lesion feature in models like the SJX011 allows for versatile training scenarios, enabling surgeons to hone their skills across various aneurysm morphologies and locations. This repetitive practice in a consequence-free environment is invaluable for developing muscle memory and refining the delicate movements required in neurovascular interventions.
Decision-Making and Problem-Solving Skills
Beyond technical proficiency, neurosurgeons must cultivate sharp decision-making abilities. Aneurysm models facilitate the development of these crucial cognitive skills by presenting trainees with diverse challenges. As they engage with these simulators, neurosurgeons-in-training learn to assess aneurysm characteristics, plan appropriate interventions, and adapt to complications that may arise during procedures. This cognitive training is essential for preparing surgeons to make split-second decisions in high-pressure operating room environments.
What Makes Aneurysm Models Effective for Surgical Simulation?
Anatomical Fidelity and Material Properties
The effectiveness of aneurysm models in surgical simulation hinges on their ability to accurately replicate human anatomy. Advanced manufacturing techniques, such as those employed by Trando 3D Medical Technology Co., Ltd, allow for the creation of models with exceptional anatomical fidelity. These simulators often utilize materials that mimic the properties of human tissue, providing realistic tactile feedback during simulated procedures. The inclusion of features like the tortuous internal carotid artery and multiple aneurysms at varying locations enhances the model's utility for comprehensive training.
Customization and Versatility
One of the key strengths of modern aneurysm models is their customizability. Manufacturers like Trandomed offer the ability to tailor models to specific educational or research objectives. This flexibility allows training programs to create scenarios that target particular learning outcomes or reflect rare and challenging cases. The option to adjust the number, size, and location of aneurysms, as well as the degree of vessel tortuosity, ensures that the models remain relevant across a wide spectrum of training needs.
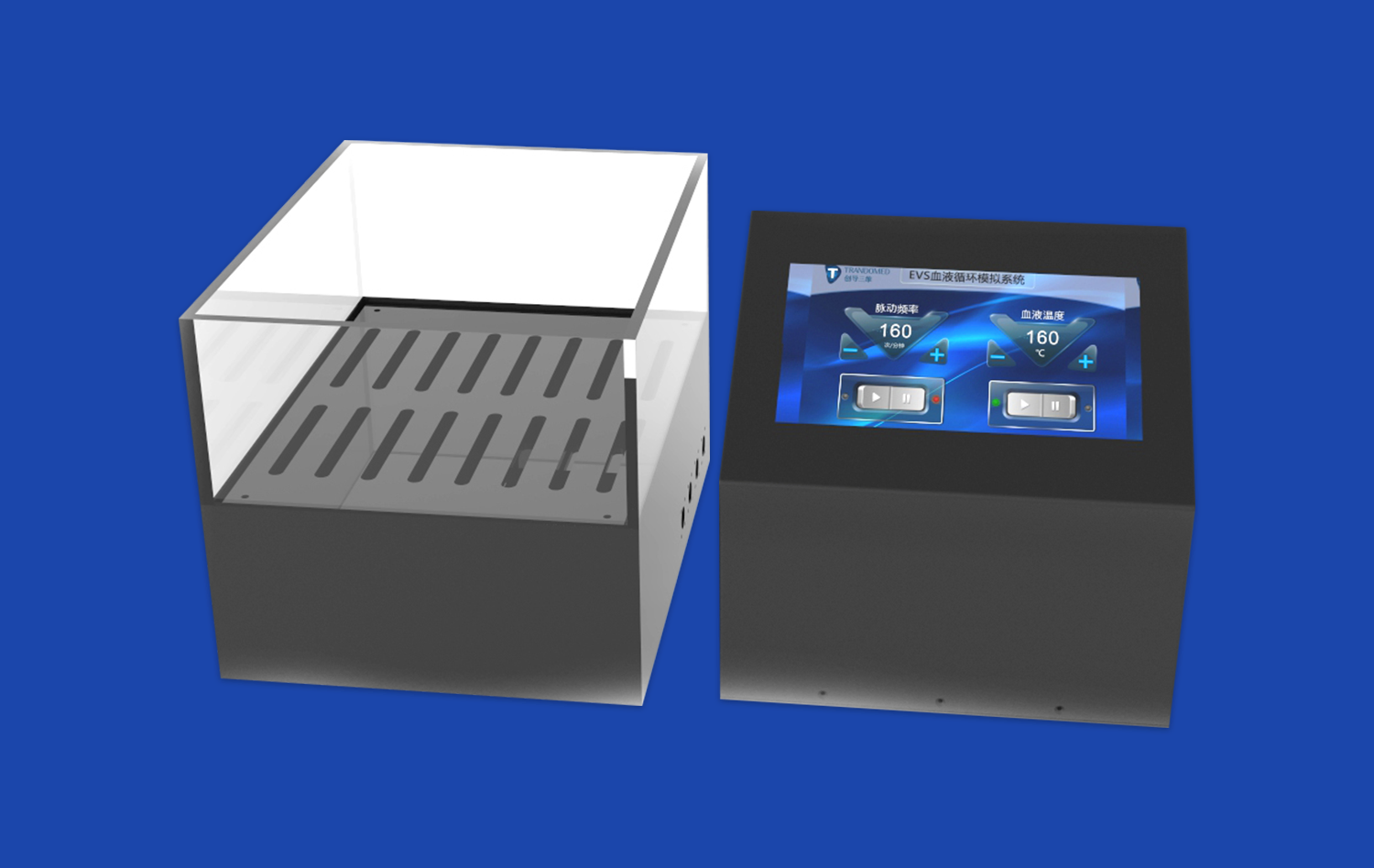
Integration of Advanced Imaging and Technology
State-of-the-art aneurysm models often incorporate advanced imaging capabilities, allowing trainees to practice with the same technological tools used in actual surgeries. Some simulators can be integrated with angiography systems, enabling residents to develop proficiency in interpreting real-time imaging during procedures. This integration of technology into physical models creates a more immersive and comprehensive training experience, bridging the gap between simulation and real-world surgical practice.
Simulation-Based Learning in Neurosurgery Residency Programs
Curriculum Integration and Structured Learning Pathways
Progressive neurosurgery residency programs have begun to systematically incorporate simulation-based learning using aneurysm models into their curricula. These structured learning pathways typically begin with basic anatomical recognition and progress to complex procedural simulations. By integrating aneurysm models throughout the training process, programs ensure that residents build a solid foundation of skills before advancing to more challenging scenarios. This stepwise approach allows for the gradual development of expertise while maintaining a focus on patient safety.
Objective Assessment and Skill Progression Tracking
Aneurysm models provide an objective means of assessing resident performance and tracking skill progression over time. Many simulation platforms include metrics that measure factors such as procedural time, accuracy, and decision-making efficiency. These quantitative assessments offer valuable feedback to both trainees and instructors, allowing for targeted improvement and personalized learning plans. The ability to objectively evaluate competency using aneurysm simulators has become an essential component in ensuring that neurosurgery residents meet the rigorous standards required for independent practice.
Collaborative Learning and Peer Feedback
Simulation-based learning with aneurysm models fosters a collaborative educational environment. Residency programs often utilize these tools in group settings, allowing trainees to observe and learn from their peers. This collaborative approach encourages the exchange of ideas, techniques, and problem-solving strategies among residents. Additionally, the presence of experienced mentors during simulation sessions provides immediate feedback and guidance, accelerating the learning process and helping to instill best practices early in a neurosurgeon's career.
Conclusion
The integration of aneurysm models into neurosurgical training programs has transformed the landscape of medical education in this specialized field. These advanced simulators provide an unparalleled platform for skill development, offering a safe environment for trainees to hone their craft before entering the operating room. As technology continues to evolve, the role of aneurysm models in shaping competent, confident neurosurgeons will only grow in importance. By embracing these innovative training tools, the neurosurgical community ensures a future where patient care is continually enhanced through well-prepared and highly skilled practitioners.
Contact Us
For more information on cutting-edge aneurysm models and how they can elevate your neurosurgical training program, contact Trandomed. Our team of experts is dedicated to providing customized solutions that meet the unique needs of your institution. Explore the possibilities of advanced medical simulation and take your training to the next level. Reach out to us at jackson.chen@trandomed.com to discuss how our state-of-the-art aneurysm models can transform your educational experience.
References
Alaraj, A., et al. (2015). Role of aneurysm models in neurosurgical training. Neurosurgery, 76(6), 762-768.
Chugh, A. J., et al. (2017). The impact of simulation-based neurosurgical training on resident performance. Journal of Neurosurgery, 126(1), 252-258.
Kirkman, M. A., et al. (2014). The use of simulation in neurosurgical education and training. Journal of Neurosurgery, 121(2), 228-246.
Lobel, D. A., et al. (2013). Value of repeat angiography in patients with aneurysmal subarachnoid hemorrhage after initial endovascular treatment. Journal of Neurosurgery, 118(1), 34-39.
Winkler-Schwartz, A., et al. (2016). Simulation in neurosurgery: a review of computer-based simulation environments and their surgical applications. Neurosurgery, 79(4), 505-516.
Zada, G., et al. (2013). Cerebrovascular bypass surgery: a critical review of the literature. Neurosurgical Focus, 34(2), E12.

_1736216292718.webp)