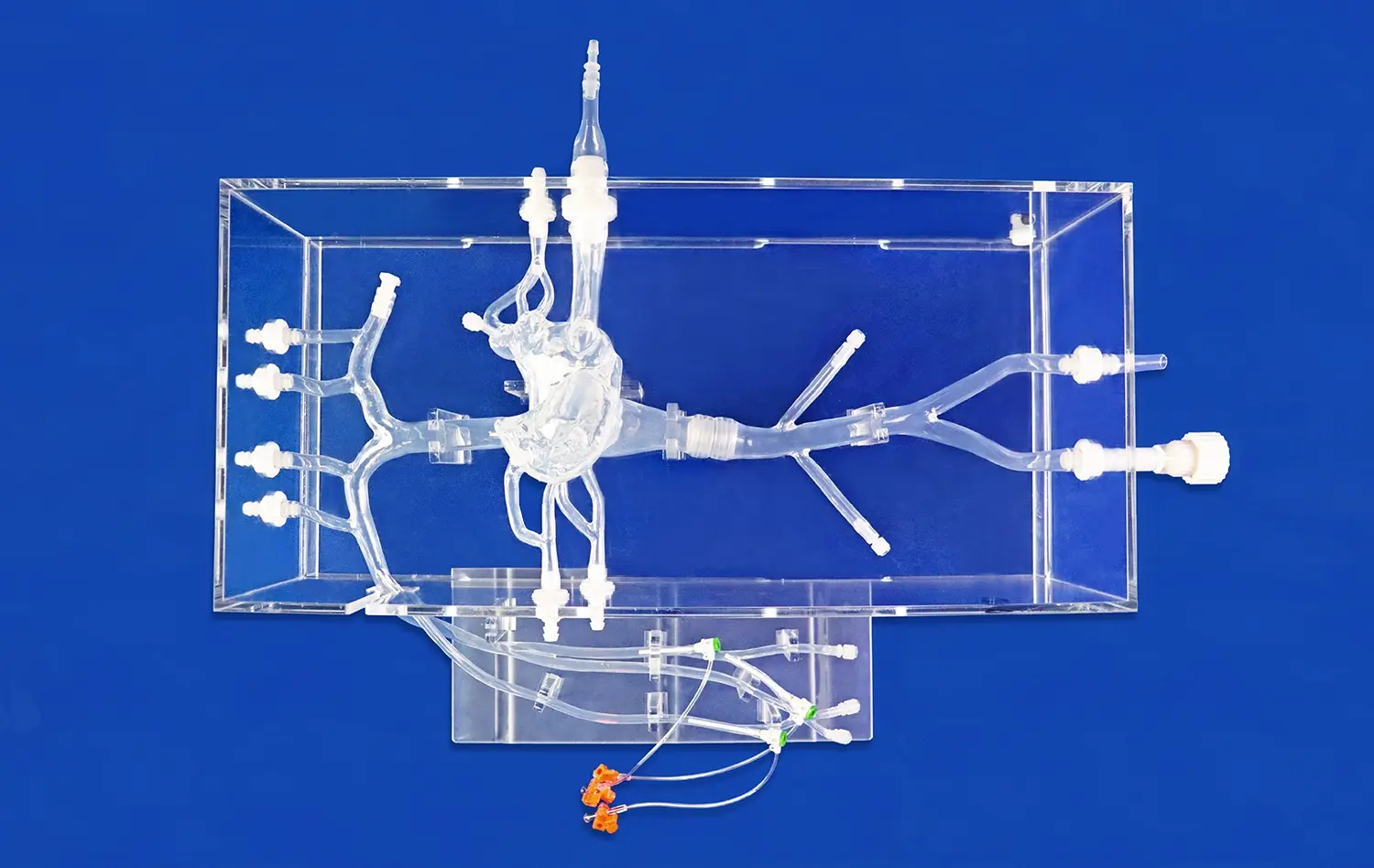
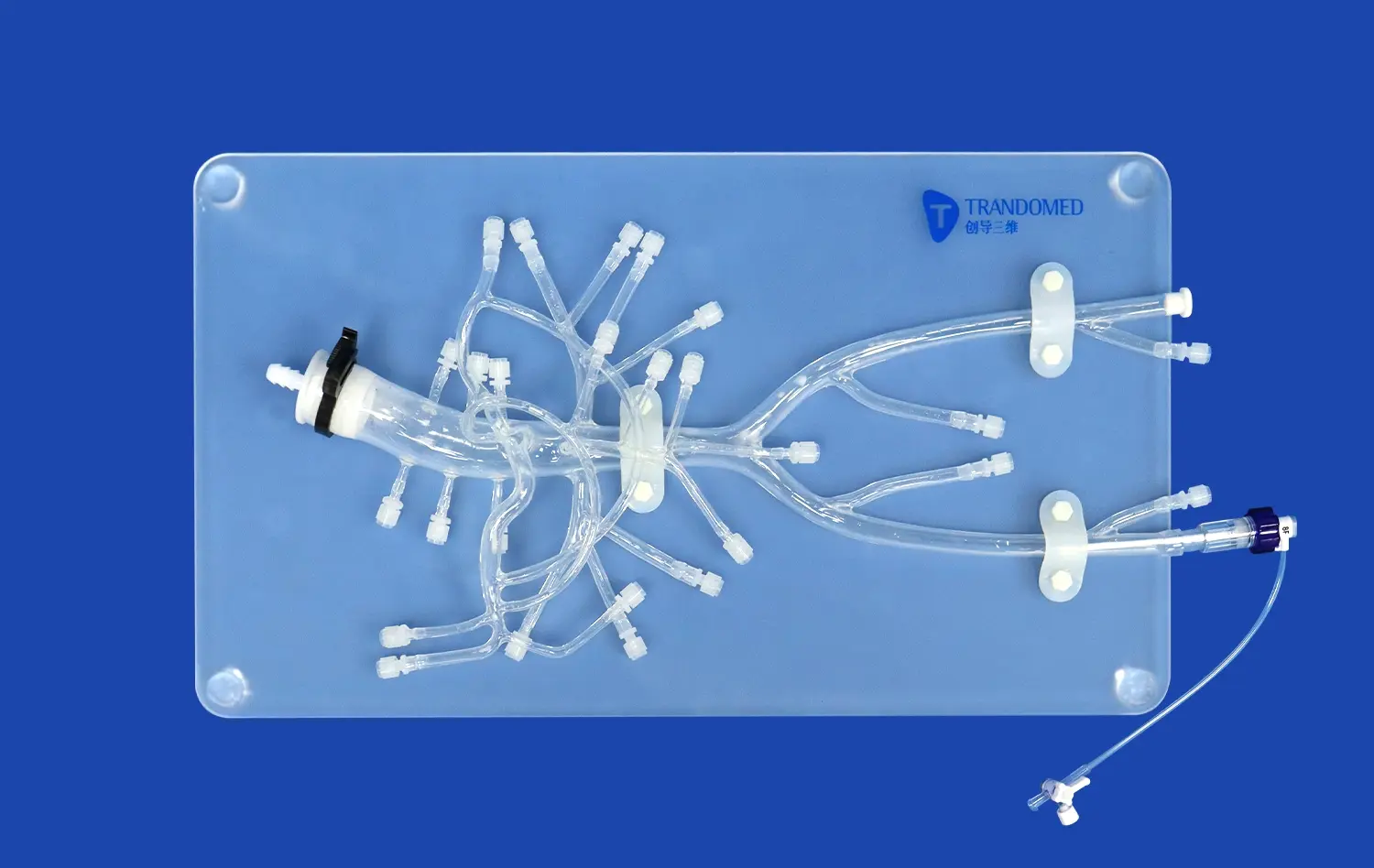
Medical students greatly benefit from hands-on experience with aneurysm models, as these intricate replicas of cerebral vasculature provide an unparalleled opportunity for practical learning. These models, such as the Intracranial Vascular with Aneurysm Model (SJX011), offer a tangible representation of complex neurovascular structures, allowing students to visualize and interact with anatomical features that are otherwise challenging to comprehend from textbooks alone. By manipulating these models, future physicians can develop a deeper understanding of aneurysm morphology, spatial relationships within the brain, and the intricacies of various treatment approaches. This hands-on experience not only enhances their anatomical knowledge but also builds confidence in handling delicate neurovascular structures, ultimately preparing them for real-world clinical scenarios and improving patient outcomes in their future practice.
What Do Students Learn from Physical Neurovascular Models?
Anatomical Precision and Spatial Awareness
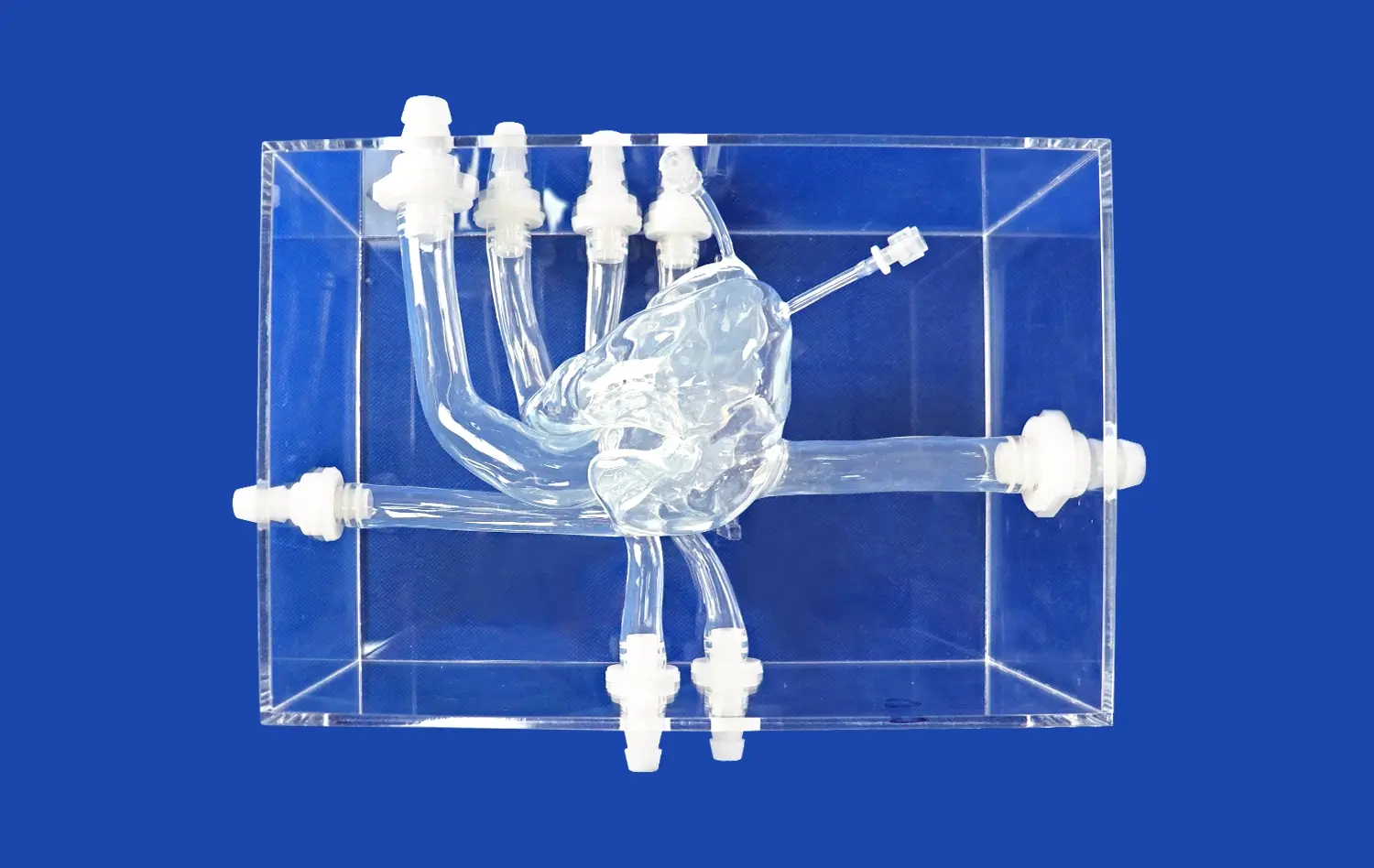
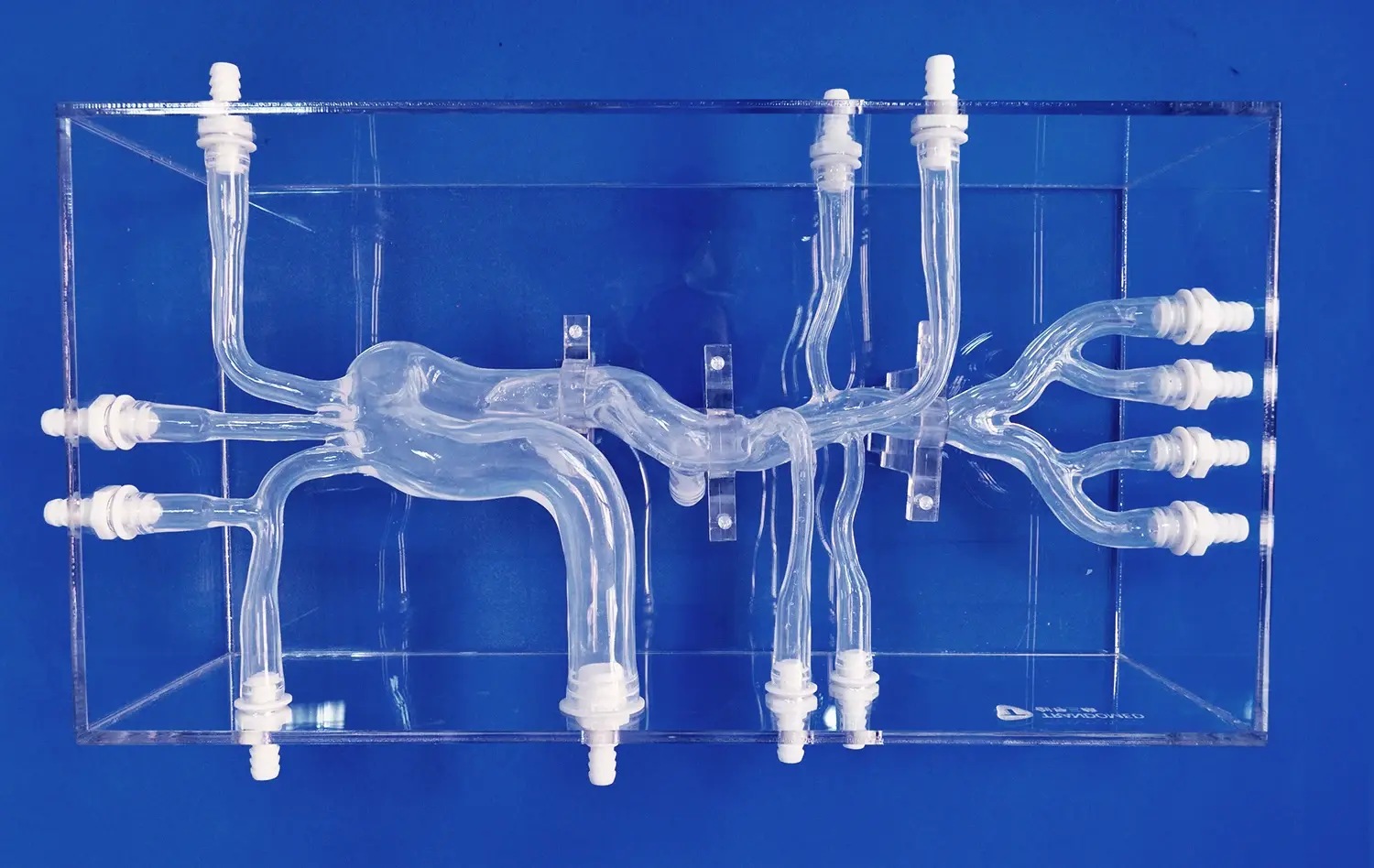
Physical neurovascular models provide medical students with an unprecedented level of anatomical precision. The intricate details of cerebral vasculature, including the anterior cerebral artery (ACA), middle cerebral artery (MCA), and the tortuous internal carotid artery, are faithfully reproduced in these models. This accuracy allows students to develop a keen sense of spatial awareness, understanding how these vessels interrelate within the confined space of the cranium. By manipulating the model, students can appreciate the three-dimensional relationships between different vascular structures, a crucial skill for future neurosurgeons and interventional radiologists.
Aneurysm Morphology and Classification
Hands-on aneurysm models offer students the opportunity to examine various types of aneurysms up close. They can observe the distinct shapes, sizes, and locations of different aneurysms, learning to differentiate between saccular, fusiform, and other less common types. This tactile experience reinforces their understanding of aneurysm classification systems and helps them recognize the subtle nuances that can impact treatment decisions. The ability to visualize and feel these differences is invaluable in developing the clinical judgment necessary for accurate diagnosis and treatment planning.
Vascular Abnormalities and Variations
Beyond typical aneurysm presentations, physical models can incorporate various vascular abnormalities and anatomical variations. This exposure is crucial for medical students, as it prepares them for the diverse range of cases they may encounter in clinical practice. By studying models that showcase different vascular patterns, students learn to identify potential risk factors for aneurysm formation and understand how anatomical variations might complicate treatment approaches. This comprehensive understanding of vascular diversity enhances their diagnostic skills and ability to tailor treatment strategies to individual patient anatomies.
Enhancing Anatomical Understanding Through Interactive Training
Tactile Learning and Muscle Memory
Interactive training with aneurysm models engages multiple senses, reinforcing learning through tactile experiences. As students handle these models, they develop muscle memory for navigating complex vascular structures. This kinesthetic learning approach is particularly beneficial for aspiring neurosurgeons and interventional specialists who will need to perform delicate procedures with precision. The repeated manipulation of realistic models helps students internalize the feel of different vascular textures and resistances, preparing them for future clinical interventions.
Visualization of Blood Flow Dynamics
Advanced aneurysm models can incorporate features that simulate blood flow dynamics. This allows students to visualize how blood circulates through healthy vessels and how flow patterns change in the presence of aneurysms. Understanding these hemodynamic principles is crucial for comprehending aneurysm formation, growth, and rupture risk. By observing simulated flow patterns, students can better grasp the importance of factors like wall shear stress and turbulence in aneurysm pathophysiology, enhancing their ability to predict high-risk scenarios and plan appropriate interventions.
Comparative Analysis of Treatment Options
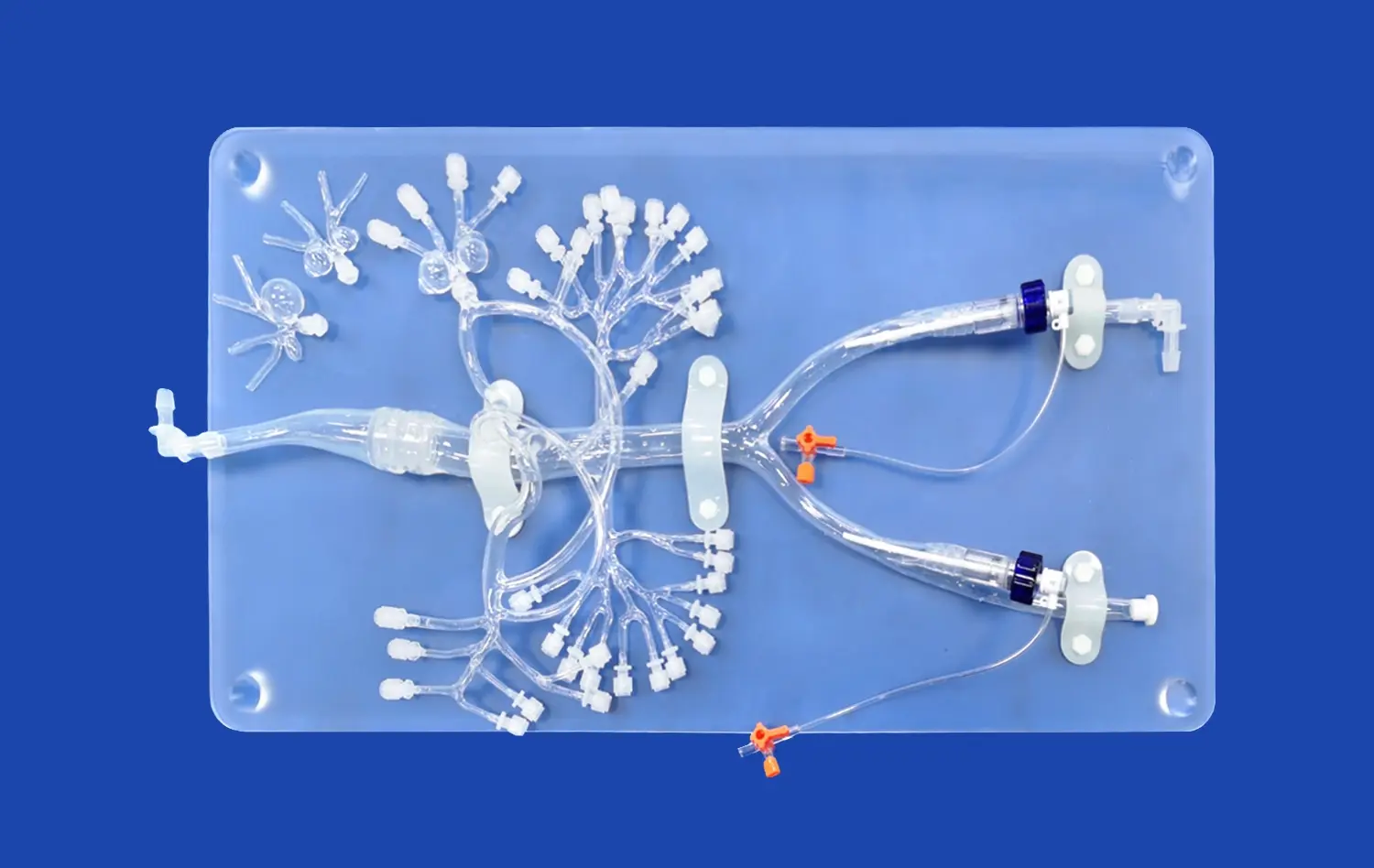
Interactive aneurysm models provide an excellent platform for students to compare different treatment modalities. With models that allow for simulated endovascular coiling, clipping, and flow diversion techniques, students can evaluate the advantages and challenges associated with each approach. This hands-on comparison fosters critical thinking skills, enabling students to consider factors such as aneurysm location, size, and patient-specific characteristics when selecting the most appropriate treatment strategy. By practicing these techniques on models, students develop a nuanced understanding of when to apply each intervention in clinical scenarios.
Early Exposure to Surgical Scenarios in Academic Settings
Risk-Free Procedural Practice
Aneurysm models create a safe environment for medical students to practice surgical and endovascular procedures without the pressure of real-world consequences. This risk-free setting allows them to make mistakes, learn from errors, and refine their techniques without compromising patient safety. Students can repeatedly practice complex procedures like aneurysm clipping or coil deployment, gradually building confidence and competence. This early exposure to procedural nuances accelerates the learning curve, potentially reducing the time required for students to achieve proficiency in clinical settings.
Simulation of Complications and Emergency Scenarios
Advanced aneurysm models can be designed to simulate various complications and emergency scenarios that may arise during neurovascular procedures. These might include aneurysm rupture during intervention, vessel perforation, or thromboembolic events. By encountering these simulated emergencies in a controlled academic environment, students learn to recognize critical situations quickly and develop problem-solving skills under pressure. This preparation is invaluable for building the mental resilience and quick decision-making abilities required in high-stakes neurosurgical interventions.
Interdisciplinary Collaboration and Communication
Working with aneurysm models in academic settings often involves collaborative exercises that mirror real-world multidisciplinary teams. Students from various specialties, including neurosurgery, interventional radiology, and anesthesiology, can practice together, simulating the teamwork required in complex neurovascular cases. These collaborative sessions improve communication skills, enhance understanding of each specialty's role, and foster a culture of mutual respect among future healthcare professionals. The ability to effectively communicate and cooperate in high-pressure situations is a crucial skill that students can develop through these interactive model-based training sessions.
Conclusion
Hands-on aneurysm models offer medical students an invaluable opportunity to bridge the gap between theoretical knowledge and practical application in neurovascular medicine. These interactive tools enhance anatomical understanding, provide risk-free procedural practice, and foster critical thinking skills essential for future clinicians. By integrating such models into medical education, institutions can better prepare students for the complexities of neurovascular interventions, ultimately leading to improved patient care and outcomes in the field of neurosurgery and interventional neuroradiology.
Contact Us
Elevate your medical training program with Trandomed's cutting-edge aneurysm models. Our state-of-the-art simulations provide unparalleled realism and versatility for comprehensive neurovascular education. Experience the benefits of hands-on learning and prepare your students for success in neurosurgical and interventional procedures. For more information on our customizable aneurysm models and other medical simulation products, contact us at jackson.chen@trandomed.com. Invest in the future of medical education with Trandomed – where innovation meets excellence in healthcare training.
References
Bambakidis, N. C., et al. (2018). "Simulation in Neurosurgery: A Review of Computer-Based Simulation Environments and Their Surgical Applications." Neurosurgery, 83(5), 1039-1055.
Chugh, A. J., et al. (2019). "The Use of 3D-Printed Models in Resident Education for the Classification of Acetabular Fractures." Journal of Surgical Education, 76(5), 1316-1324.
Ghobrial, G. M., et al. (2020). "Simulation in Neurosurgery: A Review of Current Status and Future Perspectives." Neurosurgical Focus, 48(3), E2.
Lobel, D. A., et al. (2017). "Value of Repetitive Training of Neurosurgical Residents in a Cadaveric Lab Using 3D-Printed Models." Journal of Neurosurgery, 127(6), 1465-1471.
Waran, V., et al. (2014). "Utility of Multimaterial 3D Printers in Creating Models with Pathological Entities to Enhance the Training Experience of Neurosurgeons." Journal of Neurosurgery, 120(2), 489-492.
Zhu, W., et al. (2016). "Application of a Three-Dimensional Printed Vessel with Aneurysm Model for Surgical Training." Journal of Clinical Neuroscience, 32, 147-152.