What Are the Key Challenges in Cerebral Aneurysm Tamponade?
Navigating Complex Vascular Anatomy
One of the primary challenges in cerebral aneurysm tamponade procedures is navigating the intricate network of blood vessels in the brain. The cerebral vasculature is characterized by its tortuous paths, varying vessel diameters, and delicate branching patterns. Neurovascular interventionists must possess exceptional spatial awareness and fine motor skills to maneuver catheters and guidewires through this complex anatomy without causing vessel damage or perforation.
Precise Aneurysm Occlusion
Achieving complete aneurysm occlusion while preserving blood flow to vital brain regions is a delicate balancing act. Interventionists must carefully deploy embolic coils or flow diverters to fill the aneurysm sac or redirect blood flow, respectively. The challenge lies in ensuring optimal packing density to prevent recanalization while avoiding coil herniation into the parent vessel. This requires a nuanced understanding of aneurysm morphology and hemodynamics, as well as proficiency in device selection and deployment techniques using a neuro vascular simulator
Managing Procedural Complications
Cerebral aneurysm tamponade procedures carry inherent risks, including thromboembolic events, vessel dissection, or aneurysm rupture. Recognizing and swiftly addressing these complications is crucial for patient safety. Interventionists must be prepared to manage a wide range of scenarios, from deploying rescue stents to performing emergent coiling in case of intra-procedural rupture. The ability to remain calm under pressure and make rapid, informed decisions is essential in mitigating adverse outcomes.
Precision Catheter Navigation in Aneurysm Models
Realistic Vascular Replicas
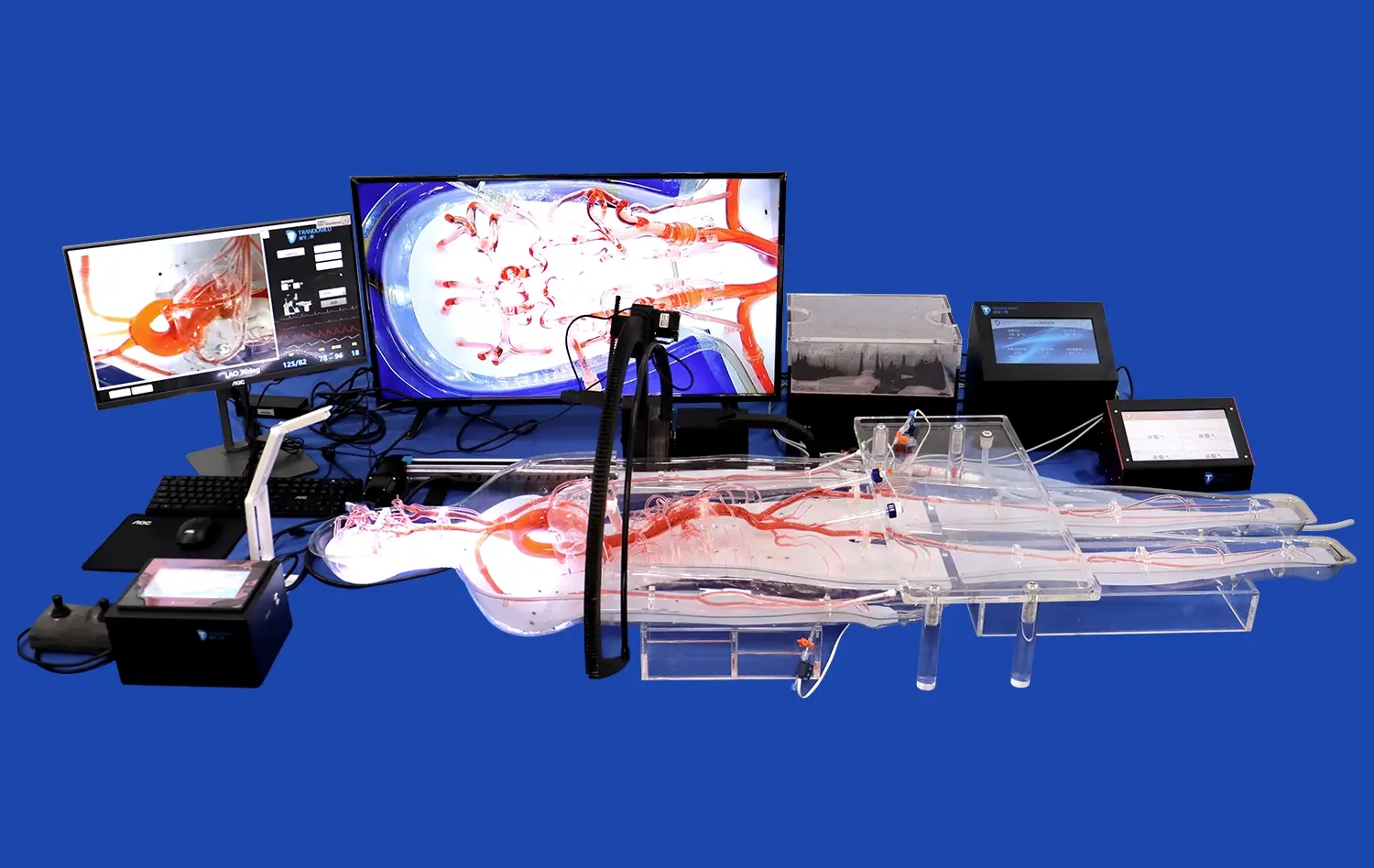
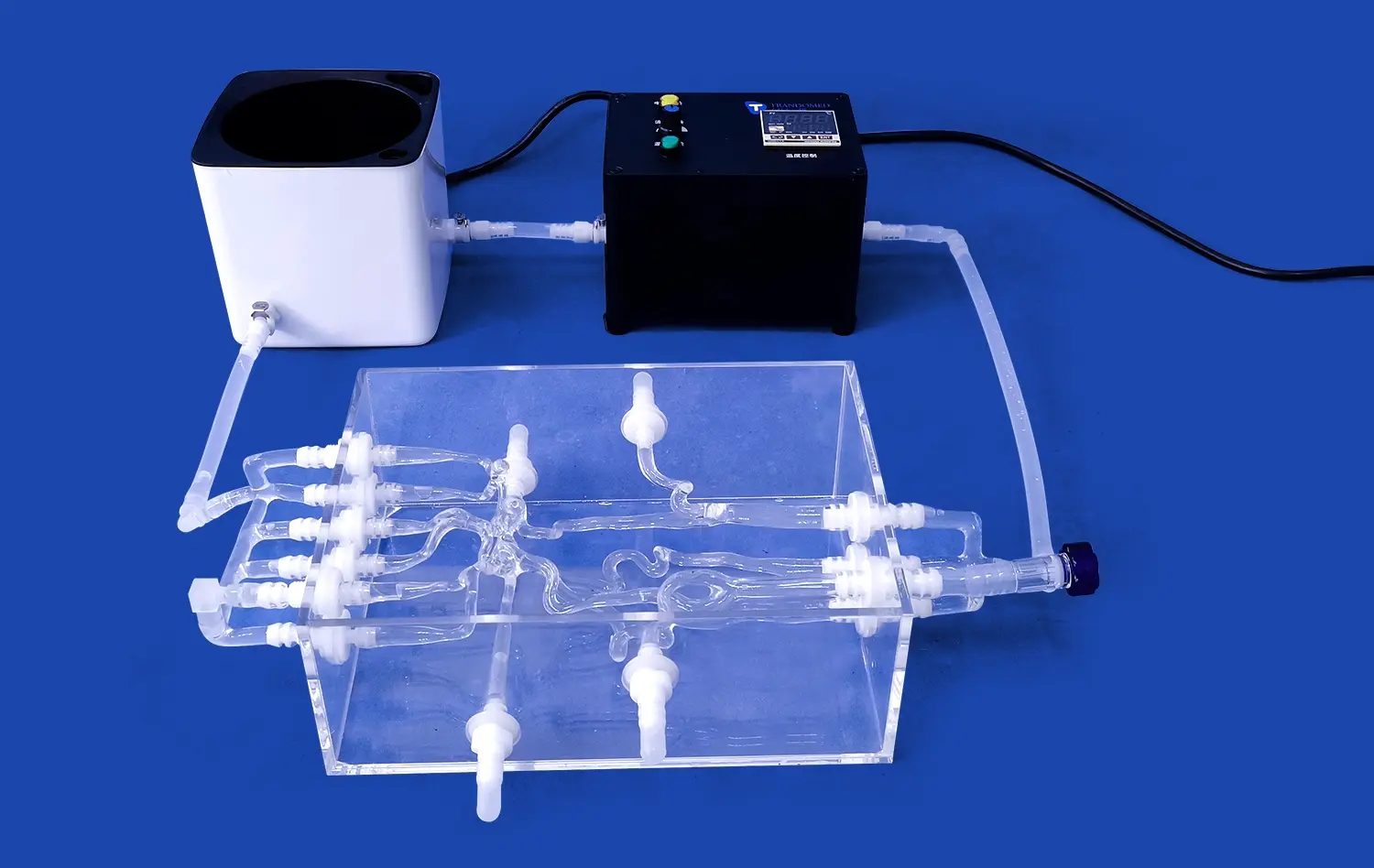
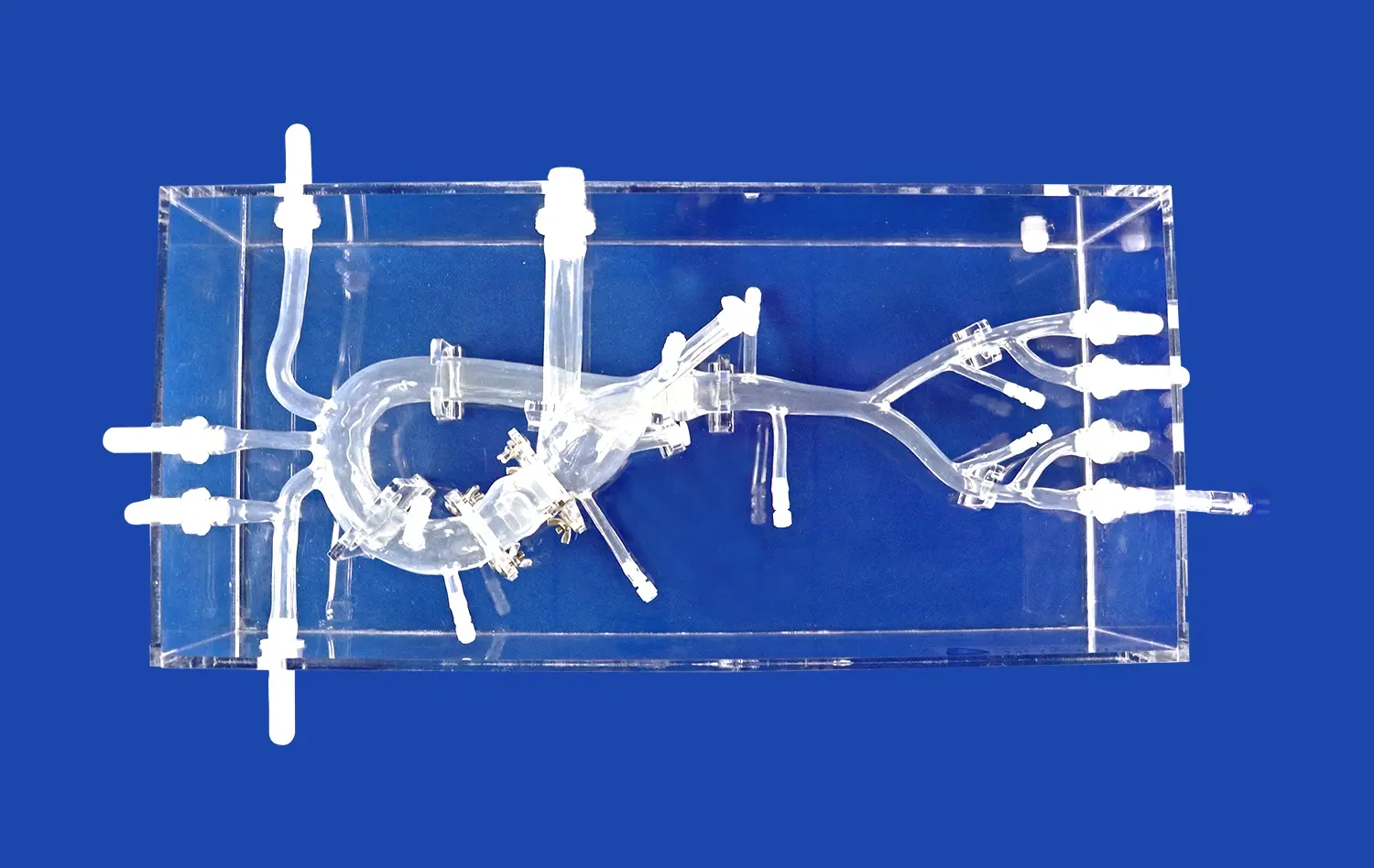
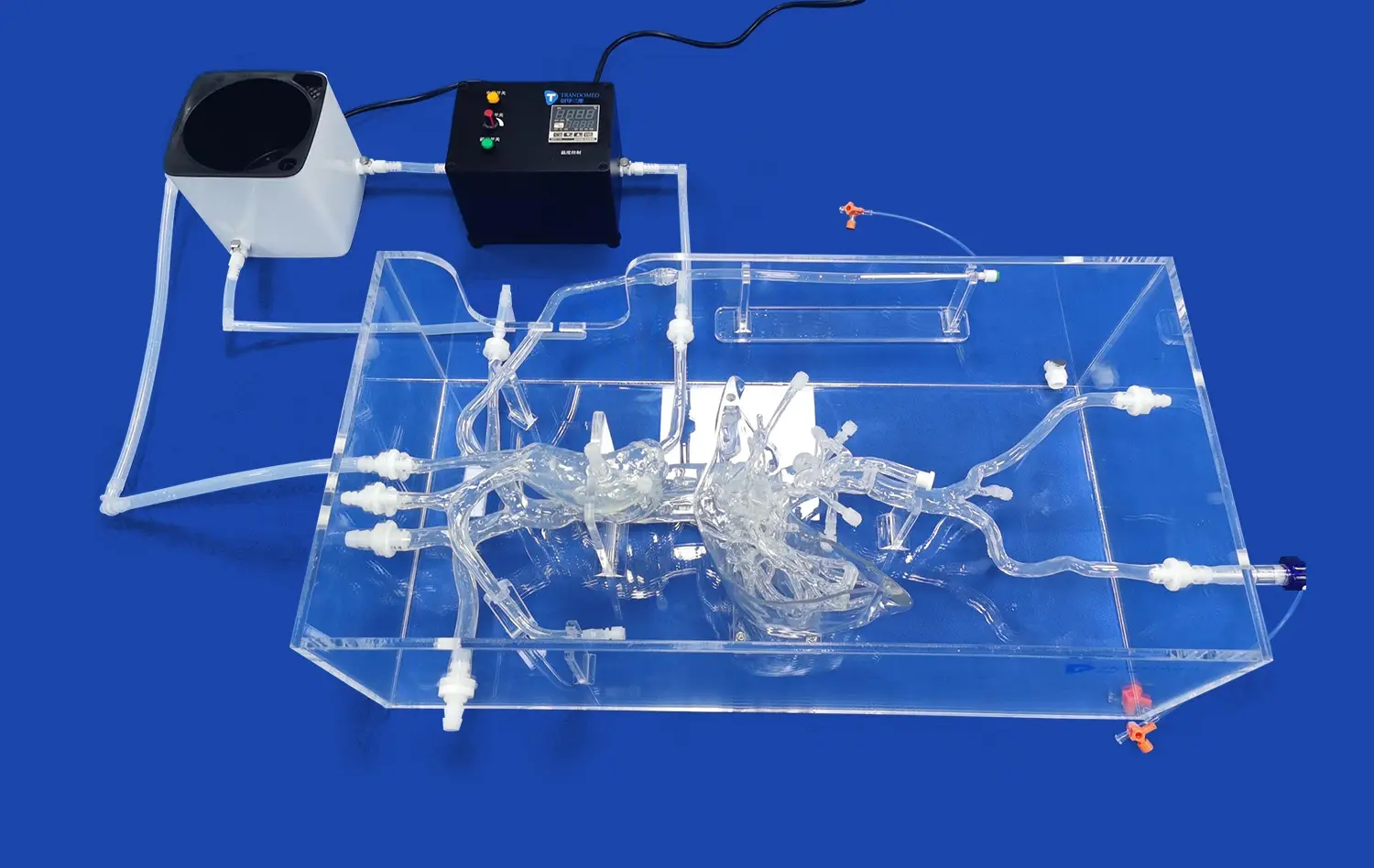
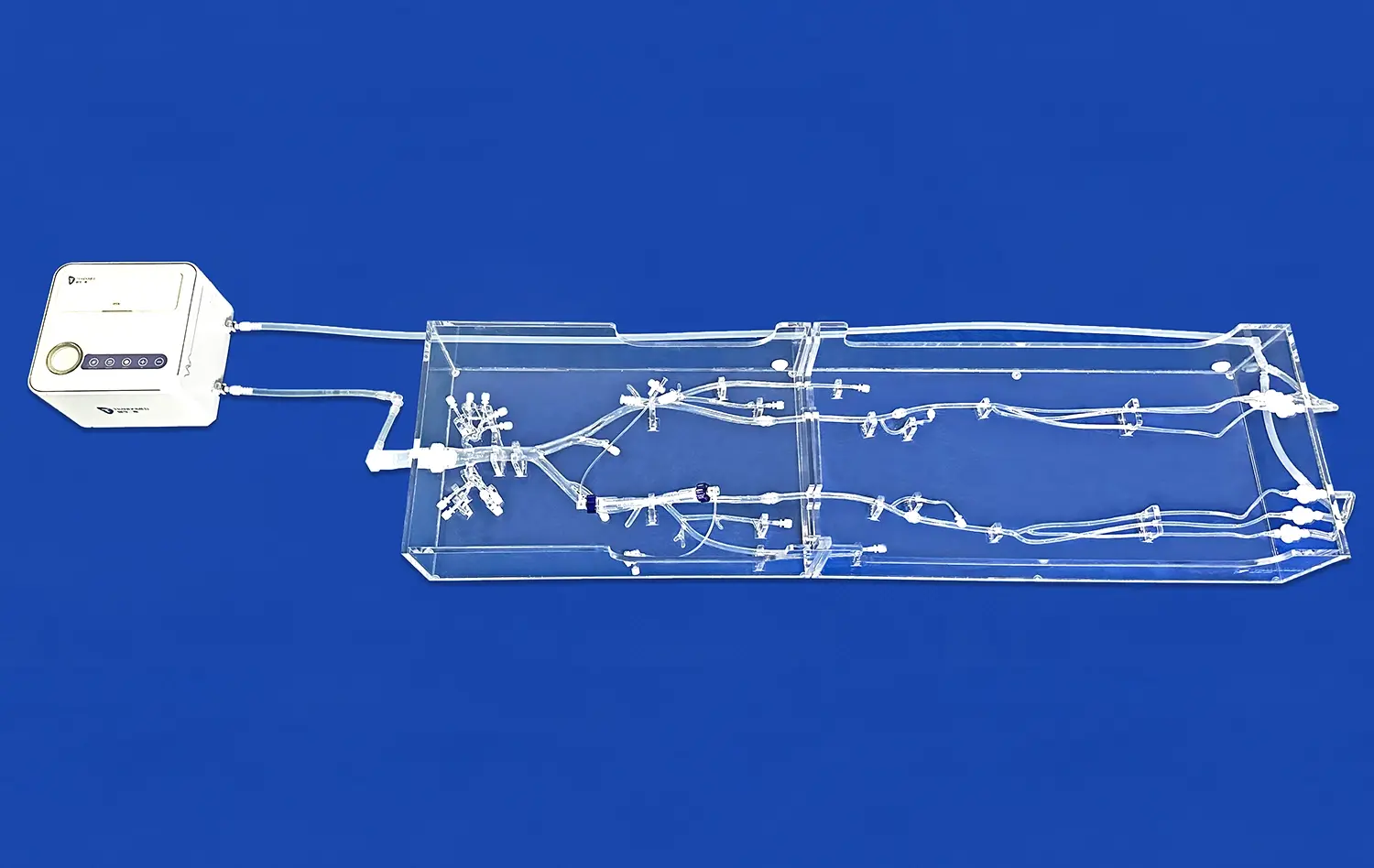
Advanced neuro vascular simulators, such as those developed by Trandomed, offer highly accurate replicas of the cerebral vasculature. These models are based on extensive real human CT and MRI data, utilizing reverse 3D reconstruction technology to create anatomically correct representations. The use of customized transparent connectors allows for interchangeable neuro, cardiac thoracic, and abdominal sections, providing a comprehensive training platform that closely mimics the clinical environment.
Haptic Feedback and Force Sensation
State-of-the-art neuro vascular simulators incorporate haptic feedback mechanisms that replicate the tactile sensations experienced during actual procedures. This feature allows trainees to develop a feel for the subtle resistance and friction encountered when navigating catheters through vessels of varying diameters and tortuosity. The ability to sense these forces is crucial for avoiding vessel trauma and perfecting the delicate movements required for successful aneurysm tamponade.
Fluoroscopic Guidance Simulation
Neuro vascular simulators integrate simulated fluoroscopic imaging, enabling trainees to practice catheter navigation under x-ray guidance without exposure to radiation. These systems often include features such as road-mapping and digital subtraction angiography, mirroring the imaging modalities used in clinical practice. By honing their skills in interpreting 2D fluoroscopic images to navigate 3D anatomical structures, interventionists can improve their spatial reasoning and reduce procedure times in real-world scenarios.
Measuring and Improving Tamponade Success Rates Through Simulation
Quantitative Performance Metrics
Neuro vascular simulators equipped with advanced software can track and analyze a wide range of performance metrics. These may include procedure time, fluoroscopy time, contrast volume used, number of catheter exchanges, and accuracy of device placement. By objectively measuring these parameters, trainees and experienced practitioners alike can identify areas for improvement and track their progress over time. This data-driven approach to skill assessment allows for targeted training interventions and helps establish benchmarks for procedural competence.
Scenario-Based Learning
Modern neuro vascular simulator platforms offer a diverse array of clinical scenarios, ranging from straightforward saccular aneurysms to complex wide-necked or fusiform configurations. Trainees can practice tamponade techniques on various aneurysm models, each presenting unique challenges in terms of access, device selection, and deployment strategy. This exposure to a wide range of cases builds adaptability and decision-making skills, preparing interventionists for the variability encountered in clinical practice.
Iterative Practice and Feedback
The ability to repeatedly practice procedures without risk to patient safety is a significant advantage of neuro vascular simulation. Trainees can attempt multiple approaches to aneurysm tamponade, learning from both successes and failures in a controlled environment. Many simulators provide immediate feedback on procedural outcomes, such as the degree of aneurysm occlusion achieved or the presence of complications like coil prolapse. This rapid feedback loop accelerates the learning process, allowing for continuous refinement of technique and decision-making skills.
Conclusion
Neuro vascular simulators have emerged as indispensable tools in improving cerebral aneurysm tamponade skills. By providing a realistic, risk-free environment for practice, these advanced training platforms address key challenges in procedural competence. From navigating complex vascular anatomy to achieving precise aneurysm occlusion, simulators offer a comprehensive solution for skill development. The integration of quantitative performance metrics and scenario-based learning further enhances the educational value, leading to improved tamponade success rates and, ultimately, better patient outcomes in clinical practice.
Contact Us
Elevate your neurovascular training program with Trandomed's cutting-edge 3D printed silicone medical simulators. Our state-of-the-art neuro vascular simulators offer unparalleled realism and versatility, helping healthcare professionals refine their skills in a risk-free environment. Experience the future of medical education and improve patient outcomes. For more information on our innovative simulation solutions, contact us at jackson.chen@trandomed.com.
References
1. Spiotta, A. M., Rasmussen, P. A., Masaryk, T. J., Benzel, E. C., & Schlenk, R. (2013). Simulated diagnostic cerebral angiography in neurosurgical training: a pilot program. Journal of Neurointerventional Surgery, 5(4), 376-381.
2. Fargen, K. M., Arthur, A. S., Bendok, B. R., Levy, E. I., Ringer, A., Siddiqui, A. H., ... & Mocco, J. (2013). Experience with a simulator-based angiography course for neurosurgical residency training: beyond the pilot program. Neurosurgery, 73(suppl_1), S46-S50.
3. Yaeger, K. A., Mascitelli, J. R., Kellner, C. P., Oermann, E. K., De Leacy, R. A., Mocco, J., & Fifi, J. T. (2019). Simulation training for neurosurgical residents targeting endovascular management of acute ischemic stroke. World Neurosurgery, 127, e468-e473.
4. Benet, A., Plata-Bello, J., Abla, A. A., Acevedo-Bolton, G., Saloner, D., & Lawton, M. T. (2015). Implantation of 3D-printed patient-specific aneurysm models into cadaveric specimens: a new training paradigm to allow for improvements in cerebrovascular surgery and research. BioMed Research International, 2015.
5. Wiebers, D. O., Whisnant, J. P., Huston III, J., Meissner, I., Brown Jr, R. D., Piepgras, D. G., ... & International Study of Unruptured Intracranial Aneurysms Investigators. (2003). Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. The Lancet, 362(9378), 103-110.
6. Molyneux, A. J., Kerr, R. S., Yu, L. M., Clarke, M., Sneade, M., Yarnold, J. A., & Sandercock, P. (2005). International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. The Lancet, 366(9488), 809-817.