How PCI Training Models Help Simulate Complex Coronary Lesions?
2025-08-07 09:00:01
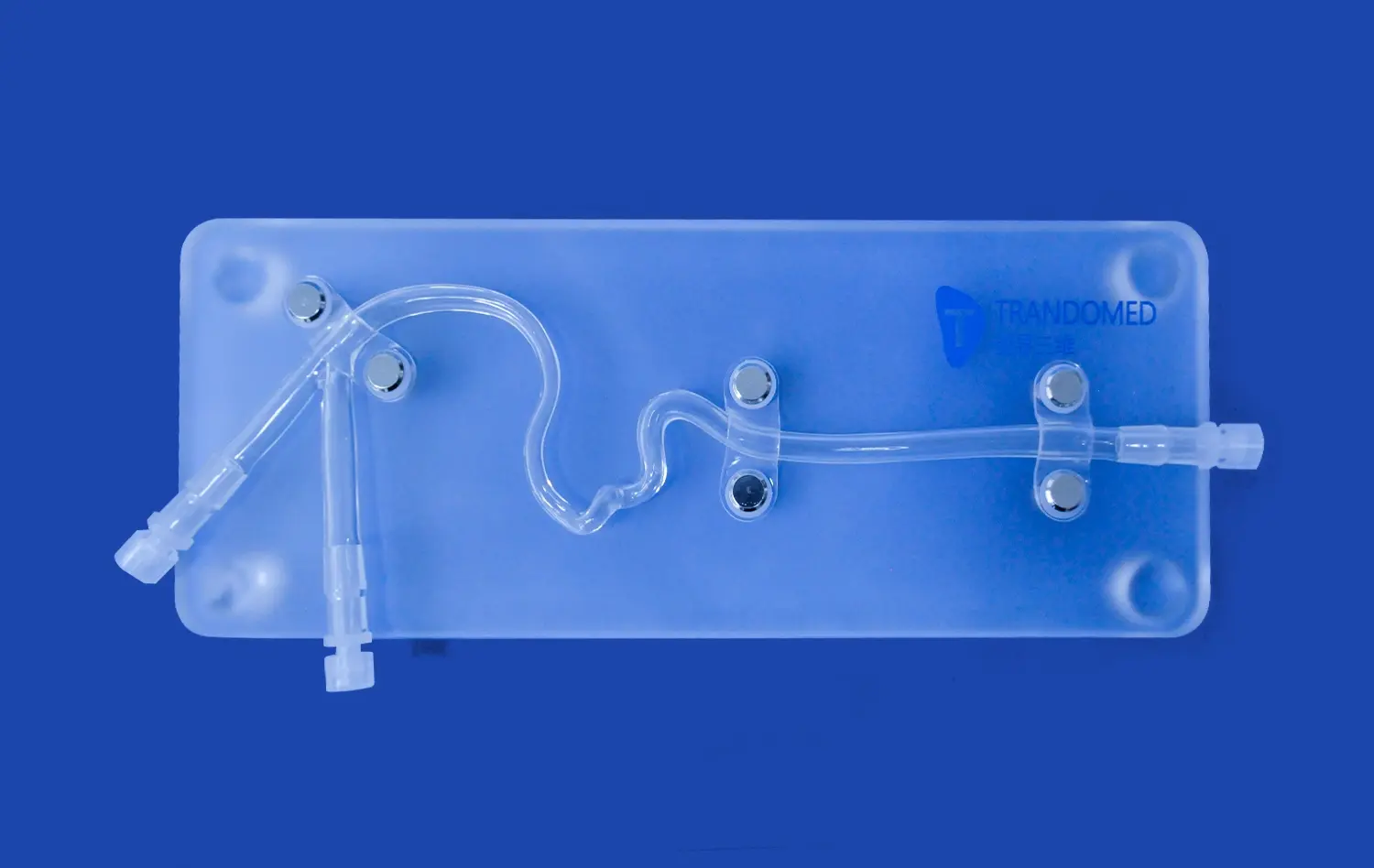
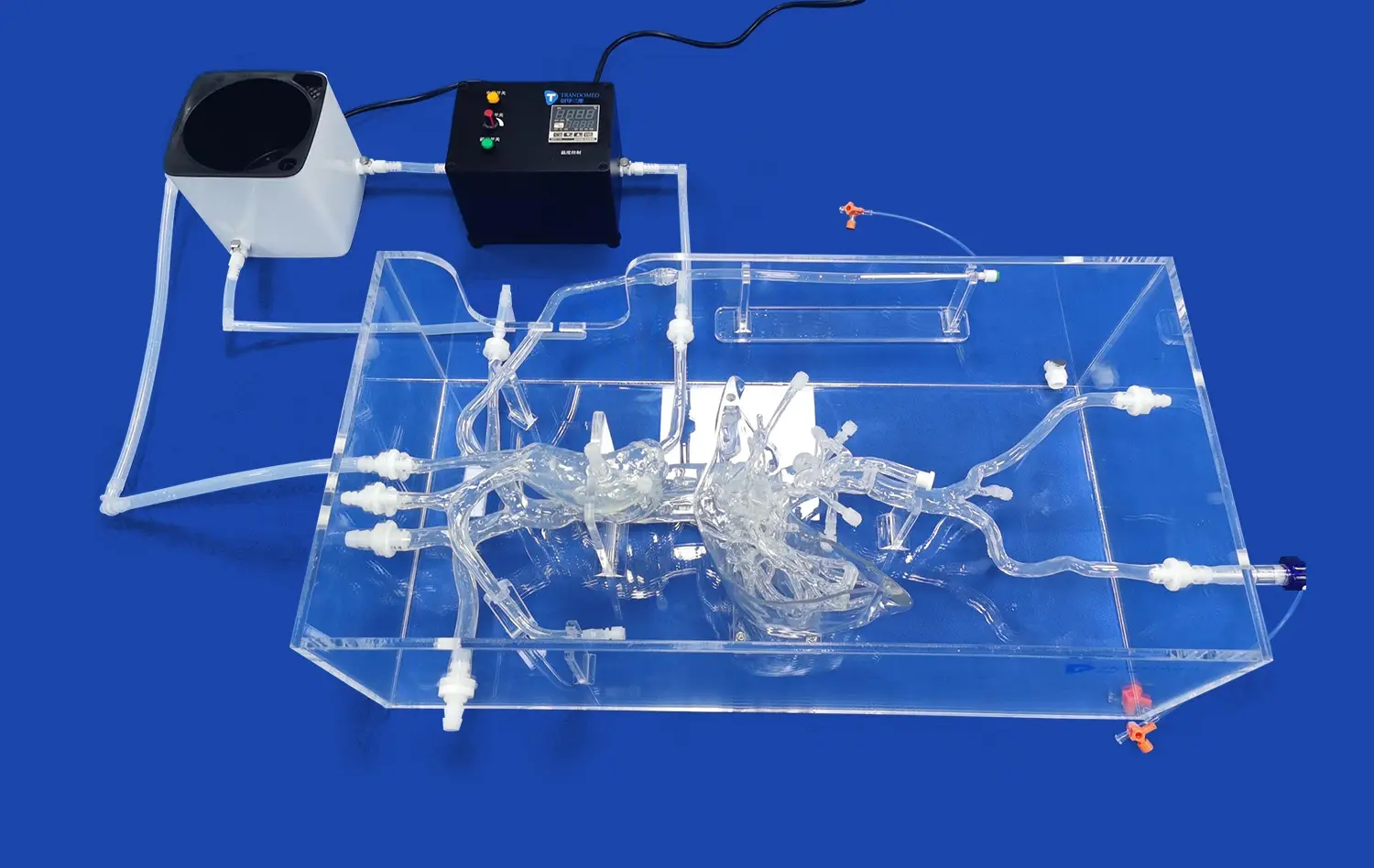
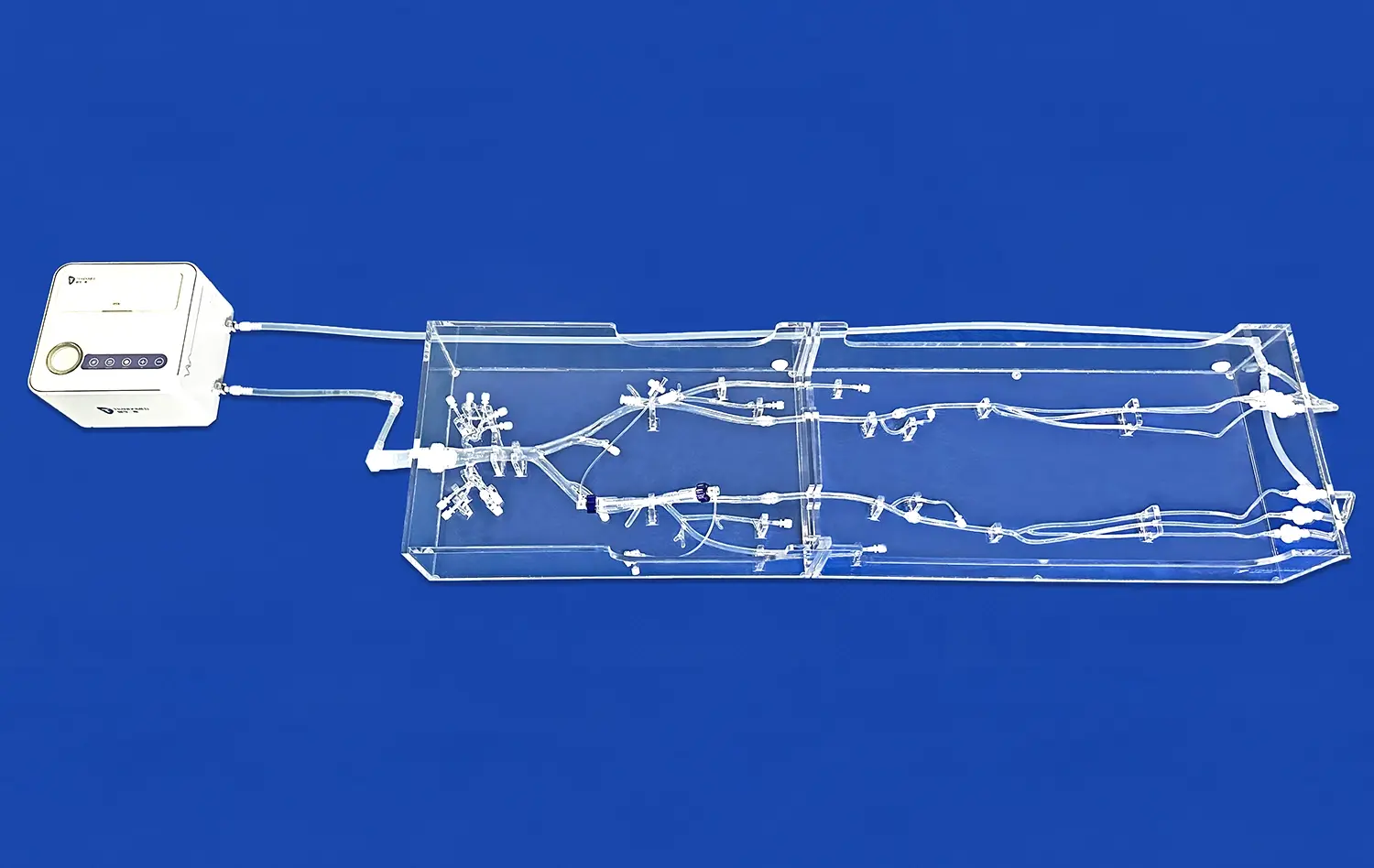
PCI training models have revolutionized the way cardiologists and interventional specialists prepare for complex coronary procedures. These advanced simulation tools provide a realistic environment for practicing intricate techniques without risk to patients. By replicating various coronary lesions with remarkable accuracy, PCI simulators enable healthcare professionals to hone their skills in treating challenging cardiac conditions. From mimicking stenoses and calcifications to recreating chronic total occlusions (CTOs) and bifurcations, these models offer invaluable hands-on experience. The ability to repeatedly practice on lifelike anatomies enhances procedural proficiency, decision-making abilities, and confidence among trainees and experienced practitioners alike. Moreover, these simulators allow for the exploration of novel treatment strategies and device testing in a controlled setting, ultimately leading to improved patient outcomes in real-world scenarios.
What Types of Lesions Can Be Replicated in PCI Training Models?
Stenoses and Occlusions
PCI training models are exceptionally adept at accurately simulating the full spectrum of coronary artery narrowing, ranging from subtle stenoses to total blockages (chronic total occlusions). These meticulously designed replicas present the identical physical challenges encountered in real procedures when traversing constricted vessel passages. Trainees gain invaluable hands-on experience manipulating guidewires, performing balloon angioplasty, and deploying stents within vessels exhibiting varying degrees of lumen restriction, directly preparing them for the demands of restoring blood flow in obstructed coronary arteries under realistic simulated conditions.
Calcified Lesions
Calcified deposits within coronary arteries pose distinct difficulties during PCI due to their extreme hardness. PCI training models integrate specialized materials that precisely mimic the density, rigidity, and resistance characteristic of actual calcified plaques. This crucial feature provides practitioners with authentic tactile feedback when attempting to cross, dilate, or stent these hardened lesions. Experiencing this resistance firsthand significantly enhances a clinician's ability to choose the most suitable devices and techniques, such as specialized balloons or atherectomy, to effectively manage calcification and achieve optimal procedural results.
Complex Morphologies
PCI simulators possess the advanced capability to replicate intricate and challenging lesion shapes and distributions, including eccentric stenoses (plaques not centered in the lumen), tandem lesions situated close together, and diffuse disease affecting long vessel segments. Practicing on these diverse and anatomically complex variations is essential for interventionalists to formulate effective strategies for addressing multi-faceted coronary blockages. This deliberate exposure allows operators to hone critical skills in detailed lesion assessment, judicious device selection, and comprehensive procedural planning tailored to specific morphological complexities encountered during interventions.
Realistic Modeling of CTOs, Bifurcations, and Calcifications
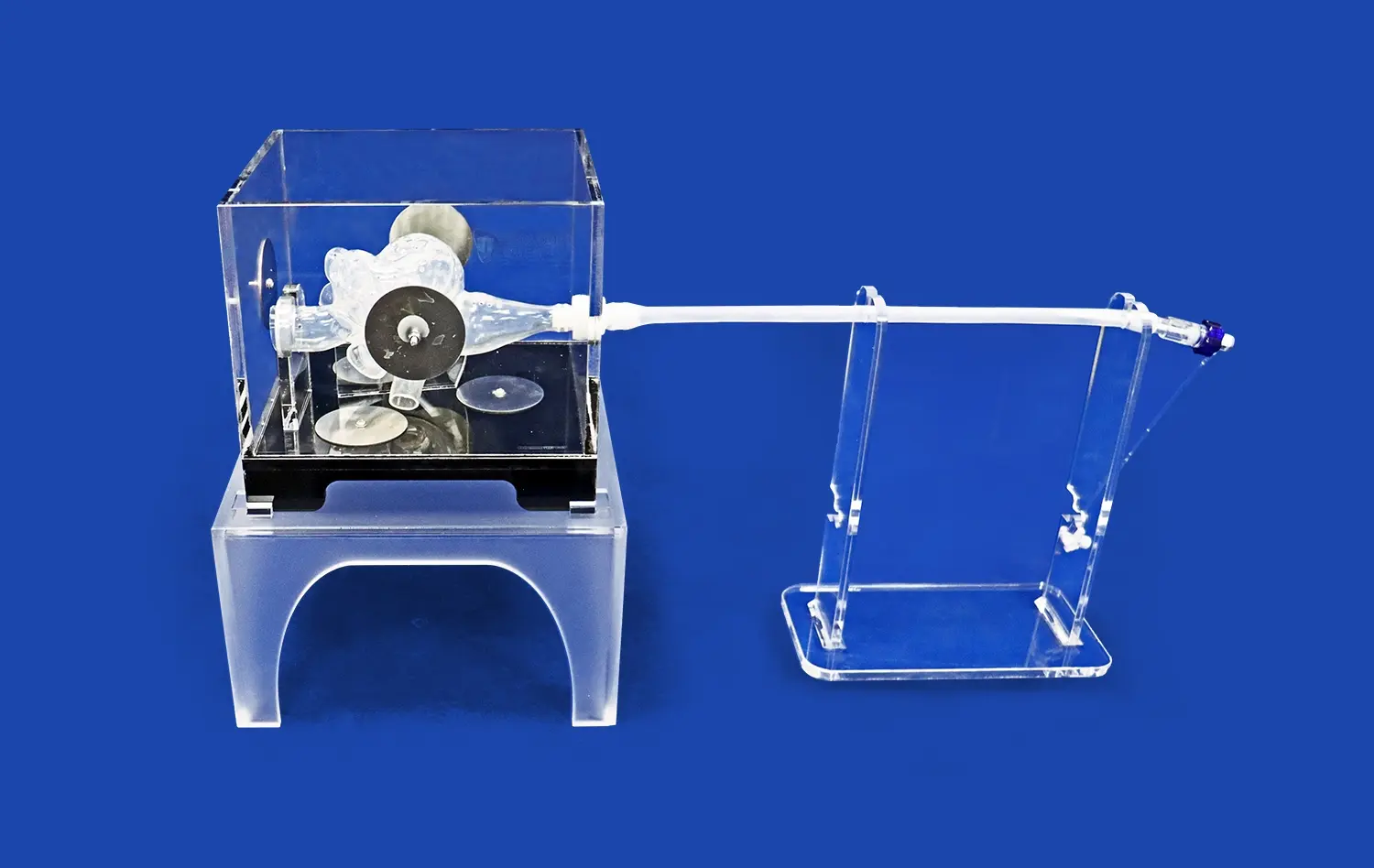
Chronic Total Occlusions (CTOs)
CTO interventions are among the most challenging procedures in interventional cardiology. PCI training models offer realistic representations of CTOs, complete with simulated microchannels and cap structures. These models allow operators to practice advanced wire techniques, such as antegrade and retrograde approaches, dissection re-entry methods, and the use of specialized CTO devices.
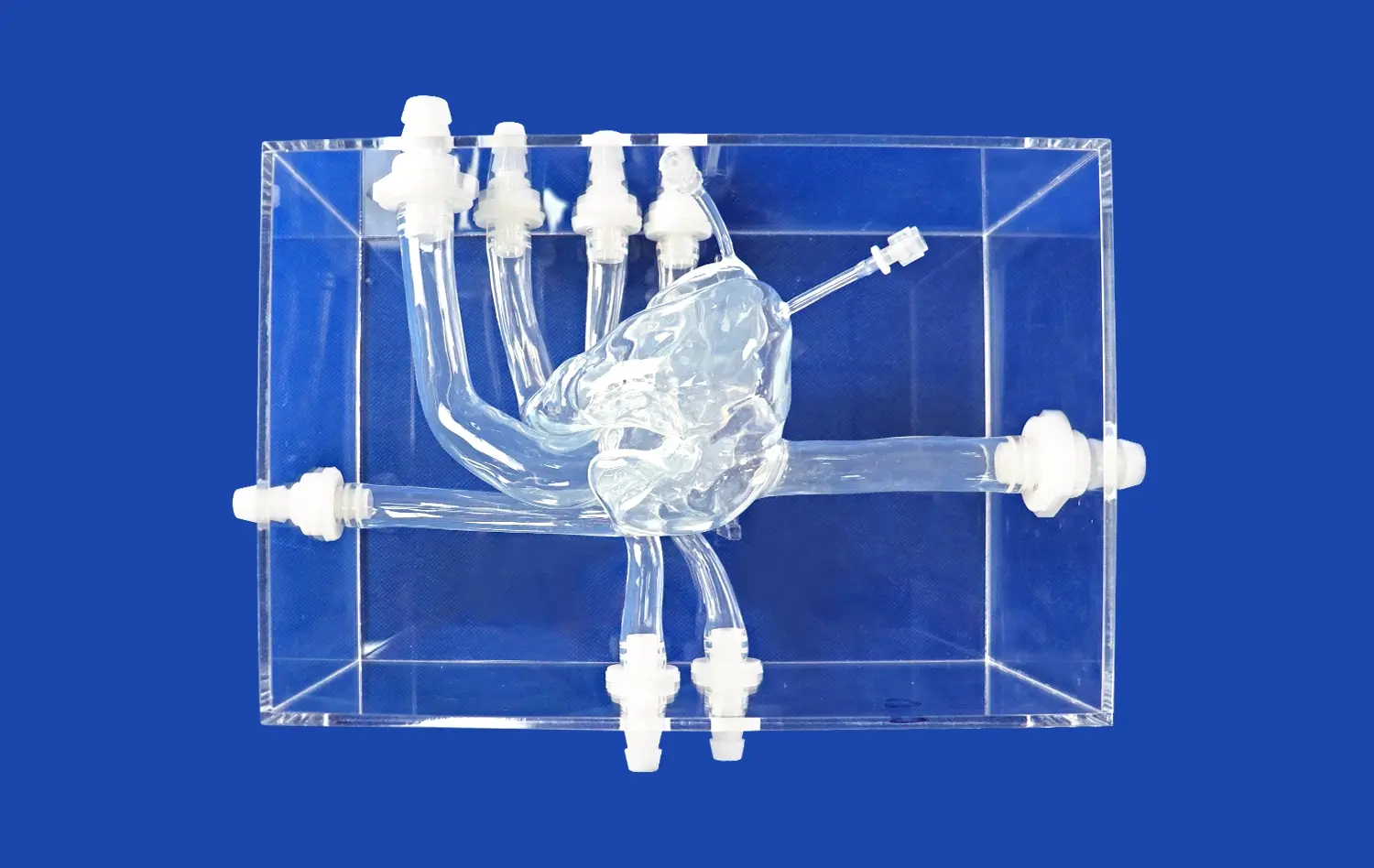
Bifurcation Lesions
Coronary bifurcations require careful management to ensure optimal treatment of both the main vessel and side branch. PCI training models featuring accurate bifurcation geometries enable practitioners to master complex stenting techniques like provisional stenting, two-stent strategies, and kissing balloon inflation. The ability to replicate various bifurcation angles and lesion distributions enhances the operator's ability to tackle these intricate scenarios.
Advanced Calcification Simulation
Modern PCI simulators incorporate sophisticated materials that mimic the properties of heavily calcified lesions. These models allow interventionalists to practice calcium modification techniques, including rotational atherectomy, orbital atherectomy, and intravascular lithotripsy. The realistic tactile feedback provided by these simulations helps operators develop the finesse required for managing challenging calcified lesions effectively.
Enhancing Treatment Strategies Through Lesion-Specific Simulation
Tailored Procedural Approaches
Lesion-specific simulations enable interventionalists to develop and refine tailored treatment strategies for each unique coronary anatomy. By practicing on a wide range of lesion types, operators can build a comprehensive toolkit of techniques and approaches. This versatility translates directly to improved decision-making and procedural success rates in clinical practice.
Device Selection and Optimization
PCI training models serve as invaluable platforms for testing and optimizing various interventional devices. Practitioners can experiment with different guidewires, balloons, stents, and specialized tools to determine the most effective combinations for specific lesion characteristics. This hands-on experience aids in selecting the most appropriate devices for each unique patient scenario.
Complication Management
Advanced PCI simulators can replicate potential procedural complications, such as dissections, perforations, or acute vessel closure. These scenarios provide crucial opportunities for operators to practice rapid decision-making and emergency management techniques in a controlled environment. By repeatedly encountering and resolving simulated complications, interventionalists can build the confidence and skills necessary to handle unexpected events during live procedures.
Conclusion
PCI training models have emerged as indispensable tools in the education and skill development of interventional cardiologists. By providing realistic simulations of complex coronary lesions, these advanced platforms bridge the gap between theoretical knowledge and practical expertise. The ability to replicate a wide range of lesion types, from simple stenoses to challenging CTOs and calcifications, allows for comprehensive training and experimentation with various treatment strategies. As technology continues to evolve, PCI simulators will play an increasingly vital role in shaping the future of coronary interventions, ultimately leading to improved patient care and outcomes.
Contact us
Experience the cutting-edge in PCI training technology with Trandomed's state-of-the-art simulators. Our advanced 3D-printed silicone models offer unparalleled realism and versatility for interventional cardiology training. Elevate your skills, explore innovative techniques, and prepare for complex procedures in a risk-free environment. To learn more about our customizable PCI training solutions and how they can benefit your institution, contact us at jackson.chen@trandomed.com.
References
1. Schmitz, C., et al. (2020). "Simulation-based training in coronary angiography and intervention." Journal of Interventional Cardiology, 33(4), 352-362.
2. Krishnasamy, V., et al. (2019). "The utility of coronary artery models for training in percutaneous coronary intervention." Catheterization and Cardiovascular Interventions, 93(7), 1240-1246.
3. Eckhouse, S. R., et al. (2021). "Advancements in percutaneous coronary intervention simulation models." Progress in Cardiovascular Diseases, 66, 41-49.
4. Manivannan, M., et al. (2018). "Virtual reality simulation in interventional cardiology training." Heart, 104(19), 1542-1547.
5. Jensen, U. J., et al. (2022). "The impact of simulation-based training on clinical outcomes in percutaneous coronary intervention." EuroIntervention, 17(14), 1168-1175.
6. Tarar, M. N., et al. (2020). "Role of simulation in interventional cardiology training." Cardiovascular Revascularization Medicine, 21(8), 962-968.