What Challenges Do CTOs and Bifurcations Present in Training?
Navigating Complex Anatomy
CTOs and bifurcation lesions represent some of the most challenging scenarios in interventional cardiology. The intricate anatomy of these lesions demands exceptional skill and precision. CTOs often involve long segments of completely blocked arteries with calcified or fibrotic tissue, making them resistant to traditional wire-crossing techniques. Bifurcations, where one artery branches into two, present unique challenges in maintaining blood flow to both branches while treating the lesion. Training for these procedures requires a deep understanding of three-dimensional vascular geometry and the ability to manipulate devices in confined spaces.
Mastering Specialized Techniques
Interventional cardiologists must master a range of specialized techniques to tackle CTOs and bifurcations effectively. For CTOs, this includes antegrade and retrograde approaches, dissection re-entry techniques, and the use of dedicated CTO wires and microcatheters. Bifurcation procedures may involve complex stenting strategies such as culotte, crush, or T-stenting techniques. Each of these methods requires precise coordination of multiple devices and an understanding of how to adapt strategies based on lesion characteristics. The PCI training model often falls short in providing adequate practice for these advanced techniques.
Managing Procedural Complications
The risk of complications is significantly higher in CTO and bifurcation procedures compared to routine PCI. Potential issues include vessel perforation, dissection, side branch occlusion, and equipment entrapment. Training must prepare physicians to recognize early signs of complications and respond swiftly with appropriate interventions. This aspect of training is particularly challenging, as it requires exposure to a wide range of potential scenarios and the development of quick decision-making skills under pressure.
Simulating Complex Lesion Morphologies with Anatomical Precision
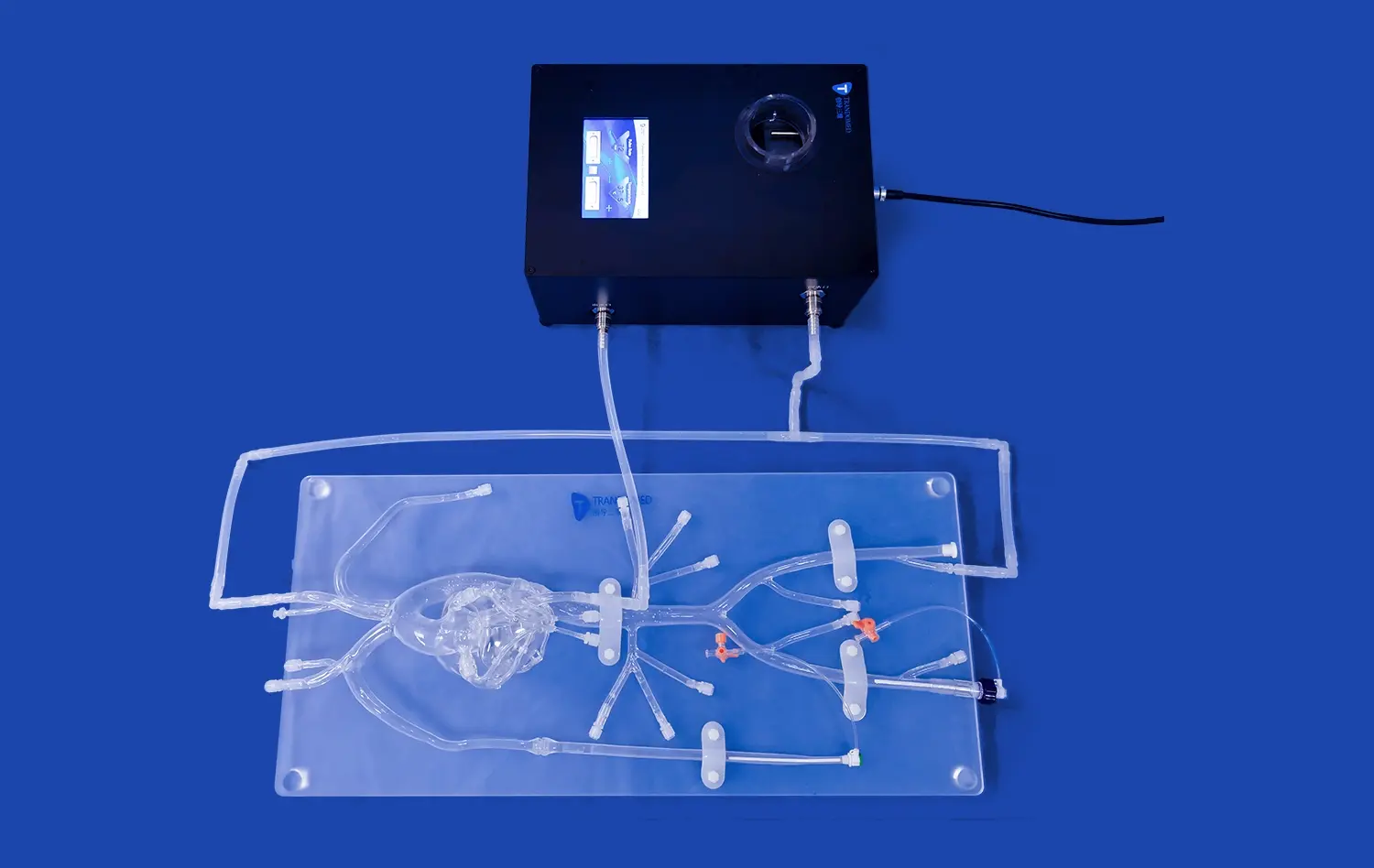
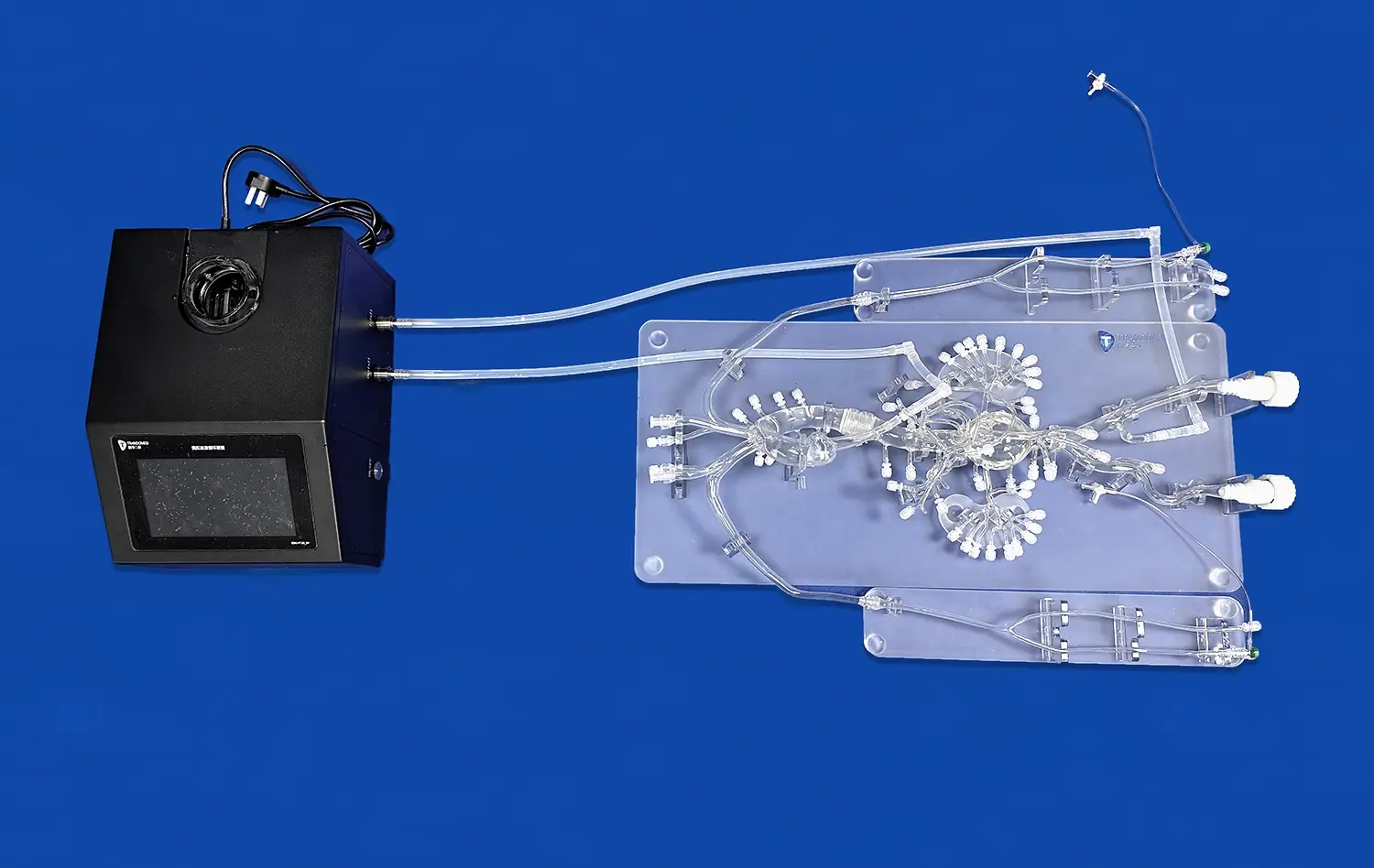
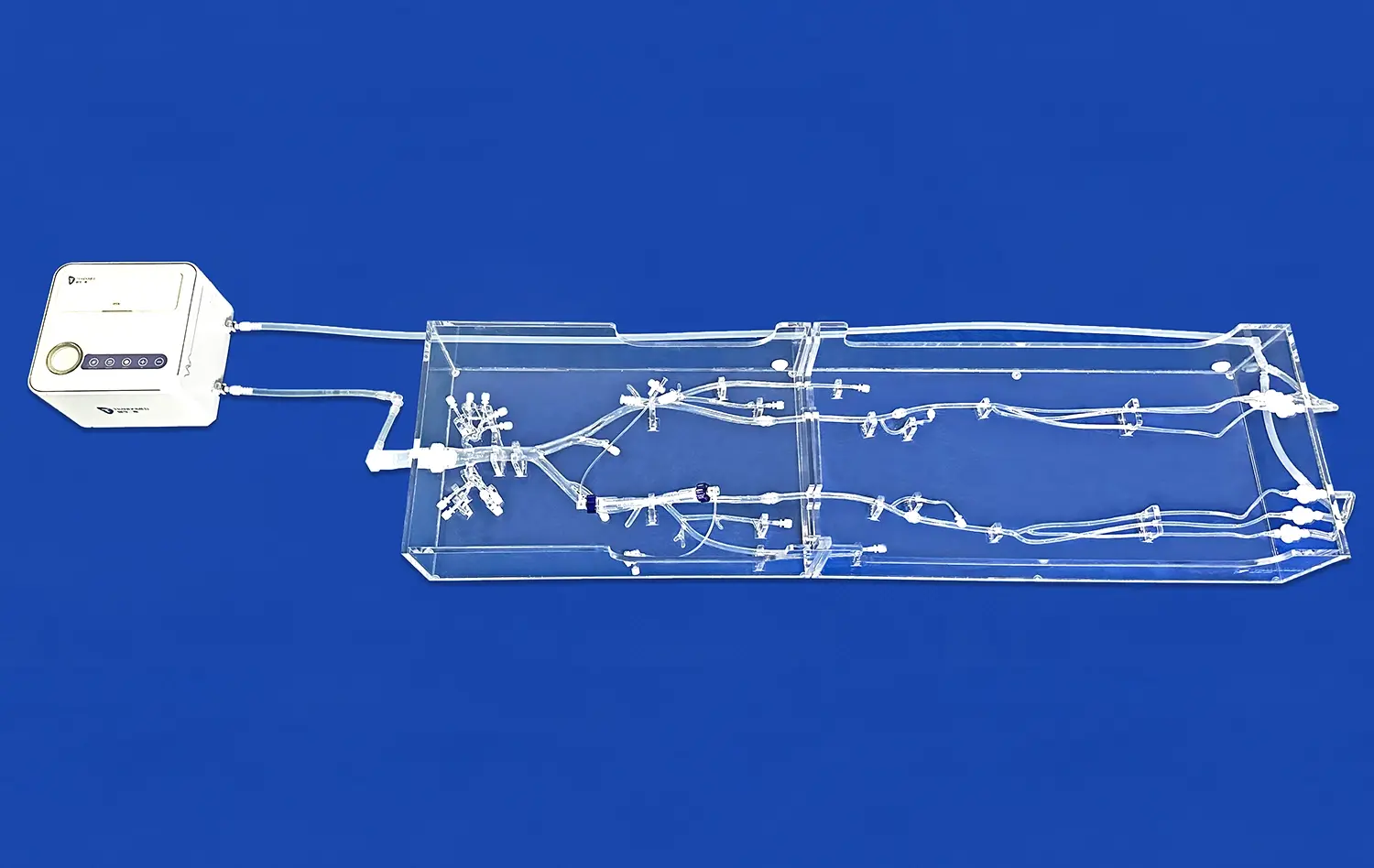
Advanced 3D Printing Technology
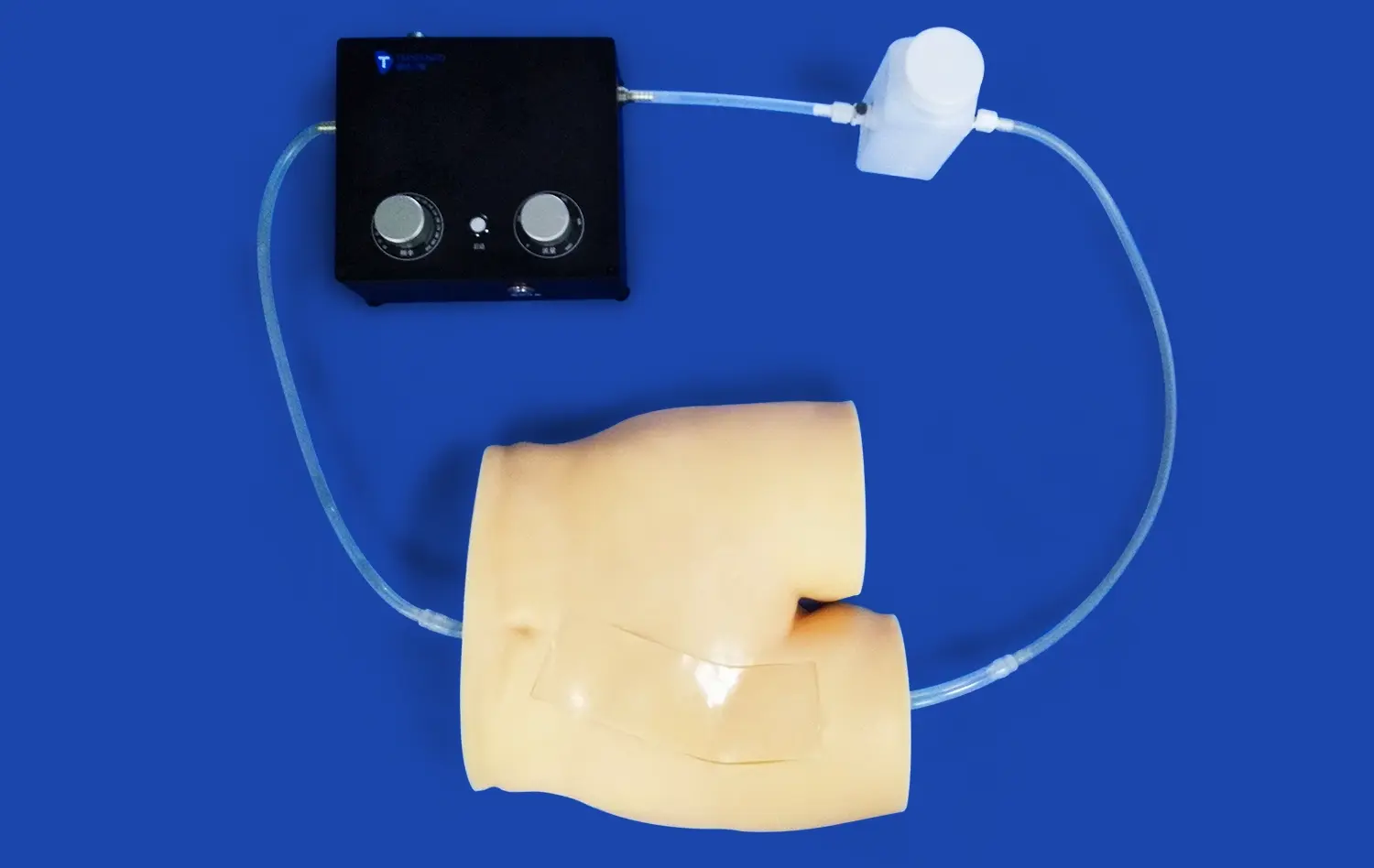
Modern PCI training models leverage cutting-edge 3D printing technology to create highly accurate representations of coronary anatomy. These models are often based on real patient CT and MRI data, ensuring that trainees encounter the same level of anatomical variation and complexity they would face in clinical practice. The ability to reproduce specific lesion characteristics, such as calcification patterns in CTOs or the precise angles of bifurcation branches, allows for targeted practice of challenging scenarios.
Customizable Lesion Scenarios
One of the key advantages of advanced PCI training models is their customizability. Manufacturers like Trandomed offer the ability to adjust the length, severity, and location of coronary artery stenoses, bifurcations, or embolisms to meet specific training needs. This flexibility allows institutions to create a diverse range of training scenarios, from straightforward lesions for beginners to highly complex cases for experienced operators looking to push their skills further. The ability to practice on models that closely mimic the unique challenges of individual patient cases is invaluable for pre-procedural planning and skill refinement.
Integration of Imaging Simulation
To enhance the realism of training, many PCI models now incorporate simulated imaging systems that replicate the fluoroscopic views used during actual procedures. These integrated systems allow trainees to practice interpreting angiographic images in real-time while manipulating devices within the model. This feature is particularly important for CTO and bifurcation procedures, where success often depends on the operator's ability to navigate based on limited visual information and to use advanced imaging techniques such as intravascular ultrasound (IVUS) or optical coherence tomography (OCT).
Building Procedural Expertise Through Repeated Model-Based Practice
Iterative Skill Development
PCI training models enable a level of repetitive practice that is simply not possible in clinical settings. This iterative approach to skill development is crucial for mastering the complex techniques required for CTO and bifurcation interventions. Trainees can attempt the same procedure multiple times, refining their approach with each iteration. This process allows for the development of muscle memory and intuitive decision-making skills that are essential for success in challenging cases. Moreover, the ability to practice without time pressure or patient risk encourages experimentation with different strategies and devices.
Objective Performance Assessment
Many advanced PCI training models and systems incorporate features for objective performance assessment. These may include metrics such as procedure time, fluoroscopy time, contrast volume used, and successful achievement of predefined procedural goals. By providing quantitative feedback, these models allow trainees to track their progress over time and identify areas for improvement. This data-driven approach to skill assessment is particularly valuable for complex procedures like CTOs and bifurcations, where small improvements in technique can lead to significant gains in procedural success and patient outcomes.
Team-Based Training Scenarios
Successful management of complex PCI cases often requires effective teamwork between the primary operator, assisting physicians, and support staff. PCI training models can be used to create realistic team-based training scenarios that simulate the catheterization laboratory environment. These exercises help develop critical non-technical skills such as communication, leadership, and crisis management. For CTO and bifurcation procedures, which often involve prolonged table times and potential complications, the ability to practice as a cohesive team can significantly enhance overall performance and patient safety.
Conclusion
PCI training models have emerged as indispensable tools for preparing interventional cardiologists to tackle the challenges of CTO and bifurcation procedures. By providing a realistic, customizable, and risk-free environment for practice, these models enable physicians to develop the advanced skills and confidence necessary for success in complex interventions. As the field of interventional cardiology continues to evolve, the role of high-fidelity simulation in training and skill maintenance will only grow in importance, ultimately leading to improved patient care and outcomes.
Contact Us
For cutting-edge PCI training solutions that support advanced procedural practice, look no further than Trandomed. Our state-of-the-art simulators offer unparalleled realism and customization options to meet your specific training needs. Experience the future of interventional cardiology education and take your skills to the next level. Contact us today at jackson.chen@trandomed.com to learn more about our innovative PCI training models and how they can enhance your training program.
_1736214519364.webp)