What Are the Diagnostic Challenges in Pulmonary Arterial Hypertension?
Complex Symptomatology and Mimicking Conditions
Diagnosing Pulmonary Arterial Hypertension (PAH) presents numerous challenges due to its complex symptomatology. The initial symptoms of PAH, such as shortness of breath, fatigue, and chest pain, are often non-specific and can mimic other cardiopulmonary conditions. This similarity in presentation can lead to misdiagnosis or delayed diagnosis, potentially allowing the disease to progress unchecked. The subtle nature of early PAH symptoms requires clinicians to maintain a high index of suspicion and consider PAH in their differential diagnosis when evaluating patients with unexplained dyspnea or exercise intolerance.
Limitations of Non-Invasive Diagnostic Tools
While non-invasive diagnostic tools play a crucial role in the initial evaluation of suspected PAH, they have inherent limitations. Echocardiography, a commonly used screening tool, can estimate pulmonary artery pressure but may not always provide accurate measurements, especially in patients with certain cardiac anomalies or obesity. Chest radiographs and electrocardiograms can suggest the presence of PAH but lack specificity. Even advanced imaging techniques like CT angiography and ventilation-perfusion scans, while valuable for ruling out other conditions, may not definitively diagnose PAH in its early stages. These limitations underscore the need for more sophisticated diagnostic approaches, such as the pulmonary artery model, and training methodologies.
Necessity of Invasive Hemodynamic Assessment
The gold standard for diagnosing PAH remains right heart catheterization (RHC), an invasive procedure that directly measures pulmonary artery pressure and blood flow. However, RHC carries inherent risks and requires specialized skills to perform and interpret accurately. The complexity of this procedure and the potential for complications highlight the importance of thorough training and practice for clinicians. This is where pulmonary artery models become invaluable, offering a safe environment for practitioners to refine their catheterization techniques and improve their ability to interpret hemodynamic data accurately.
Simulating Hemodynamic Measurements and Pressure Assessment
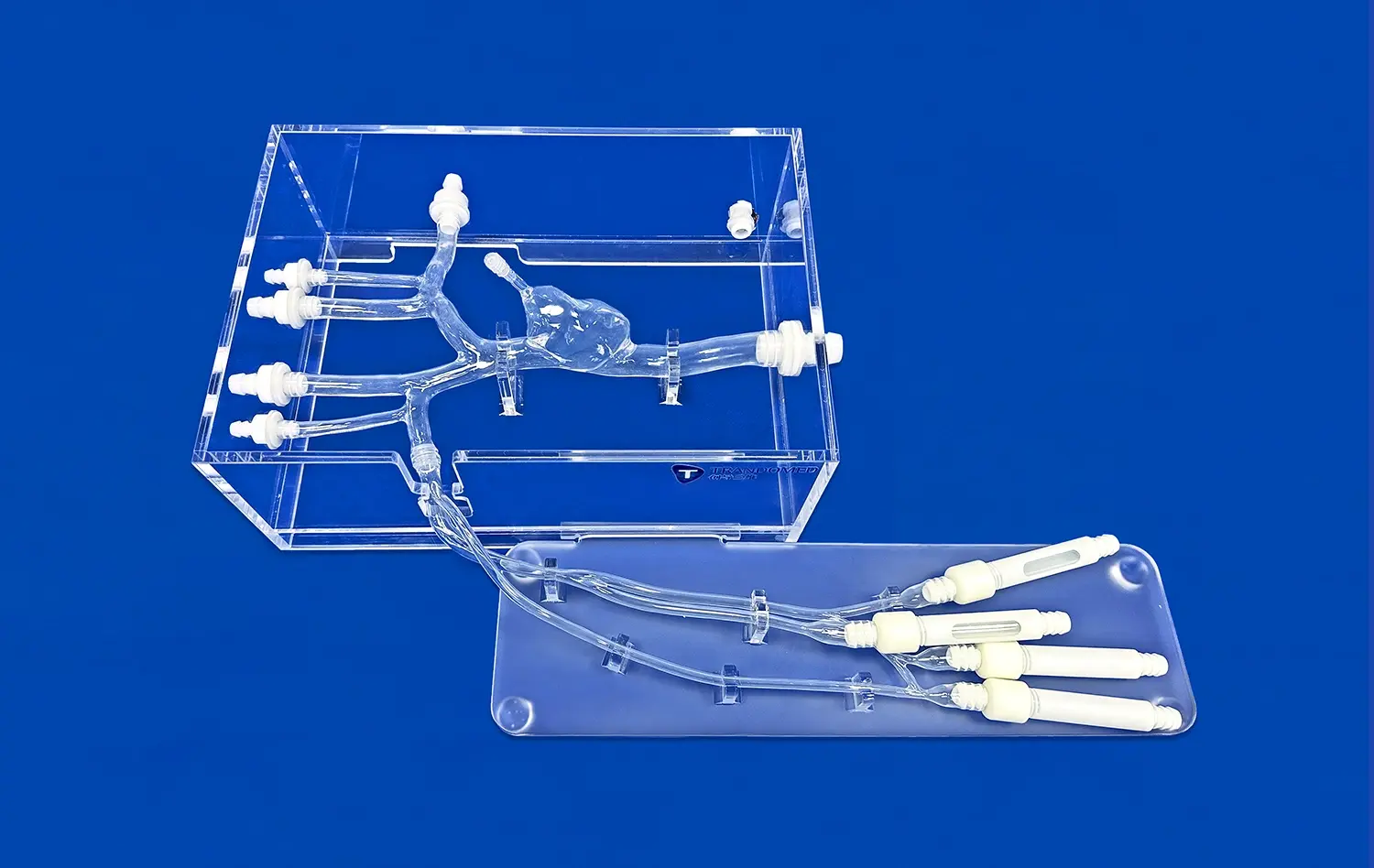
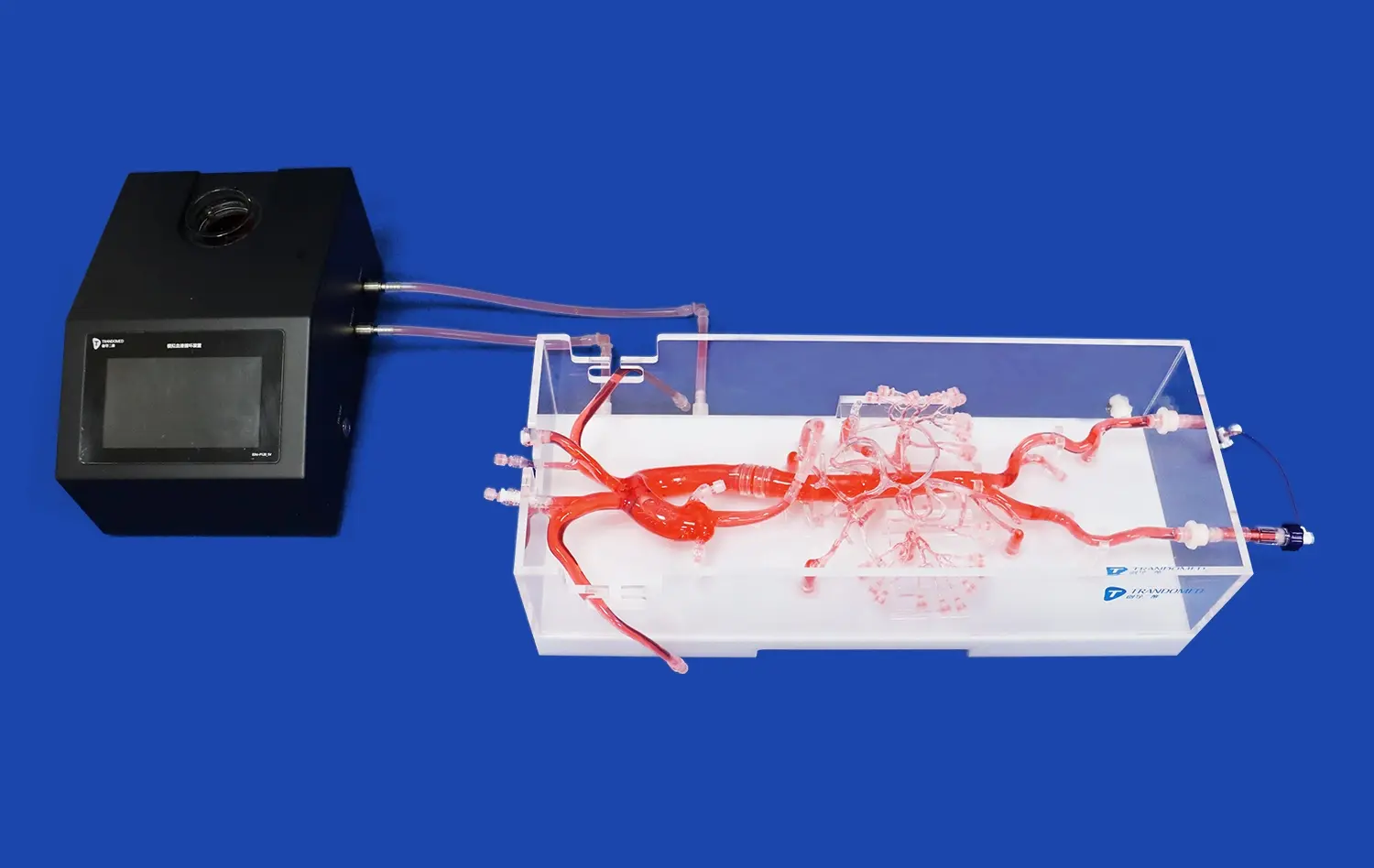
Replicating Physiological Conditions
Advanced pulmonary artery models, such as those developed by Trandomed, excel in replicating the physiological conditions found in PAH. These models are designed with meticulous attention to anatomical detail, incorporating features like the intricate branching patterns of the pulmonary arteries and the variable vessel diameters characteristic of PAH. By simulating different stages of the disease, from early onset to advanced cases, these models allow clinicians to experience a wide range of scenarios they might encounter in clinical practice. The ability to adjust parameters such as vessel compliance and resistance enables the creation of patient-specific simulations, further enhancing the educational value of these tools.
Pressure Measurement and Waveform Analysis
One of the key advantages of using pulmonary artery models in PAH diagnosis training is the ability to practice pressure measurement and waveform analysis. These models can be equipped with sensors that provide real-time pressure readings, mimicking the data obtained during right heart catheterization. Trainees can learn to navigate the catheter through the simulated vasculature, position it correctly for accurate measurements, and interpret the pressure waveforms characteristic of PAH. This hands-on experience is crucial for developing the skills necessary to differentiate between normal pulmonary artery pressures and those indicative of PAH, as well as recognizing patterns that suggest disease severity or complications.
Cardiac Output and Vascular Resistance Calculations
Beyond pressure measurements, pulmonary artery models facilitate practice in calculating important hemodynamic parameters such as cardiac output and pulmonary vascular resistance. These calculations are essential for accurately diagnosing PAH and assessing its severity. By incorporating flow sensors and allowing for the manipulation of various physiological variables, these models enable trainees to understand the relationships between pressure, flow, and resistance in the pulmonary circulation. This comprehensive approach to hemodynamic assessment enhances the clinician's ability to make informed decisions about patient management and treatment strategies based on a thorough understanding of the underlying pathophysiology.
Enhancing Treatment Planning Through Repeated Model-Based Practice
Procedural Skill Development
Pulmonary artery models serve as an exceptional platform for developing and refining procedural skills critical in PAH management. These models allow clinicians to practice a wide array of interventional techniques, from basic catheter manipulation to more complex procedures such as balloon atrial septostomy or pulmonary angioplasty. The tactile feedback provided by high-fidelity silicone models closely mimics the feel of real tissue, enabling practitioners to develop the dexterity and precision required for successful interventions. Repeated practice on these models helps build muscle memory and confidence, potentially reducing procedure times and complication rates in actual patient care scenarios.
Treatment Response Simulation
One of the most valuable aspects of pulmonary artery models in PAH management is their ability to simulate treatment responses. These models can be programmed to replicate the hemodynamic changes that occur with various therapeutic interventions, such as vasodilator therapy or mechanical circulatory support. By observing and analyzing these simulated responses, clinicians can better understand the potential effects of different treatment modalities on pulmonary hemodynamics. This capability allows for the exploration of various treatment strategies in a controlled environment, helping clinicians make more informed decisions about patient care and potentially improving treatment outcomes.
Complication Management and Crisis Scenarios
Pulmonary artery models also play a crucial role in preparing clinicians for managing complications and crisis scenarios associated with PAH and its treatment. These models can be configured to simulate rare but critical events such as acute right heart failure, pulmonary artery rupture, or severe hypoxemia during procedures. By practicing these high-stakes scenarios in a risk-free environment, healthcare teams can develop and refine their crisis management skills, improve team communication, and establish effective protocols for emergency situations. This type of simulation-based training is invaluable for building the confidence and competence necessary to handle complex cases and unexpected complications in real-world clinical settings.
Conclusion
Pulmonary artery models have emerged as indispensable tools in improving PAH diagnosis and treatment skills. By providing a realistic, risk-free environment for practice, these models address the complex challenges associated with PAH management. From enhancing diagnostic accuracy through simulated hemodynamic assessments to refining treatment strategies via repeated procedural practice, these models contribute significantly to clinical competence. As medical education continues to evolve, the integration of such advanced simulation technologies promises to elevate the standard of care for PAH patients, ultimately leading to improved outcomes and quality of life for those affected by this challenging condition.
Contact Us
Elevate your PAH diagnosis and treatment skills with Trandomed's cutting-edge pulmonary artery models. Our advanced silicone simulators offer unparalleled realism and versatility, enabling you to practice complex procedures and enhance your clinical decision-making. Experience the future of medical education and improve patient outcomes. For more information on our innovative medical simulation products, contact us at jackson.chen@trandomed.com.

_1736215128474.webp)
 (SJ001D)_1734504338727.webp)