What Role Do 3D Artery Models Play in Developing Surgical Precision?
Enhanced Anatomical Understanding
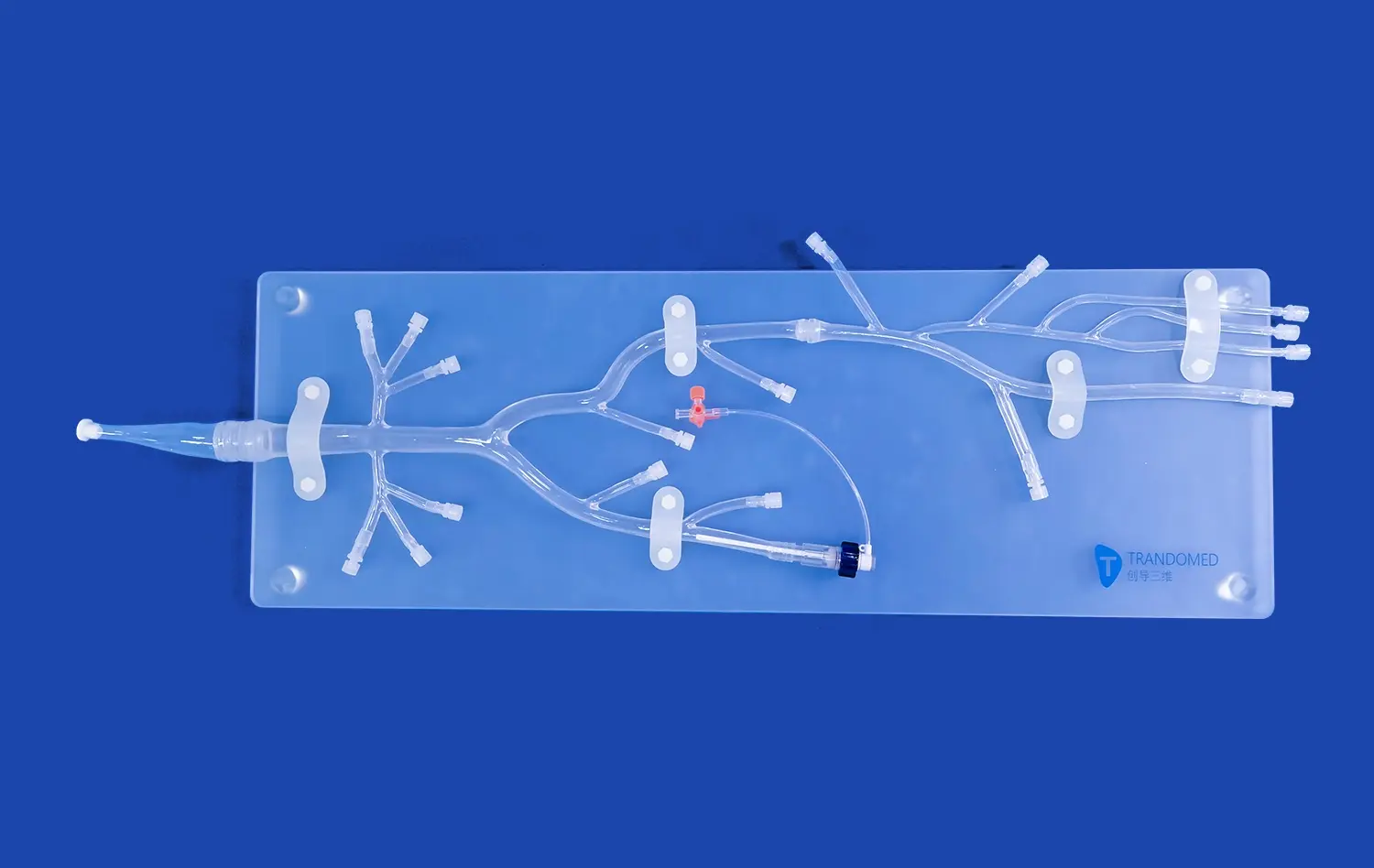
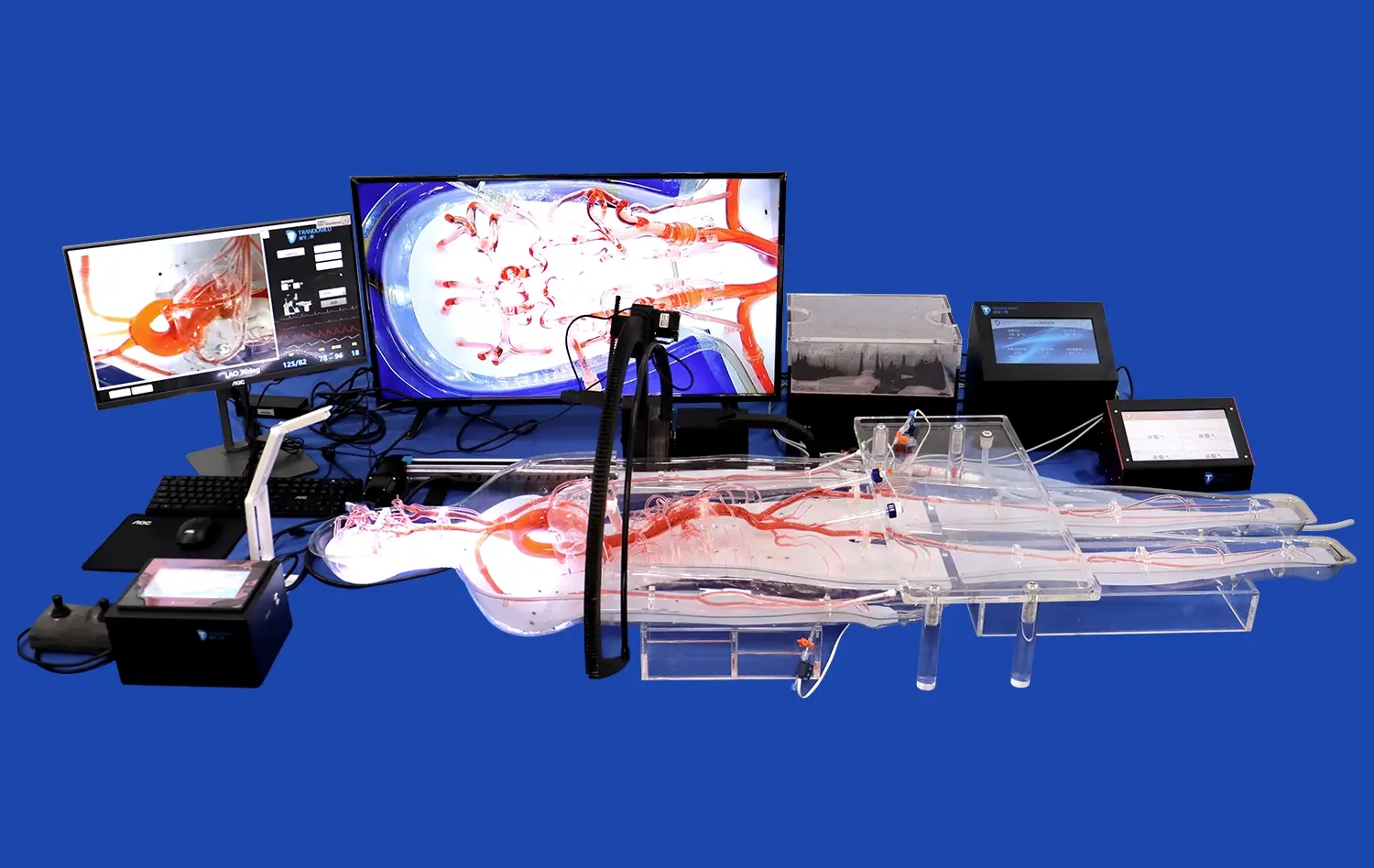
3D artery models, particularly those designed to replicate the lower extremity vasculature, provide an unparalleled opportunity for surgeons to study complex vessel networks in a realistic and interactive way. Unlike flat imaging, these models enable detailed observation of vessel curvature, branching, and spatial orientation. The tactile feedback of silicone-based materials closely mimics human tissue, enhancing spatial awareness and depth perception. This hands-on experience deepens anatomical comprehension, preparing trainees to navigate delicate vascular pathways with greater confidence and precision.
Procedural Rehearsal and Skill Refinement
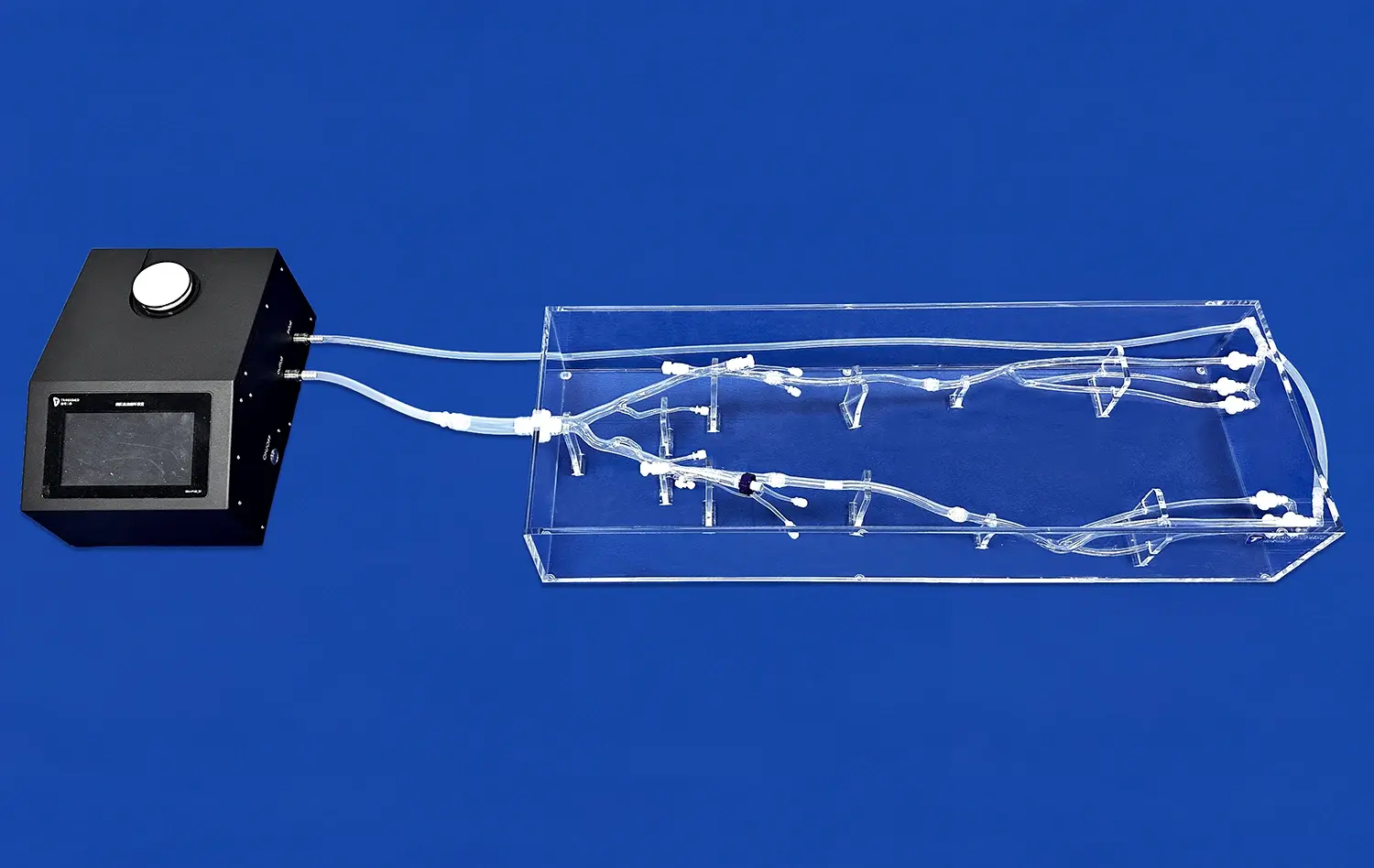
Using a lower extremity artery model, surgeons can repeatedly simulate intricate procedures such as angioplasty, stenting, or bypass grafting. Each rehearsal helps refine fine motor skills, improve instrument handling, and reinforce procedural accuracy. The controlled, risk-free environment encourages experimentation with different techniques and devices. Over time, this repetitive practice enhances muscle memory and decision-making under pressure, directly translating into improved surgical precision and reduced complication rates during real-life vascular operations.
Customized Learning Experiences
The integration of 3D printing with medical imaging allows for the creation of patient-specific artery models that accurately reflect individual anatomy. These personalized replicas let surgeons analyze challenging cases in advance, plan optimal intervention strategies, and rehearse procedures tailored to the patient's condition. Practicing on a customized lower extremity artery model enhances preparedness and adaptability in the operating room. This individualized approach not only shortens operative times but also increases procedural safety and overall patient outcomes.
Performance Assessment Through High-Fidelity Simulation
Objective Evaluation Metrics
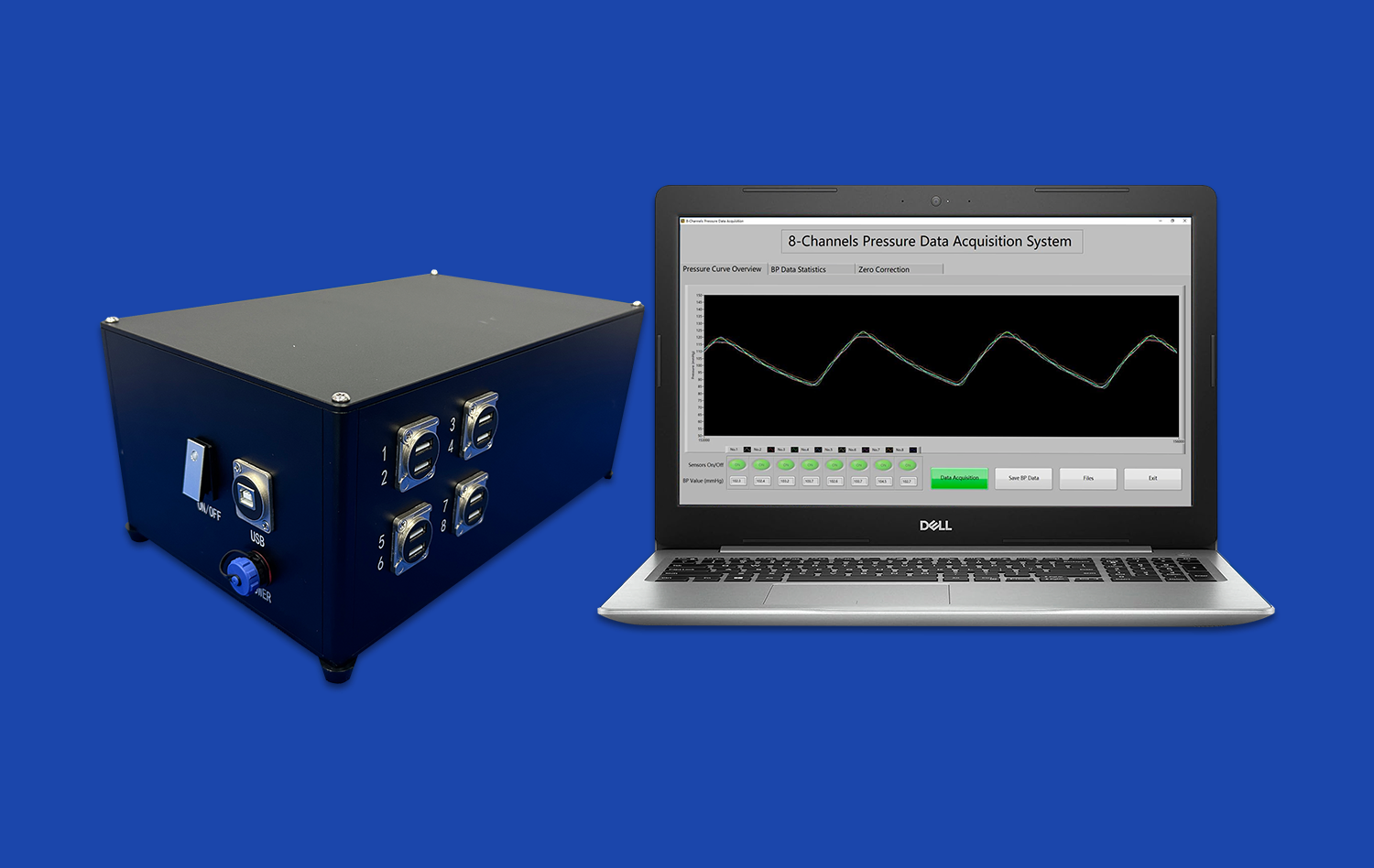
High-fidelity artery simulations offer educators a reliable and standardized way to measure surgical performance objectively. By tracking quantitative indicators such as procedural duration, precision of catheter or stent placement, and management of simulated complications, instructors can assess both technical proficiency and decision-making. These objective metrics enable consistent benchmarking across trainees, helping identify strengths and areas for improvement. Over time, this data-driven evaluation supports personalized training pathways that enhance overall surgical competency and readiness for clinical practice.
Scenario-Based Training
Advanced artery models, such as the lower extremity artery model, enable realistic simulation of diverse clinical situations, from standard interventions to rare or high-risk complications. Trainees can practice navigating tortuous arteries, managing sudden occlusions, or responding to simulated bleeding events. Each scenario challenges participants to think critically, adapt quickly, and apply evidence-based techniques under pressure. Exposure to such varied conditions builds resilience, sharpens judgment, and prepares surgeons to perform confidently in unpredictable real-world vascular procedures and emergency environments.
Feedback and Debriefing
Simulation sessions using high-fidelity artery models allow for structured feedback and interactive debriefing immediately after practice. Instructors can review performance step by step, emphasizing key procedural moments, identifying technical errors, and discussing alternative strategies. This reflective process deepens comprehension of vascular techniques and promotes continuous improvement. Immediate correction and discussion reinforce learning retention, helping trainees refine their approach, strengthen procedural accuracy, and develop the confidence necessary for complex surgical interventions.
How Advanced Models Contribute to Better Patient Safety and Outcomes?
Risk Reduction Through Pre-operative Planning
Patient-specific artery models, particularly those focusing on the lower extremities, enable surgeons to meticulously plan interventions before entering the operating room. By studying these accurate 3D representations, practitioners can anticipate potential challenges, select appropriate devices, and determine optimal access points. This thorough preparation minimizes the risk of intraoperative complications and reduces procedure times, ultimately enhancing patient safety.
Improved Procedural Efficiency
Regular training with high-fidelity artery models, such as the lower extremity artery model, leads to increased procedural efficiency. Surgeons who have honed their skills on these simulators typically demonstrate smoother instrument handling, quicker decision-making, and more confident execution of techniques. This improved efficiency translates to shorter operative times, reduced anesthesia exposure, and potentially faster patient recovery.
Enhanced Communication and Informed Consent
Realistic 3D artery models serve as valuable tools for patient education and obtaining informed consent. Surgeons can use these tangible representations to explain planned procedures, potential risks, and expected outcomes to patients and their families. This visual aid improves understanding, facilitates meaningful discussions, and helps patients make more informed decisions about their care.
Conclusion
The integration of realistic artery models, such as the lower extremity artery model, particularly those focusing on lower extremity vasculature, has markedly improved vascular surgery training outcomes. These advanced simulators enhance anatomical understanding, provide a platform for skill refinement, and enable objective performance assessment. By facilitating thorough pre-operative planning and improving procedural efficiency, these models contribute significantly to patient safety and surgical outcomes. As medical simulation technology continues to evolve, the role of high-fidelity artery models in vascular surgery education and clinical practice is set to become even more pivotal, shaping the future of vascular interventions and patient care.
Contact Us
At Trandomed, we are at the forefront of developing cutting-edge 3D printed medical simulators, including highly realistic lower extremity artery models. Our advanced manufacturing processes and commitment to innovation ensure that our products meet the exacting standards required for effective surgical training. As a leading supplier and manufacturer in this field, we offer customizable solutions to meet the unique needs of medical institutions worldwide. Experience the difference that our high-fidelity models can make in your vascular surgery training program. For more information or to discuss your specific requirements, please contact us at jackson.chen@trandomed.com.

_1734504197376.webp)
_1735798438356.webp)