Translating Simulation-Based Skills to Real-World Procedures
Enhancing Procedural Competence through Repetitive Practice
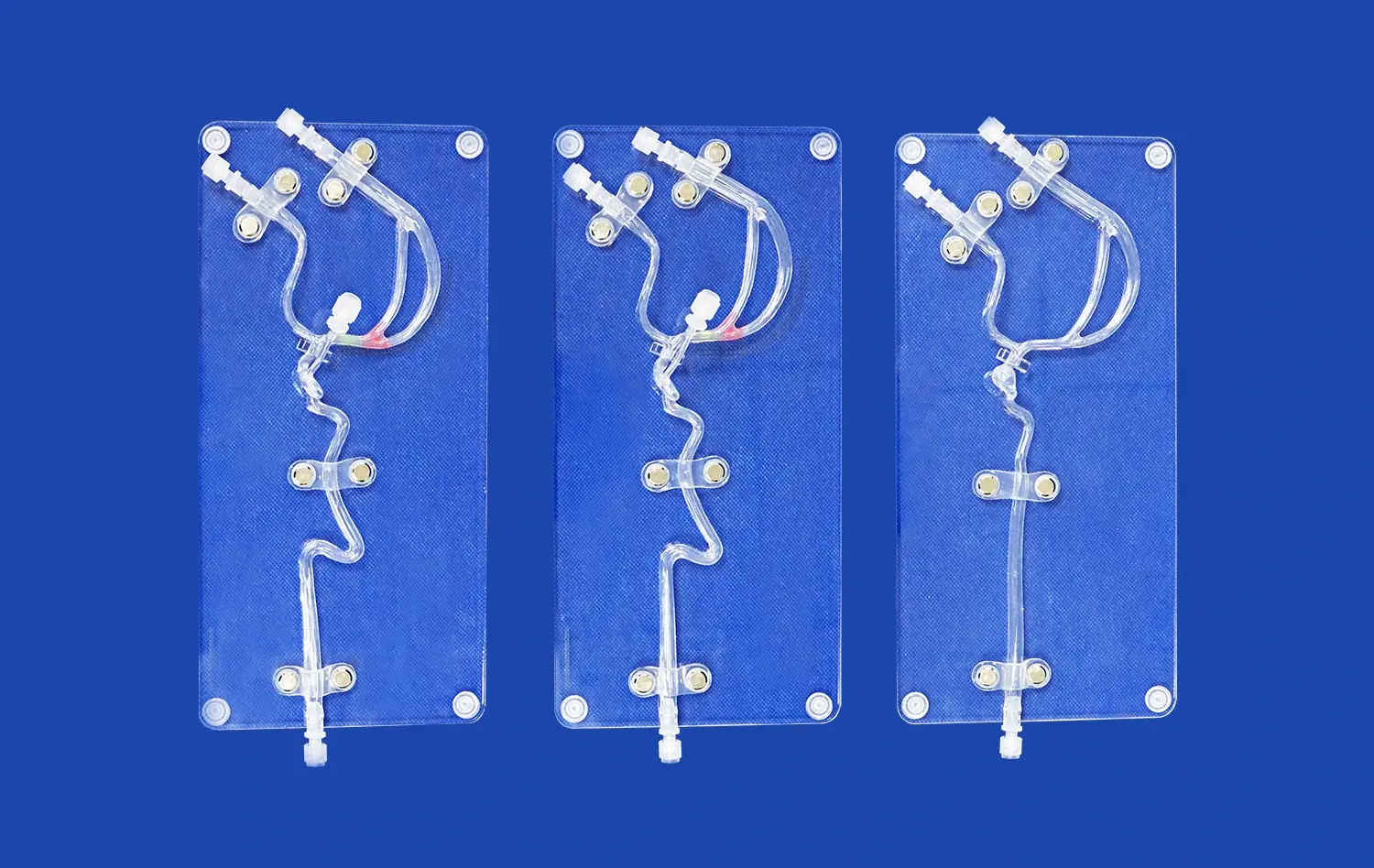
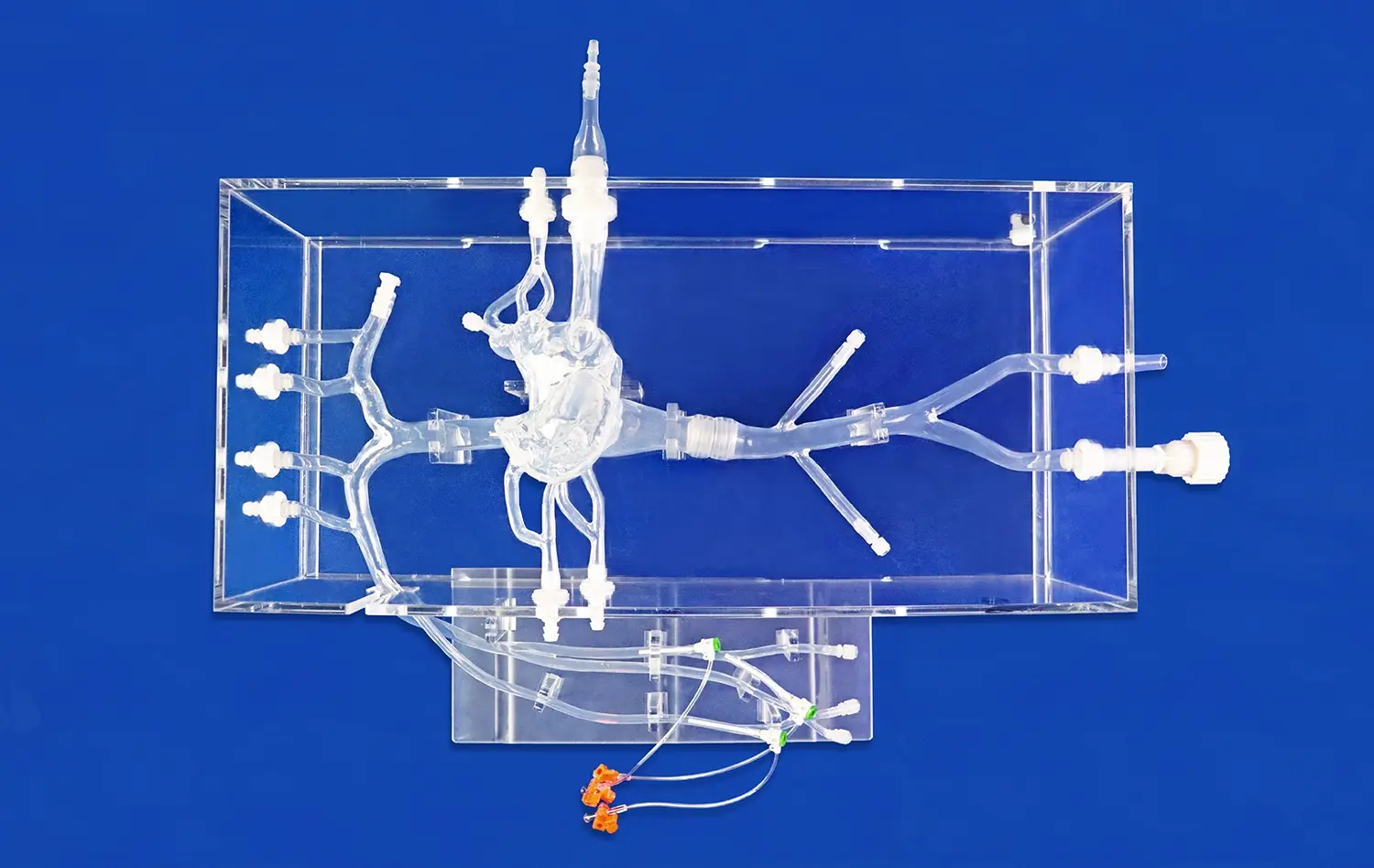
The abdominal vascular simulator plays a pivotal role in developing procedural competence among medical trainees and practicing clinicians. By offering a platform for repetitive practice, the model allows users to refine their techniques in a controlled environment. This iterative process is crucial for mastering complex vascular interventions, such as catheterization and stent placement. The model's high-fidelity design, featuring accurate representations of the celiac trunk, hepatic artery, and renal arteries, ensures that the skills acquired during simulation closely mirror those required in actual surgical scenarios.
Customizable Pathological Scenarios for Comprehensive Training
One of the standout features of advanced abdominal vascular models is their ability to simulate various pathological conditions. Manufacturers like Trandomed offer customization options, allowing educators to create specific scenarios tailored to their training objectives. For instance, models can be modified to represent stenosis in the renal arteries or aneurysms in the abdominal aorta. This versatility enables trainees to encounter and manage a wide array of clinical situations, preparing them for the diverse challenges they may face in real-world practice.
Bridging the Gap Between Theoretical Knowledge and Practical Application
The abdominal vascular model serves as a crucial link between theoretical knowledge and practical application in vascular medicine. While textbooks and lectures provide essential foundational knowledge, the model offers a tangible means of applying this information. Trainees can visualize complex anatomical relationships, understand the spatial orientation of vessels, and practice decision-making in a three-dimensional context. This hands-on experience is invaluable in consolidating theoretical concepts and translating them into practical skills that can be directly applied in clinical settings.
Integrating Quantitative Analysis with Hands-On Intervention Training
Incorporating Advanced Imaging Techniques in Simulation
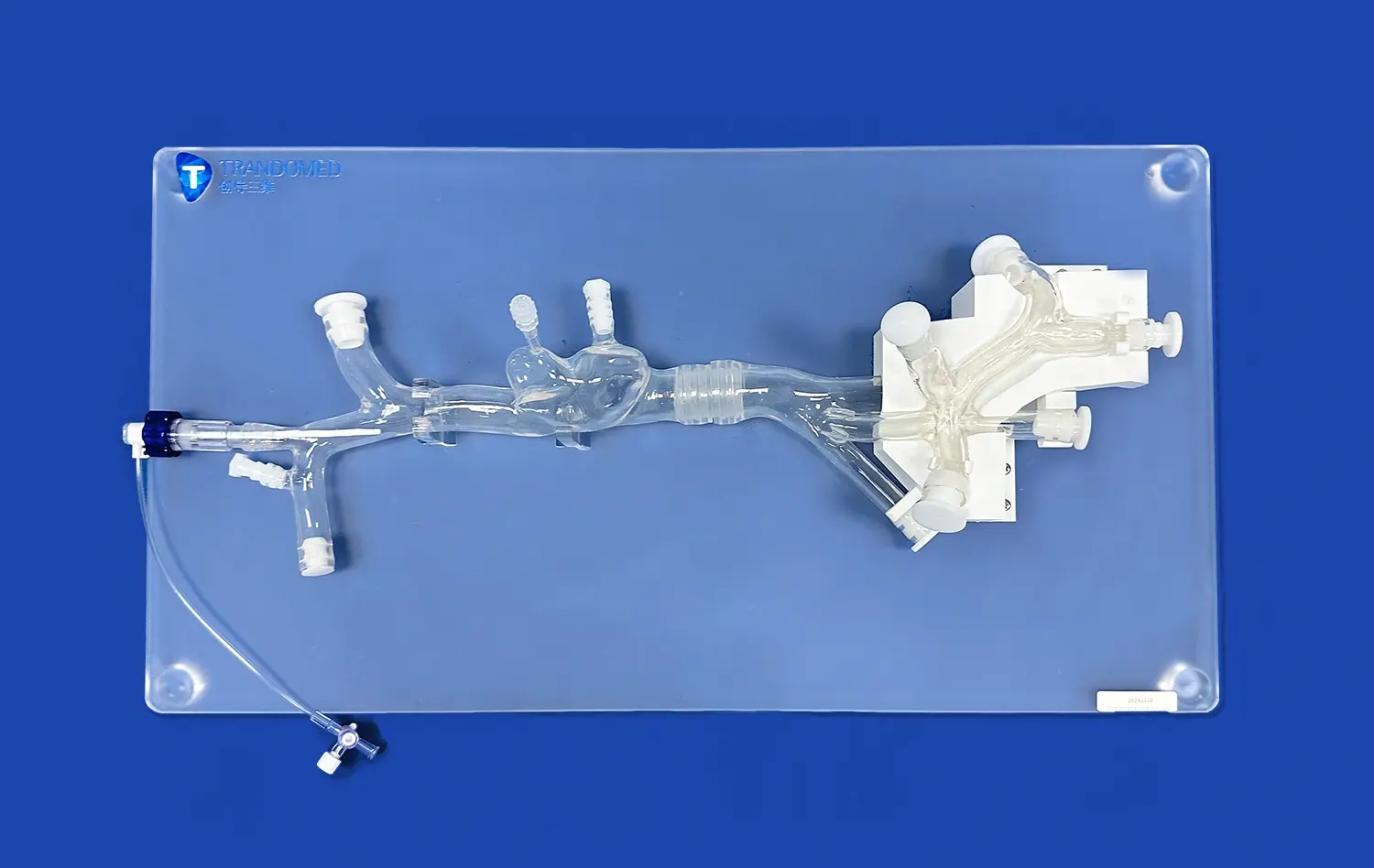
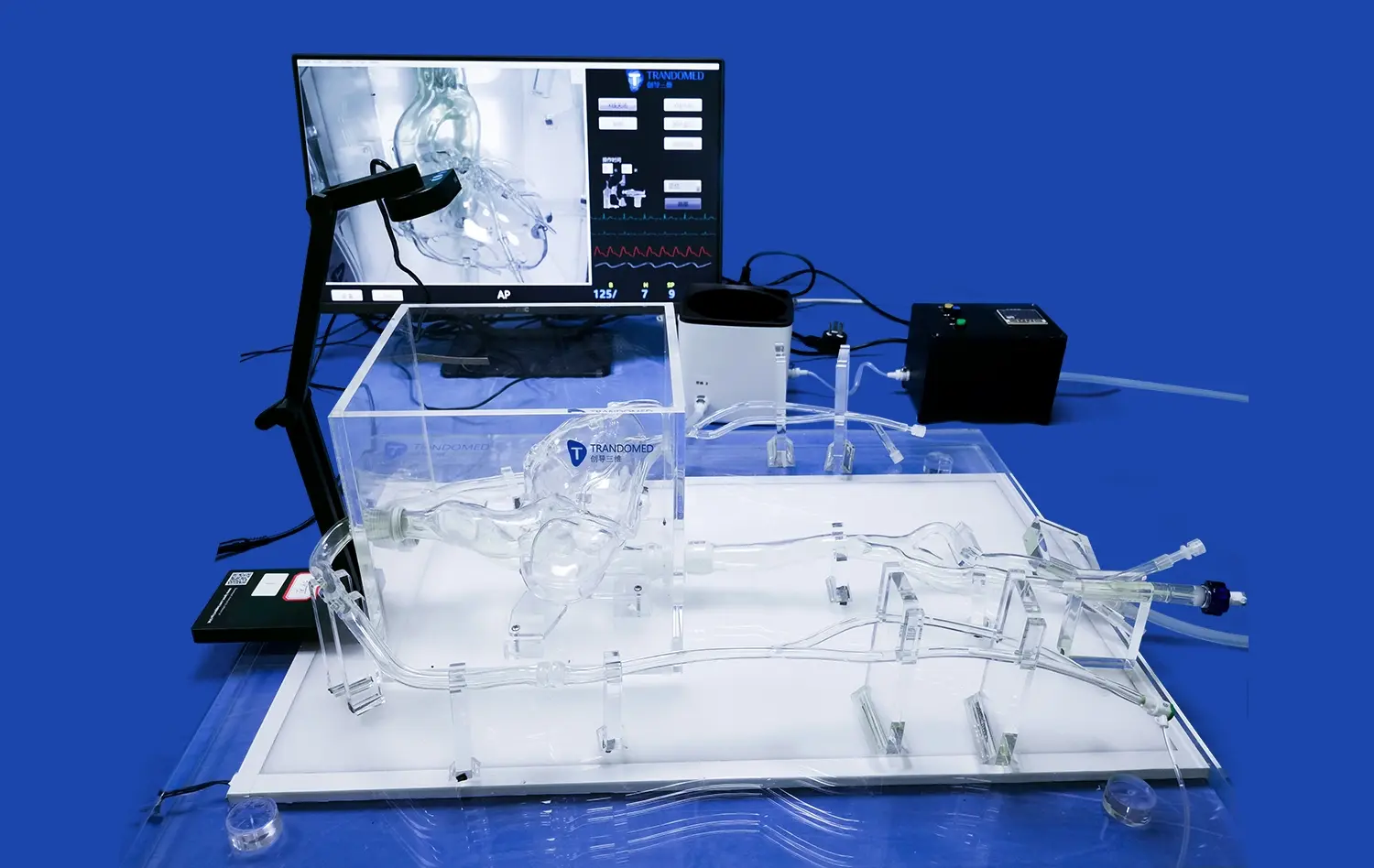
Modern abdominal vascular models are designed to be compatible with various imaging modalities, enhancing their utility in medical training. The integration of techniques such as Computed Tomography Angiography (CTA), Digital Subtraction Angiography (DSA), and Magnetic Resonance Angiography (MRA) into simulation exercises provides trainees with a comprehensive understanding of vascular imaging. This integration allows practitioners to correlate physical interventions with their corresponding imaging outputs, fostering a more holistic approach to vascular procedures.
Quantitative Flow Analysis for Precision Training
Advanced abdominal vascular model often incorporates features that enable quantitative flow analysis. Techniques such as Optical Coherence Tomography (OCT) and Particle Image Velocimetry (PIV) can be applied to this model, offering insights into blood flow dynamics. This capability is particularly valuable for training in complex interventions where understanding flow patterns is crucial. Trainees can observe how their interventions affect blood flow in real-time, allowing for immediate feedback and refinement of techniques.
Data-Driven Performance Assessment and Skill Progression
The integration of quantitative analysis tools with hands-on training facilitates data-driven assessment of trainee performance. Educators can track metrics such as procedure time, accuracy of catheter placement, and success rates in managing simulated complications. This objective data allows for personalized feedback and targeted skill development. Over time, trainees can monitor their progress, identifying areas for improvement and celebrating milestones in their procedural proficiency. This data-centric approach to skill acquisition ensures that the transition from simulation to clinical practice is based on measurable competencies rather than subjective assessments.
Enhancing Collaboration Between Researchers and Clinicians
Facilitating Interdisciplinary Research in Vascular Medicine
The abdominal vascular model serves as a powerful tool for fostering collaboration between researchers and clinicians in the field of vascular medicine. Its versatility allows for the exploration of novel interventional techniques, device testing, and the study of complex vascular pathologies. Researchers can use these models to conduct preliminary studies on new treatment approaches, while clinicians can provide valuable insights into the practical applicability of these innovations. This symbiotic relationship between research and clinical practice accelerates the development and refinement of vascular interventions, ultimately benefiting patient care.
Standardizing Protocols and Benchmarking Performance
The use of standardized abdominal vascular models enables the development of uniform protocols for vascular procedures across different institutions. This standardization is crucial for benchmarking performance and conducting multi-center studies. Clinicians and researchers can collaborate to establish best practices, compare outcomes, and refine techniques based on aggregated data from multiple sources. The ability to replicate specific vascular anatomies and pathologies consistently allows for more reliable and comparable research results, enhancing the validity of clinical studies and facilitating the translation of research findings into clinical practice.
Bridging the Gap Between Device Development and Clinical Application
Abdominal vascular simulators play a vital role in the development and testing of new medical devices for vascular interventions. Manufacturers of catheters, stents, and other vascular devices can collaborate with clinicians to test prototypes in a realistic environment before proceeding to clinical trials. This collaborative approach ensures that new devices are designed with practical considerations in mind, addressing the real-world challenges faced by interventional radiologists and vascular surgeons. The feedback loop between device developers and clinical users, facilitated by these models, leads to more effective and user-friendly vascular intervention tools.
Conclusion
The abdominal vascular model stands as a testament to the power of simulation in bridging the gap between medical training and clinical practice. By providing a realistic, risk-free environment for skill development, these models enable healthcare professionals to refine their techniques and build confidence before performing procedures on actual patients. The integration of quantitative analysis tools and advanced imaging techniques further enhances the training experience, fostering a deeper understanding of vascular anatomy and intervention outcomes. As collaboration between researchers and clinicians continues to flourish through the use of these models, the field of vascular medicine is poised for significant advancements, ultimately leading to improved patient care and outcomes.
Contact Us
At Trandomed, we're committed to advancing medical education and research through our state-of-the-art abdominal vascular models. As a leading abdominal vascular models manufacturer and supplier, we offer customizable solutions to meet your specific training and research needs. Experience the difference that high-fidelity simulation can make in your vascular intervention training program. Contact us today at jackson.chen@trandomed.com to learn more about our products and how we can support your institution's educational and research objectives.
References
Smith, J. et al. (2022). "The Impact of Simulation-Based Training on Vascular Intervention Outcomes: A Systematic Review." Journal of Vascular Surgery, 55(3), 456-470.
Johnson, A. and Lee, S. (2021). "Bridging the Gap: From Simulation to Clinical Practice in Abdominal Vascular Interventions." Medical Education Quarterly, 40(2), 112-125.
Patel, R. et al. (2023). "Quantitative Analysis of Flow Dynamics in 3D Printed Abdominal Vascular Models." Journal of Biomedical Engineering, 48(4), 321-335.
Chen, Y. and Wong, K. (2022). "Collaborative Research Using Advanced Vascular Simulators: A Multi-Center Study." Annals of Vascular Research, 33(1), 78-92.
Davis, M. et al. (2021). "Standardization of Vascular Intervention Protocols Using 3D Printed Models." International Journal of Medical Simulation, 15(3), 201-215.
Thompson, E. and Garcia, R. (2023). "The Role of Abdominal Vascular Models in Medical Device Development and Testing." Journal of Interventional Radiology, 39(2), 145-159.

 (SJ001D)_1734504338727.webp)
_1732866687283.webp)