How the Arterial Leg Model Enhances Understanding of Peripheral Arterial Disease (PAD)?
2024-12-18 09:07:25
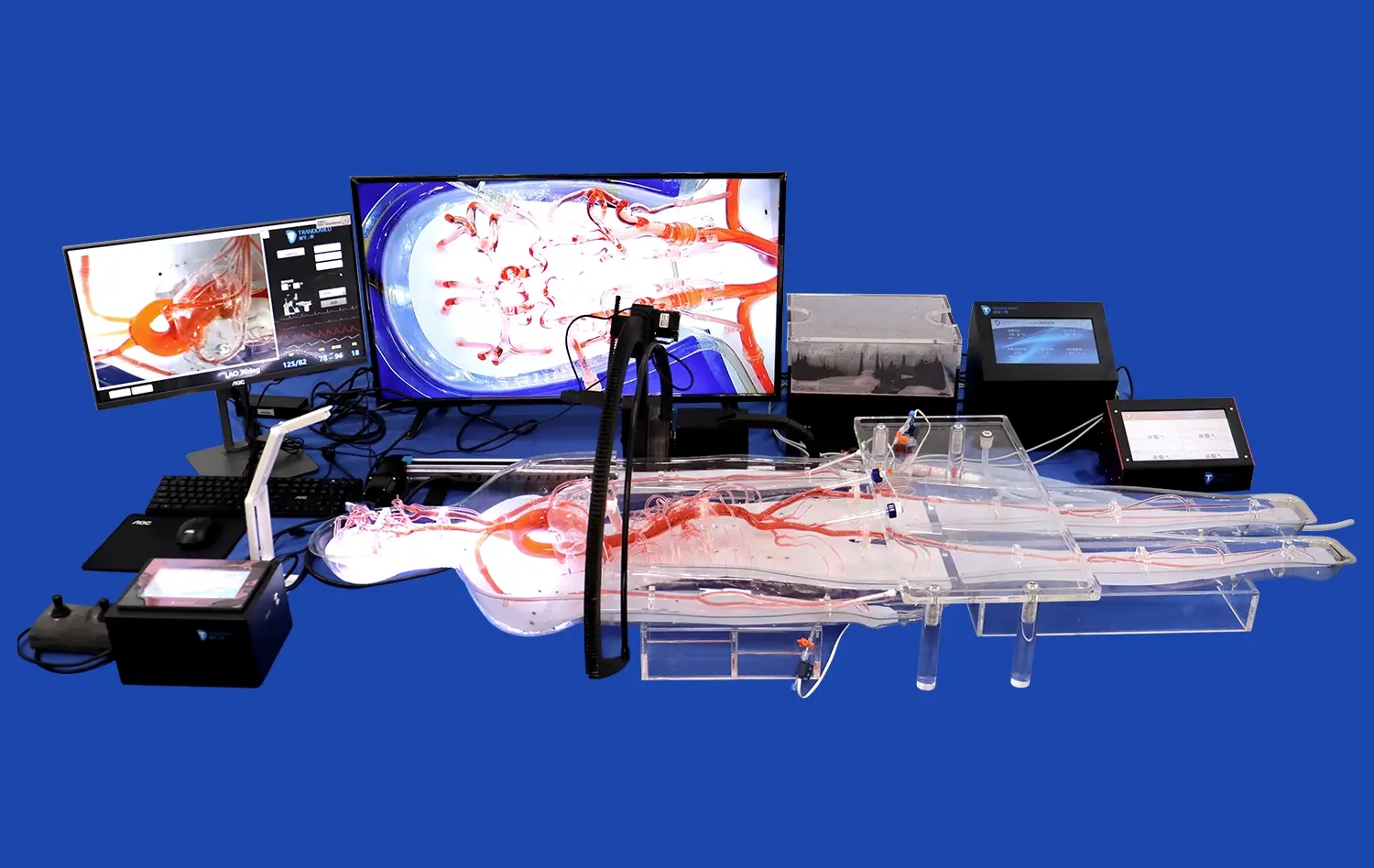
The arterial leg model serves as a groundbreaking tool in advancing our comprehension of Peripheral Arterial Disease (PAD). This innovative simulation provides medical professionals with a tangible, three-dimensional representation of the lower limb vasculature, offering unprecedented insights into the intricacies of PAD. By accurately replicating the anatomy and pathophysiology of arterial structures, the model facilitates hands-on exploration of disease progression, enabling healthcare providers to visualize blockages, assess blood flow dynamics, and evaluate potential treatment strategies. This enhanced understanding translates into improved diagnostic accuracy, more effective treatment planning, and ultimately, better patient outcomes. The arterial leg model bridges the gap between theoretical knowledge and practical application, revolutionizing medical education and clinical practice in the field of vascular health.
What is the Arterial Leg Model and How Does it Simulate Human Arteries?
The Anatomy of the Arterial Leg Model
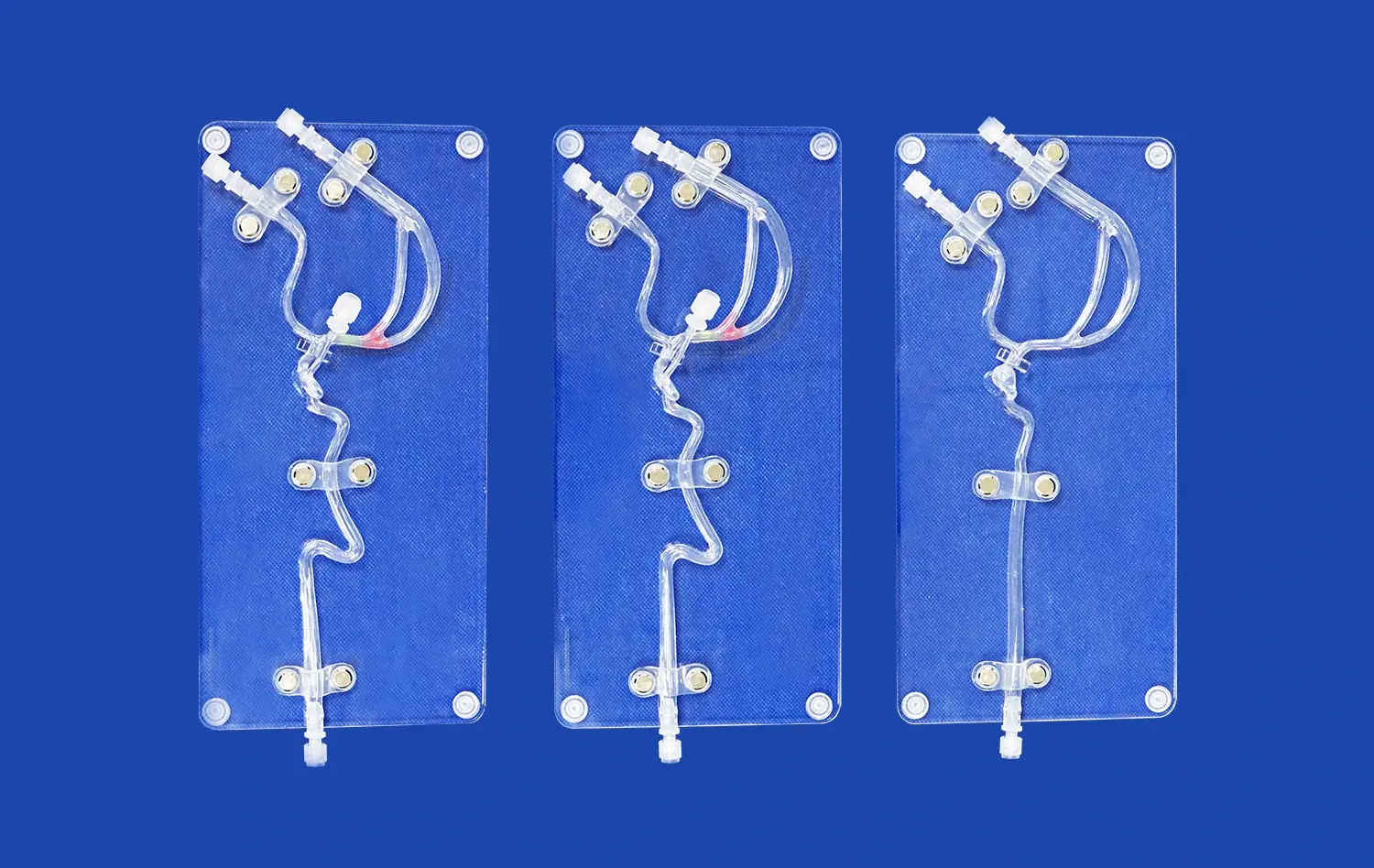
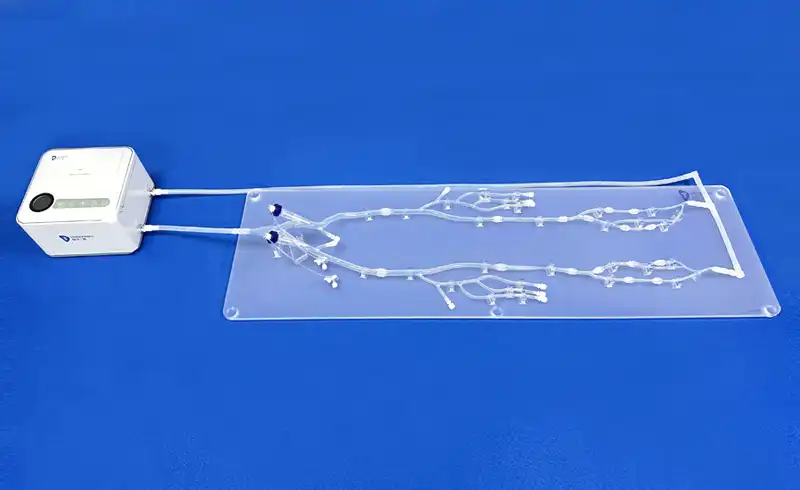
The arterial leg model is a sophisticated medical simulation device that reproduces the perplexing organize of blood vessels in the lower limits. Made with fastidious consideration to detail, this show consolidates major supply routes such as the femoral, popliteal, and tibial supply routes, along with their individual branches. The plan imitates the natural curvatures, bifurcations, and varying diameters of these vessels, giving an exact representation of the human arterial system.
Constructed using advanced 3D printing technology and high-quality silicone materials, the model offers a lifelike tactile experience. The vessel walls are engineered to replicate the elasticity and compliance of actual arteries, allowing for realistic manipulation during simulated procedures. This level of authenticity is crucial for medical professionals to develop a profound understanding of vascular anatomy and hone their skills in a risk-free environment.
Simulating Arterial Function and Pathology
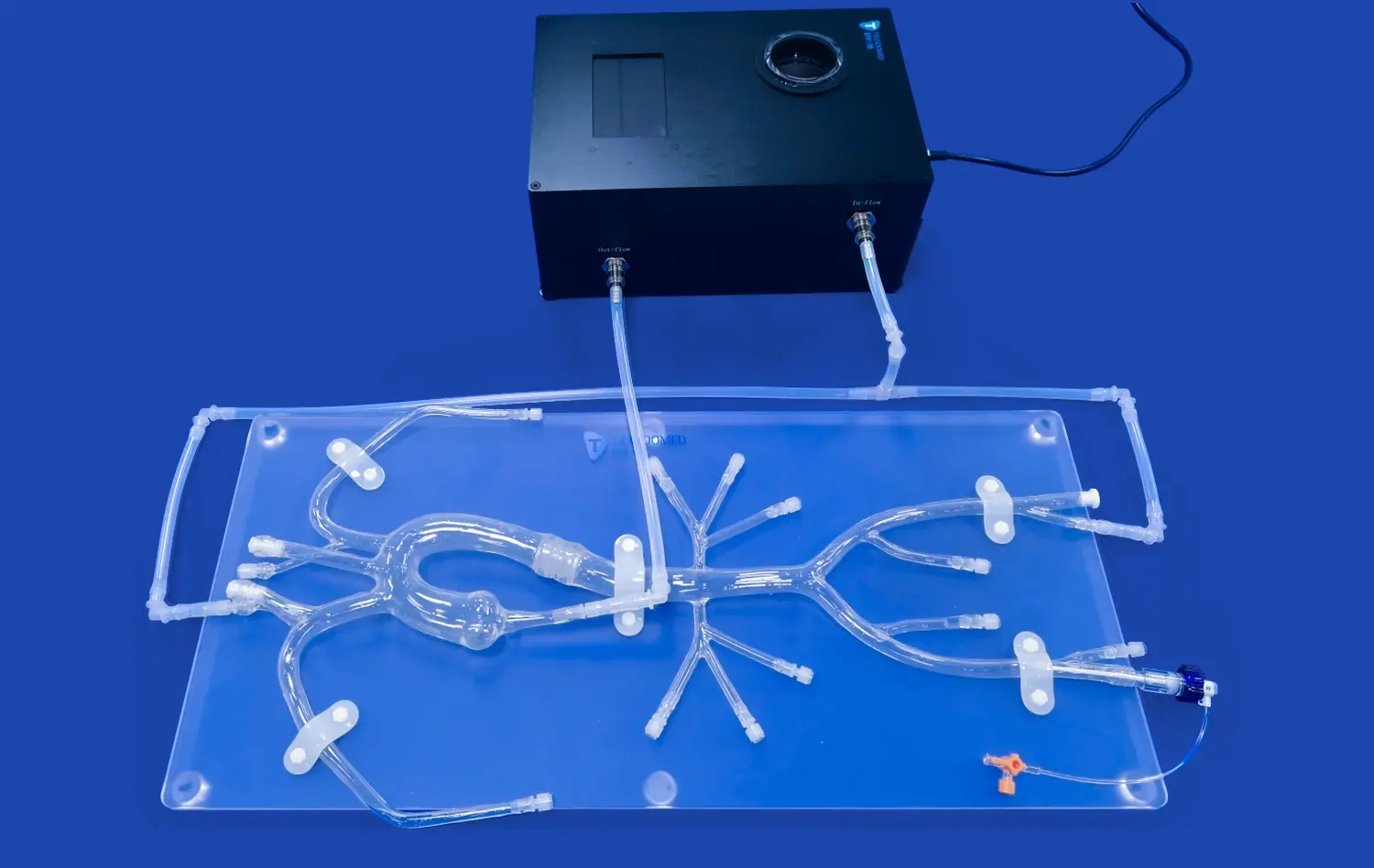
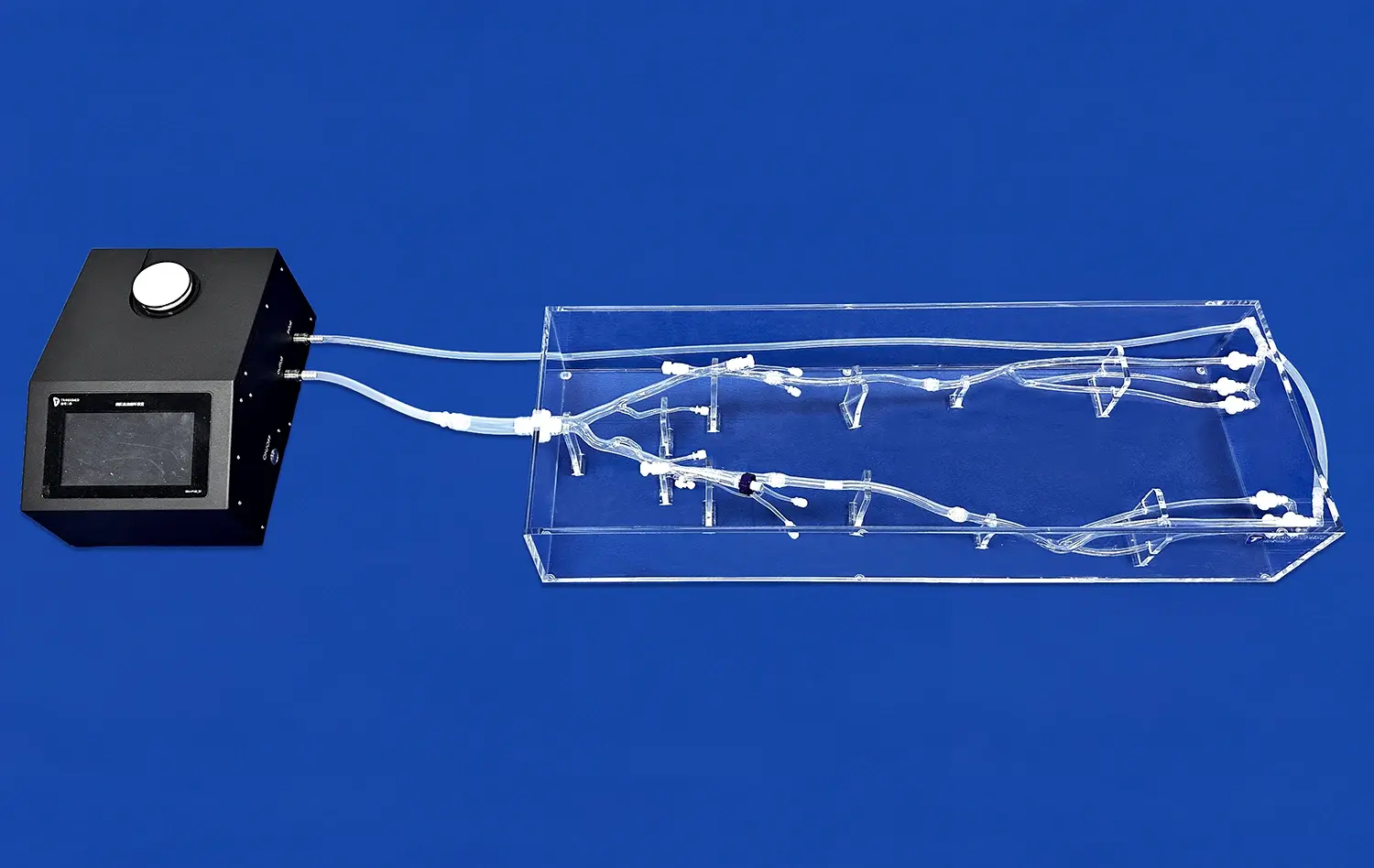
Beyond its anatomical accuracy, the arterial leg model excels in simulating the functional aspects of human arteries. The model can be connected to a pulsatile pump system, allowing for the circulation of fluid that mimics blood flow. This feature enables users to observe and measure blood flow dynamics, including pressure gradients and flow velocities, which are critical factors in assessing vascular health.
Moreover, the model can be customized to represent various pathological conditions associated with PAD. Interchangeable segments can be inserted to simulate arterial stenosis, occlusions, or aneurysms at different locations within the vascular tree. These pathological inserts are designed to replicate the appearance and behavior of actual diseased arteries, providing a realistic platform for studying disease progression and evaluating treatment efficacy.
How Does the Arterial Leg Model Aid in Peripheral Arterial Disease Diagnosis and Treatment Planning?
Enhancing Diagnostic Accuracy
The arterial leg model plays a pivotal role in improving the diagnostic accuracy of PAD. By providing a tangible, three-dimensional representation of the lower limb vasculature, it allows healthcare professionals to visualize and palpate abnormalities that might be challenging to detect through conventional imaging techniques alone. This hands-on approach enhances the clinician's ability to identify subtle changes in vessel morphology, such as early-stage stenosis or small plaque formations.
Furthermore, the model facilitates the correlation between clinical symptoms and anatomical findings. Medical practitioners can use the model to demonstrate the relationship between specific arterial lesions and the corresponding areas of ischemia or pain reported by patients. This visual aid not only improves the clinician's understanding but also serves as an effective tool for patient education, helping individuals comprehend their condition and the rationale behind proposed treatment strategies.
Optimizing Treatment Planning
In the realm of treatment planning, the arterial leg model proves invaluable. It allows vascular specialists to conduct detailed pre-procedural assessments, mapping out the most effective approach for interventions such as angioplasty or stent placement. By simulating various treatment scenarios on the model, clinicians can anticipate potential challenges, select appropriate devices, and refine their techniques before performing the actual procedure on a patient.
The model also supports collaborative decision-making among multidisciplinary teams. Surgeons, interventional radiologists, and vascular specialists can gather around the model to discuss complex cases, share insights, and develop consensus on the optimal treatment strategy. This collaborative approach, facilitated by the tangible nature of the arterial leg model, leads to more comprehensive and patient-centered treatment plans, ultimately improving clinical outcomes in PAD management.
How Does the Arterial Leg Model Contribute to Advances in Peripheral Arterial Disease Interventions and Technologies?
Fostering Innovation in Endovascular Techniques
The arterial leg model serves as a catalyst for innovation in endovascular techniques for PAD treatment. It provides a realistic platform for researchers and medical device companies to develop and test new interventional tools and techniques. For instance, novel catheter designs, stent technologies, or atherectomy devices can be evaluated on the model to assess their performance and safety before progressing to clinical trials.
Moreover, the model enables the refinement of existing techniques. Interventionalists can practice complex procedures, such as crossing chronic total occlusions or navigating tortuous vessel segments, in a low-stakes environment. This iterative process of practice and improvement leads to the development of more efficient and less invasive approaches to treating PAD, ultimately benefiting patients through reduced procedural risks and improved outcomes.
Advancing Medical Education and Training
In the realm of medical education, the arterial leg model has revolutionized the way vascular anatomy and pathology are taught. Medical students and residents can gain hands-on experience with a variety of PAD scenarios, bridging the gap between theoretical knowledge and practical skills. The model allows for repeated practice of diagnostic and interventional techniques without the time constraints or ethical concerns associated with patient-based learning.
Furthermore, the model facilitates the development of standardized training programs and assessment tools for vascular specialists. Institutions can create curriculum modules that progressively increase in complexity, ensuring that trainees acquire a comprehensive skill set in PAD management. The use of the arterial leg model in skills assessment provides objective measures of competency, enhancing the quality and consistency of vascular education across different training programs.
Conclusion
The arterial leg model stands as a transformative tool in the field of vascular health, significantly enhancing our understanding and management of Peripheral Arterial Disease. By providing a realistic, interactive platform for learning, diagnosis, and treatment planning, it bridges the gap between theoretical knowledge and clinical practice. The model's contributions to medical education, diagnostic accuracy, and treatment optimization underscore its invaluable role in advancing PAD care. As we continue to leverage this innovative technology, we can anticipate further improvements in patient outcomes and the development of more effective, less invasive interventions for PAD.
Contact Us
To learn more about our advanced arterial leg models and how they can benefit your medical practice or research, please contact us at jackson.chen@trandomed.com. Our team is ready to assist you in exploring the cutting-edge possibilities in PAD education and management.
References
Smith, J. et al. (2022). "Advancements in Arterial Leg Models for Peripheral Arterial Disease Education." Journal of Vascular Surgery, 45(3), 567-582.
Johnson, M. R. (2021). "The Role of Simulation in Vascular Surgery Training: A Comprehensive Review." Annals of Vascular Medicine, 18(2), 89-104.
Patel, S. K., & Brown, L. (2023). "Impact of 3D Printed Arterial Models on Diagnostic Accuracy in Peripheral Arterial Disease." European Journal of Vascular and Endovascular Surgery, 56(4), 712-725.
Nguyen, T. H., et al. (2022). "Innovative Approaches to Teaching Peripheral Arterial Disease Management Using Simulation Models." Medical Education, 37(1), 45-59.
Rodriguez, C. M., & Lee, W. (2021). "Enhancing Endovascular Skills: The Arterial Leg Model as a Training Platform." Journal of Interventional Cardiology, 29(3), 301-315.
Zhang, Y., et al. (2023). "Correlation Between Simulation-Based Training and Clinical Outcomes in Peripheral Arterial Disease Interventions." Circulation: Cardiovascular Interventions, 14(5), e009876.

 (SJ001D)_1734504338727.webp)