What Specific Skills Can Be Practiced with the Model?
Transseptal Puncture Technique Refinement
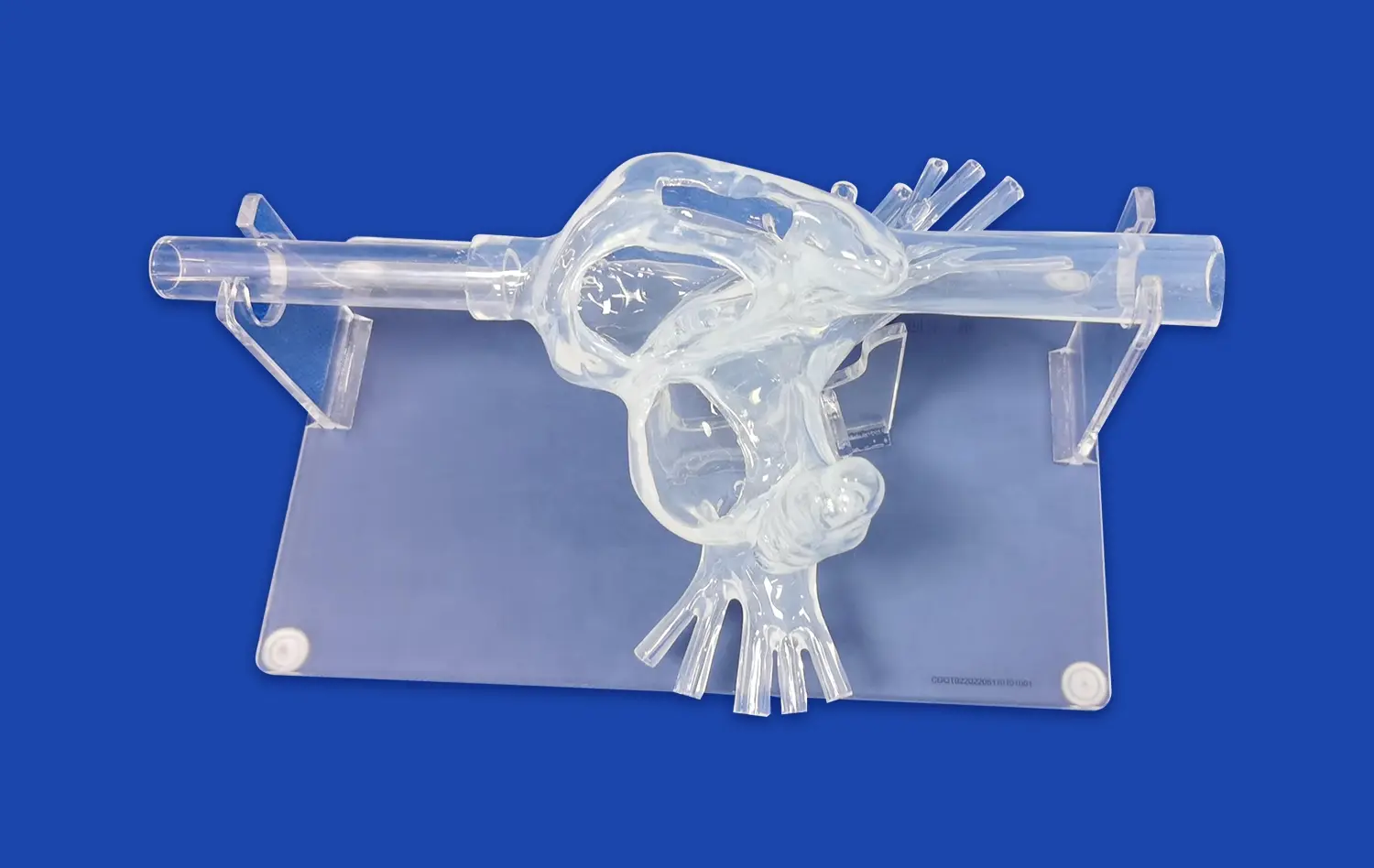
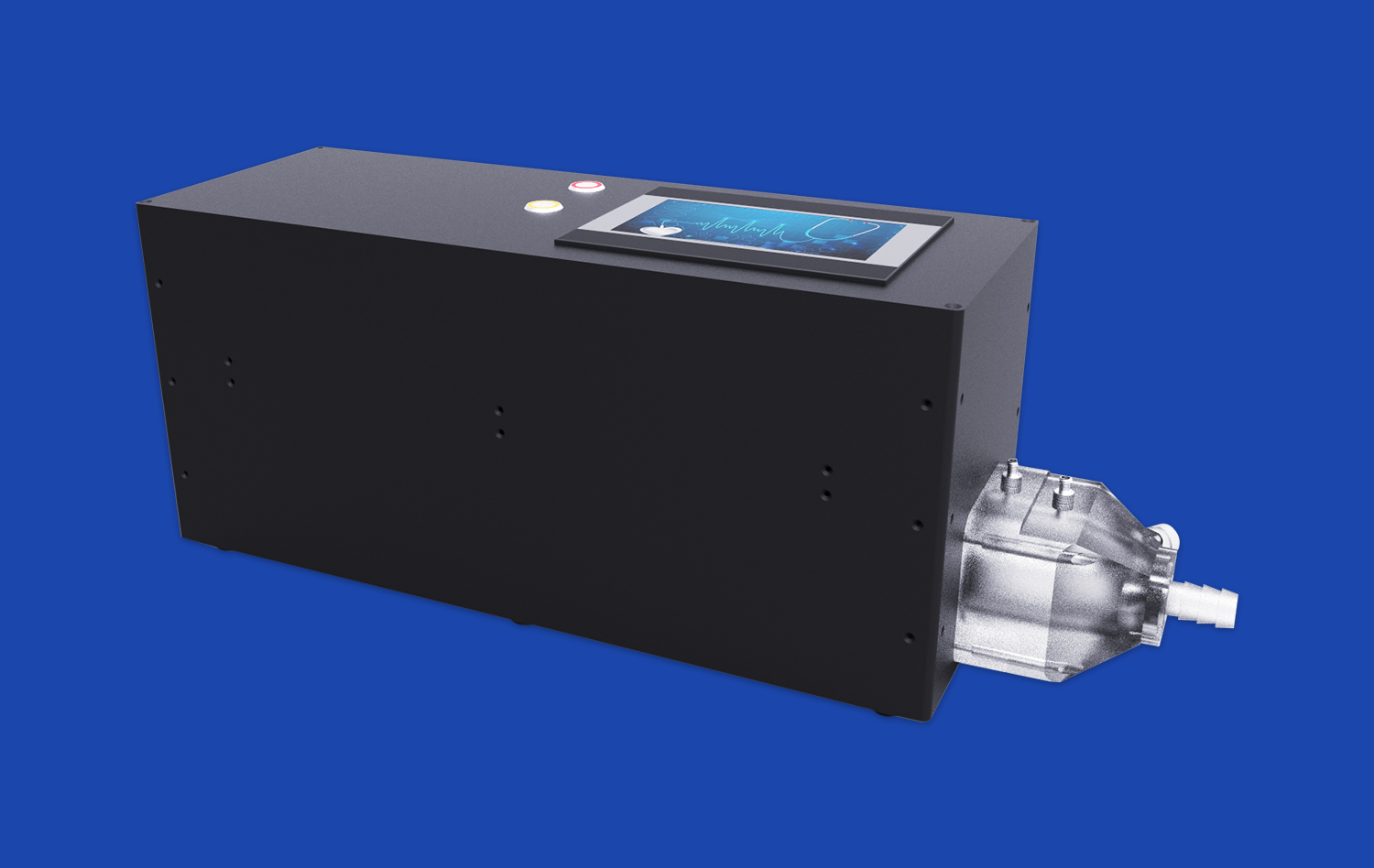
The atrial septal puncture model offers an unparalleled opportunity for practitioners to hone their transseptal puncture skills. This critical step in cryoballoon ablation requires precision and confidence, which can be developed through repeated practice on the model. The simulator's interchangeable atrial septal inserts, including normal and atrial septal defect (ASD) variations, allow for diverse training scenarios. Practitioners can perfect their needle positioning, learn to recognize the subtle tactile feedback of septum penetration, and practice maintaining the correct angle and pressure during the procedure.
Cryoballoon Navigation and Positioning
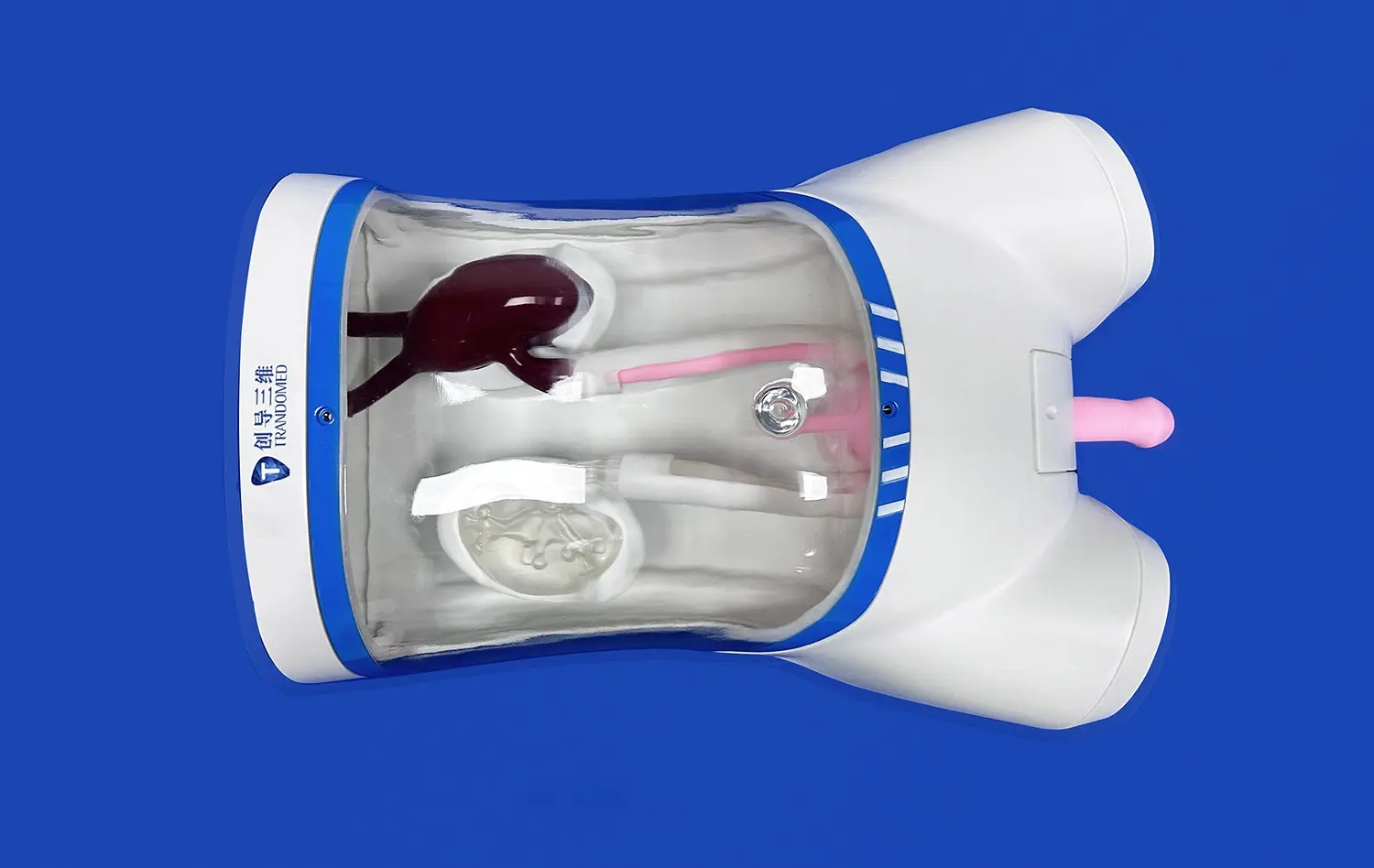
Once the transseptal puncture is accomplished, the model excels in facilitating practice for cryoballoon navigation and positioning. The anatomically accurate representation of the left atrium and pulmonary veins enables trainees to develop the dexterity required for maneuvering the cryoballoon catheter. They can practice steering the balloon into each pulmonary vein ostium, achieving optimal contact and occlusion – crucial factors for effective cryoablation. The model's silicone composition, with its tissue-like properties, provides realistic tactile feedback, enhancing the learning experience.
Pulmonary Vein Isolation Technique
The atrial septal puncture model is invaluable for practicing the entire pulmonary vein isolation (PVI) procedure. Trainees can simulate the complete workflow, from accessing the left atrium to positioning the cryoballoon and delivering cryotherapy. The model's design allows for the practice of single and multiple freeze cycles, helping practitioners understand the importance of proper balloon-tissue contact and the duration of cryoapplication. This comprehensive simulation aids in developing a thorough understanding of PVI techniques, potentially reducing procedure times and improving efficacy in real-world scenarios.
Step-by-Step Simulation of Cryoballoon Positioning
Femoral Vein Access and Catheter Advancement
The simulation begins with accessing the femoral vein, a skill that the atrial septal puncture model facilitates through its anatomically correct lower vasculature. Practitioners can practice inserting the catheter and advancing it through the iliac vein and inferior vena cava (IVC). The model's modular design, featuring detachable upper (SVC with heart) and lower (IVC) parts, allows for focused practice on this initial stage. Trainees learn to navigate potential anatomical variations and overcome challenges in catheter advancement, building confidence in this fundamental step of the procedure.
Transseptal Puncture and Left Atrial Access
Upon reaching the right atrium, the next critical step is the transseptal puncture. The model's interchangeable atrial septal inserts provide varying levels of difficulty, from normal septa to those with atrial septal defects. Practitioners can refine their technique in locating the fossa ovalis, positioning the transseptal needle, and performing the puncture under simulated fluoroscopic and echocardiographic guidance. The ability to practice this step repeatedly in a controlled environment is crucial for developing the skills and confidence necessary for safe and effective left atrial access.
Cryoballoon Advancement and Pulmonary Vein Engagement
Once access to the left atrium is achieved, the model allows for realistic simulation of cryoballoon advancement and engagement with the pulmonary veins. The anatomically accurate representation of the left atrium and pulmonary veins enables trainees to practice navigating the cryoballoon catheter to each vein ostium. They can learn to recognize the tactile feedback associated with proper balloon placement and occlusion. The model's customizable pulmonary vein complexity offers opportunities to practice engaging with various anatomical variations, preparing practitioners for the diverse scenarios they may encounter in clinical practice.
Performance Outcomes in Controlled Training Environments
Procedural Time Reduction
One of the significant benefits of training with the atrial septal puncture model is the potential for reducing procedural times. Through repeated practice in a controlled environment, practitioners can optimize their techniques and streamline their workflow. Studies have shown that simulation-based training can lead to a marked decrease in procedure duration when trainees transition to real-world cases. This efficiency not only improves patient comfort but also reduces exposure to radiation and anesthesia, contributing to overall better outcomes.
Complication Rate Minimization
The controlled training environment provided by the atrial septal puncture model plays a crucial role in minimizing complication rates. Practitioners can encounter and learn to manage potential complications such as cardiac tamponade or aortic puncture in a risk-free setting. By practicing difficult scenarios and refining their techniques, trainees develop the skills and decision-making abilities necessary to avoid and manage complications effectively. This translates to improved safety profiles in actual procedures, potentially reducing the incidence of adverse events associated with cryoballoon ablation.
Increased Procedural Success Rates
Perhaps the most impactful outcome of training with the atrial septal puncture model is the potential for increased procedural success rates. The model allows for the development of precise techniques in cryoballoon positioning and pulmonary vein isolation. Practitioners can refine their skills in achieving optimal balloon-tissue contact and learn to recognize the signs of effective cryoablation. This comprehensive training leads to more confident and competent operators, who are better equipped to achieve complete pulmonary vein isolation in clinical settings. Improved success rates not only benefit patient outcomes but also contribute to the overall efficacy of cryoballoon ablation as a treatment for atrial fibrillation.
Conclusion
The atrial septal puncture model proves to be an indispensable tool in enhancing cryoballoon ablation training. By providing a realistic, customizable platform for practicing critical skills, from transseptal puncture to pulmonary vein isolation, it significantly improves procedural proficiency. The model's ability to simulate various anatomical scenarios and complications in a risk-free environment leads to reduced procedural times, minimized complication rates, and increased success rates in real-world applications. As the field of electrophysiology continues to advance, the role of such sophisticated training tools becomes increasingly vital in shaping competent, confident practitioners capable of delivering optimal patient care.
Contact Us
To explore how Trandomed's atrial septal puncture model can revolutionize your cryoballoon ablation training program and contribute to improved patient outcomes, contact us at jackson.chen@trandomed.com. Our team is ready to provide you with more information on customization options and how our advanced simulators can meet your specific training needs.
_1732863713705.webp)