Simulating Aneurysm Scenarios with Variable Sizes
Anatomical Accuracy and Pathological Replication
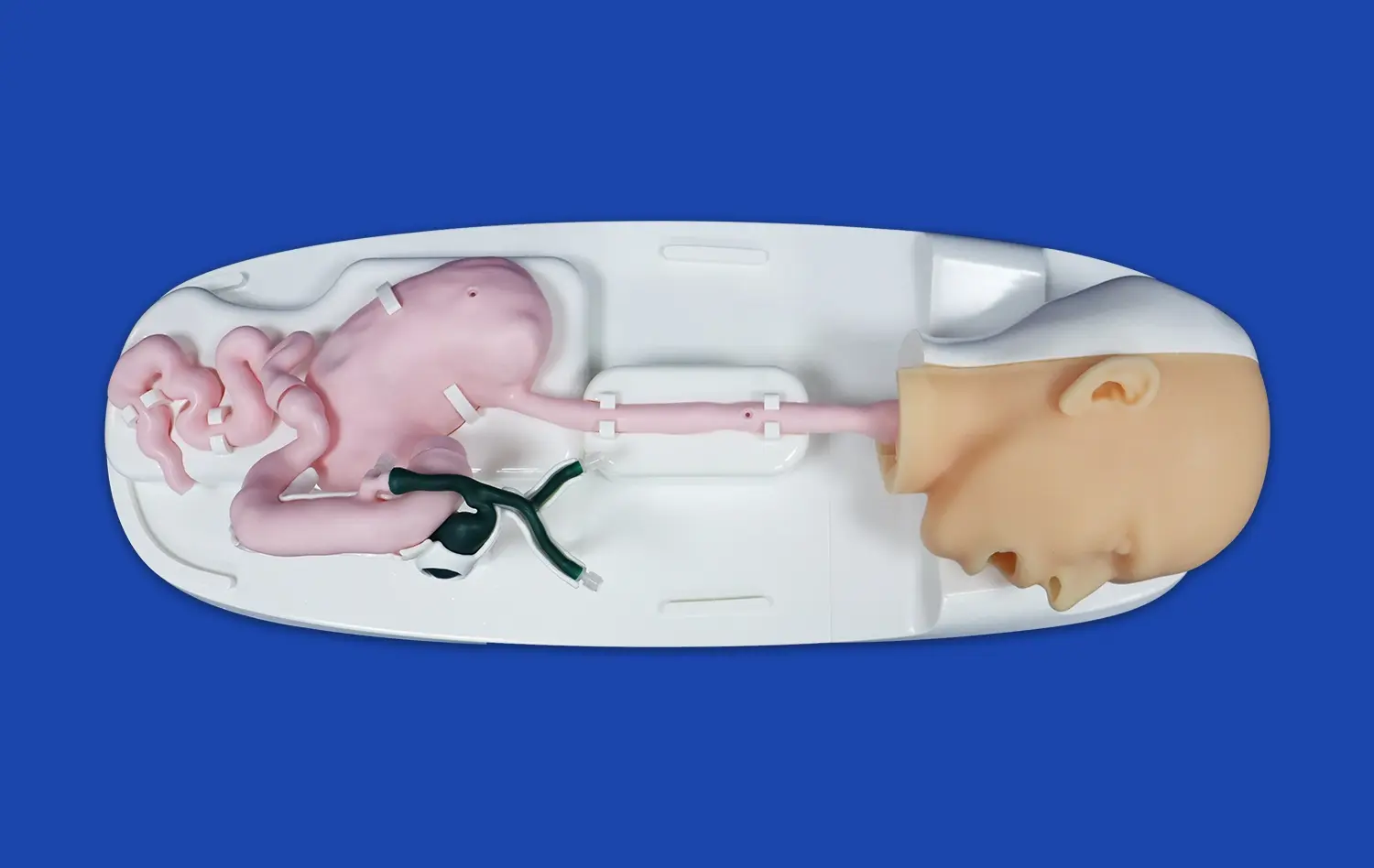
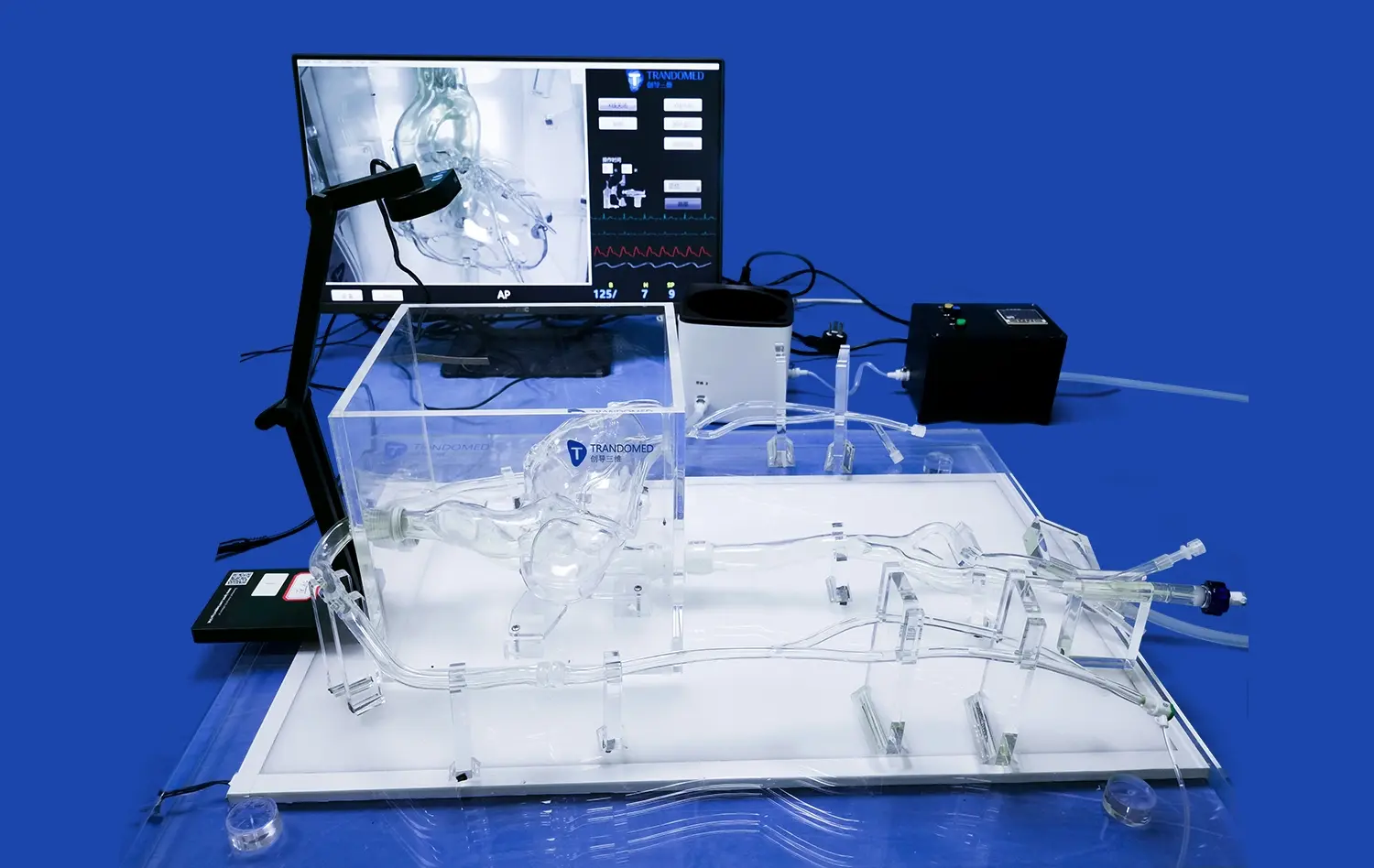
The Full Body Artery Model excels in its anatomical precision, crafted using real human CT and MRI data. This level of detail ensures that trainees encounter a highly realistic representation of the vascular system. The model's intracranial segment features three aneurysms of different sizes, mirroring the diversity of cases encountered in clinical practice. This variety allows healthcare professionals to familiarize themselves with the nuances of different aneurysm morphologies and locations, enhancing their diagnostic and treatment planning skills.
Customizable Pathological Features
One of the standout features of the full body artery model is its customizability. Trandomed's in-house manufacturing capabilities allow for the creation of bespoke models tailored to specific training needs. This flexibility enables educators to design scenarios that focus on particular challenges or rare conditions, ensuring that trainees are prepared for a wide spectrum of clinical situations. The ability to adjust dimensions and replicate specific pathological features makes this model an adaptable and invaluable tool in aneurysm tamponade training.
Integration of Stenotic Lesions
Beyond aneurysms, the model incorporates a stenotic lesion in the right brain, adding another layer of complexity to the training scenarios. This feature allows practitioners to simultaneously consider the implications of arterial narrowing in conjunction with aneurysm management. Such comprehensive representation of vascular pathologies enhances the model's utility in training for real-world clinical decision-making and procedural planning.
Hands-On Training for Advanced Endovascular Techniques
Realistic Tactile Feedback
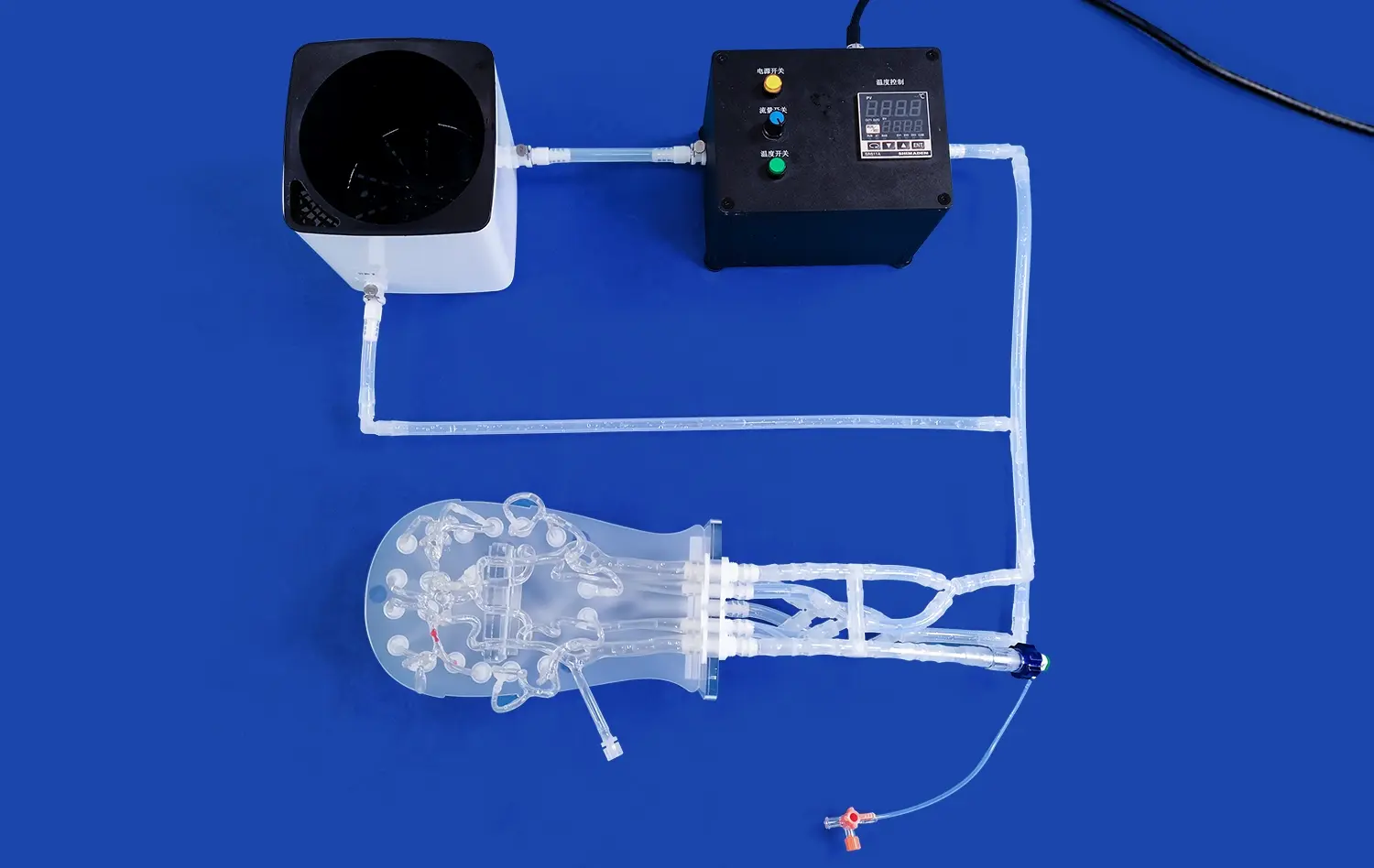
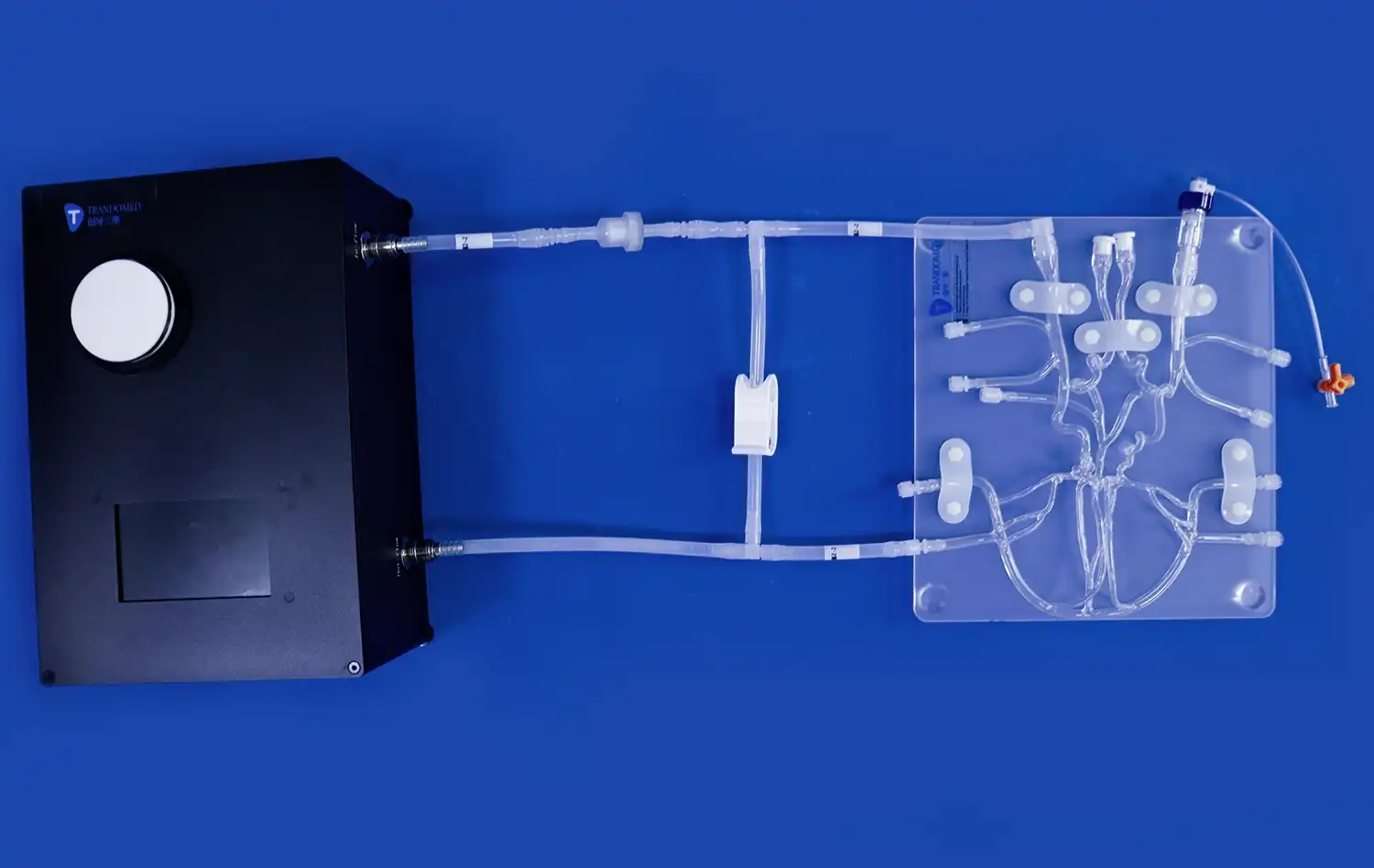
The Full Body Artery Model is constructed from high-quality silicone with a Shore hardness of 40A, closely mimicking the elasticity and texture of human blood vessels. This material property provides trainees with realistic tactile feedback during simulated procedures, allowing them to develop a feel for the delicate manipulations required in endovascular interventions. The authentic sensation of catheter navigation and device deployment significantly enhances the learning experience, bridging the gap between theoretical knowledge and practical application.
Comprehensive Procedural Simulation
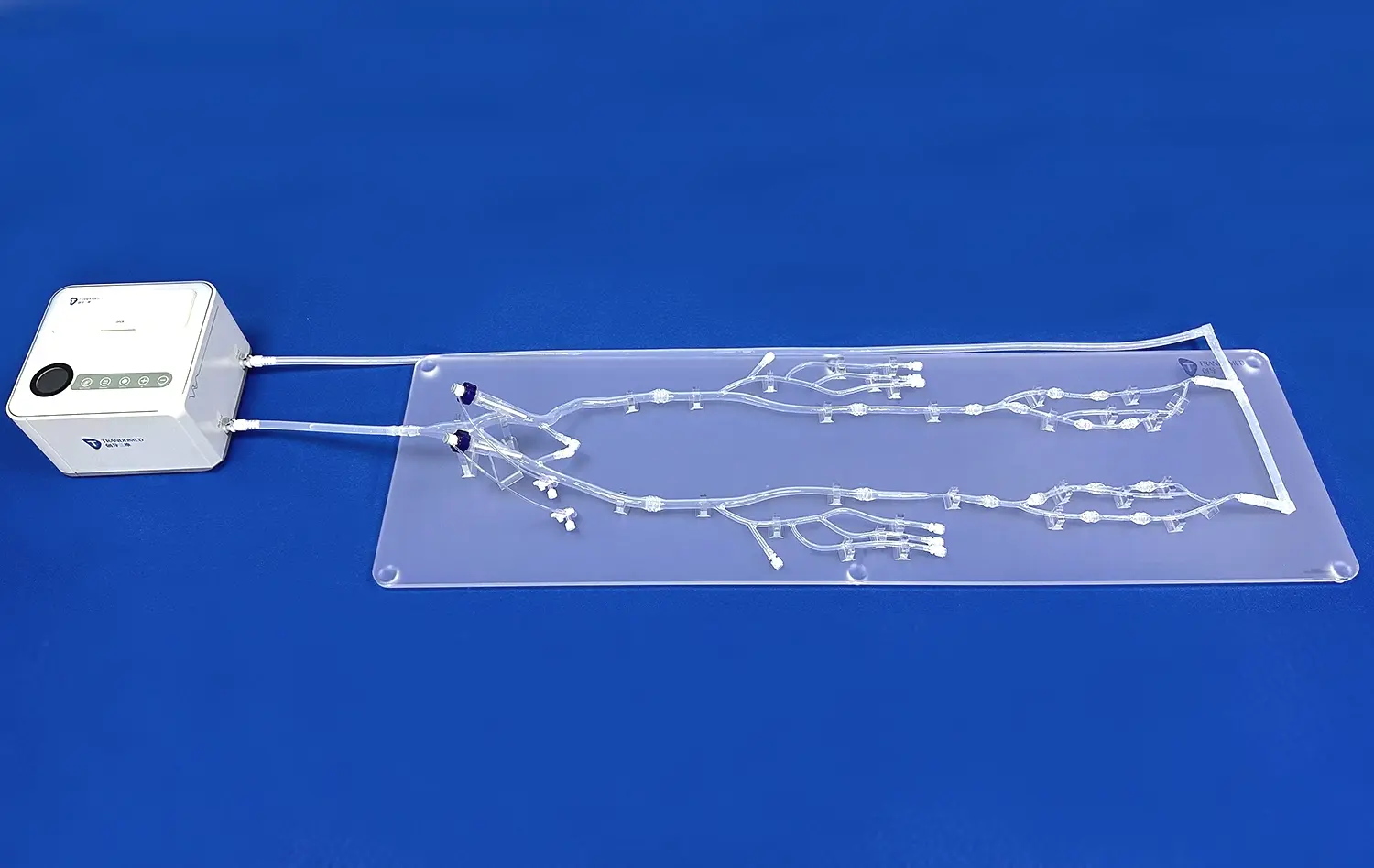
Extending from the femoral artery to the A2 segment of the anterior cerebral artery (ACA) and the M2 segment of the middle cerebral artery (MCA), the full body artery model offers a complete pathway for endovascular navigation. This extensive coverage allows trainees to practice the entire sequence of an aneurysm tamponade procedure, from femoral access to intracranial intervention. The ability to repeatedly perform these complex maneuvers in a risk-free environment accelerates skill acquisition and procedural familiarity.
Device Testing and Validation
Beyond its training applications, the Full Body Artery Model serves as an excellent platform for the development, testing, and validation of neuro-interventional devices. Manufacturers can utilize this model to assess the performance and compatibility of new endovascular tools under conditions that closely resemble clinical use. This capability not only aids in refining existing technologies but also fosters innovation in aneurysm treatment modalities.
Measuring Procedure Efficiency and Success Rates
Quantifiable Performance Metrics
The Full Body Artery Model facilitates the collection of objective data on procedural performance. Trainers can measure various parameters such as time to aneurysm access, accuracy of device placement, and overall procedure duration. These quantifiable metrics provide valuable insights into a trainee's progress and help identify areas for improvement. By establishing benchmarks and tracking performance over time, educational programs can ensure consistent skill development among their trainees.
Comparative Analysis of Techniques
Full body artery model's consistency and reproducibility make it an ideal tool for comparing different endovascular techniques or approaches to aneurysm tamponade. Researchers and educators can systematically evaluate the efficacy of various strategies, contributing to the refinement of best practices in aneurysm management. This comparative capability is particularly valuable in assessing novel techniques or devices against established methods, driving evidence-based advancements in the field.
Simulation of Complication Scenarios
To further enhance training realism, the Full Body Artery Model can be adapted to simulate potential complications during aneurysm tamponade procedures. By incorporating scenarios such as vessel rupture or thrombus formation, trainees can practice managing adverse events in a controlled environment. This exposure to complication management not only improves technical skills but also enhances critical thinking and decision-making abilities under pressure.
Conclusion
The full body artery model represents a significant leap forward in aneurysm tamponade training. Its anatomical accuracy, customizable features, and comprehensive simulation capabilities provide an unparalleled platform for skill development in endovascular techniques. By offering hands-on experience with realistic tactile feedback and diverse pathological scenarios, the model accelerates the learning curve for healthcare professionals. The ability to measure and analyze performance metrics further enhances its value as an educational tool. As medical education continues to evolve, the Full Body Artery Model stands as a testament to the power of advanced simulation in preparing the next generation of neuro-interventional specialists.
Contact Us
Trandomed, a leading manufacturer of 3D printed silicone medical simulators, is committed to advancing medical education through innovative products like the Full Body Artery Model. Our state-of-the-art factory and extensive experience in designing and producing medical simulation products ensure that you receive the highest quality training tools. As a trusted supplier and manufacturer in the field, we offer customization services to meet your specific training needs. Experience the difference that realistic, comprehensive simulation can make in your aneurysm tamponade training program. Contact us today at jackson.chen@trandomed.com to learn more about how our Full Body Artery Model can elevate your medical education and research capabilities.
_1732863962417.webp)