How Venous Cardiac Electrophysiology Models Enhance Catheter Ablation Outcomes?
2025-07-16 09:00:00
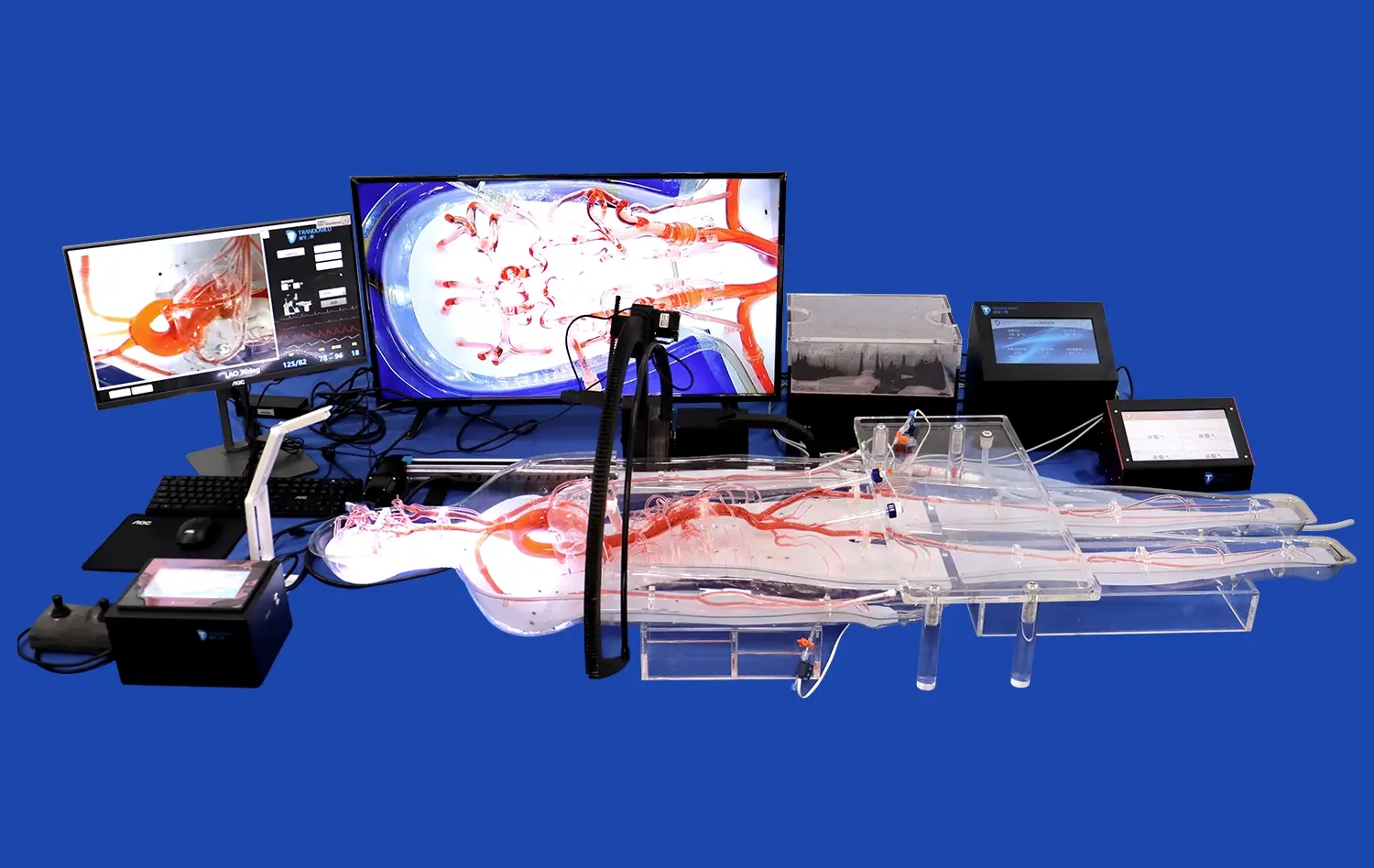
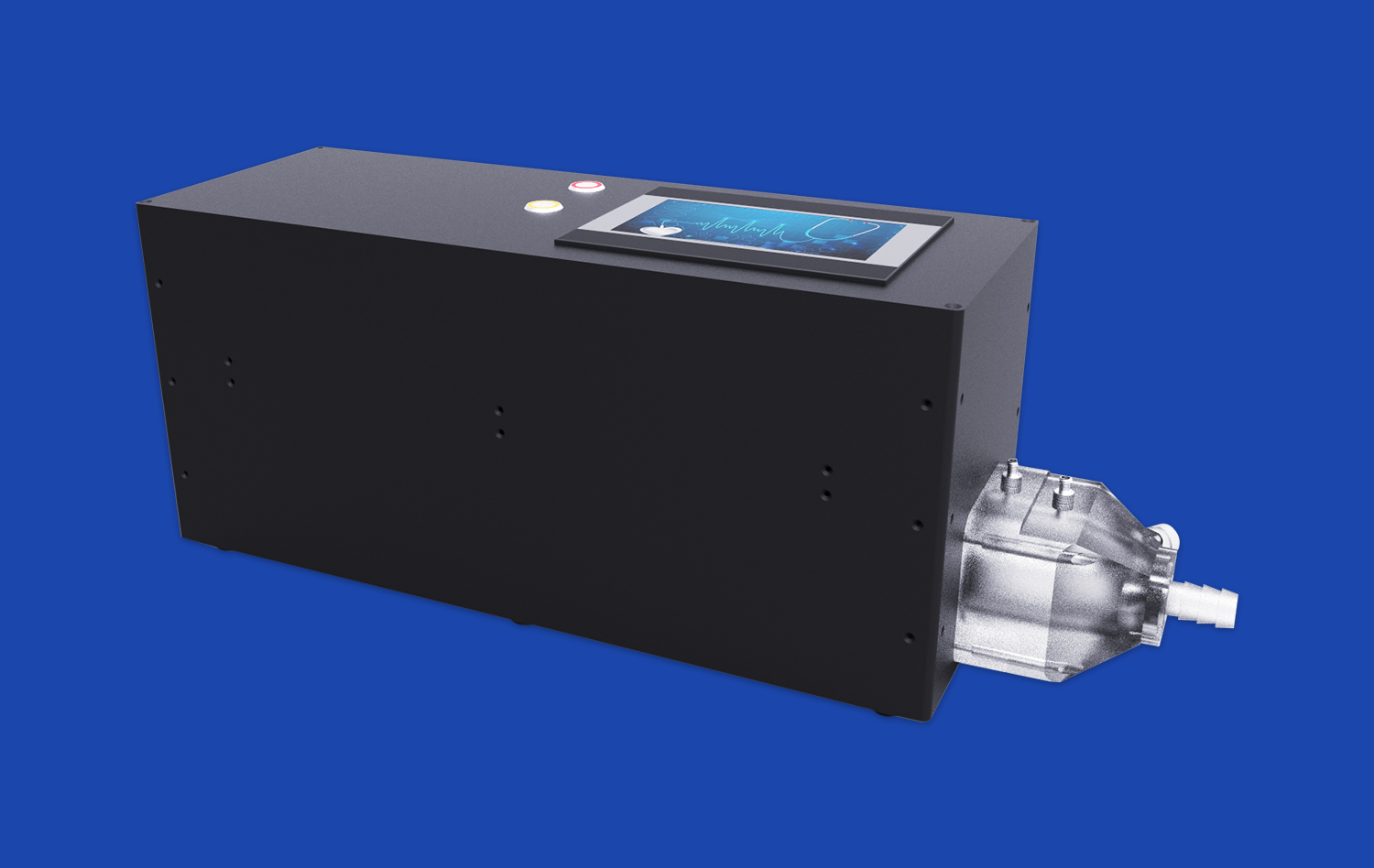
Venous cardiac electrophysiology models have revolutionized the field of catheter ablation, significantly improving procedural outcomes and patient care. These advanced 3D-printed simulators provide an unparalleled platform for understanding complex arrhythmias, refining ablation techniques, and enhancing procedural safety. By replicating patient-specific cardiac anatomy and electrophysiological characteristics, these models enable clinicians to practice and perfect their skills in a risk-free environment. The integration of these models into pre-procedural planning and intra-procedural guidance has led to more precise ablation strategies, reduced procedure times, and improved long-term success rates. Moreover, the ability to visualize and interact with accurate representations of individual patient anatomy has dramatically reduced the risk of complications and enhanced overall procedural efficacy.
Replicating Patient-Specific Arrhythmias in the Venous Cardiac Electrophysiology Model
Customized Anatomical Accuracy
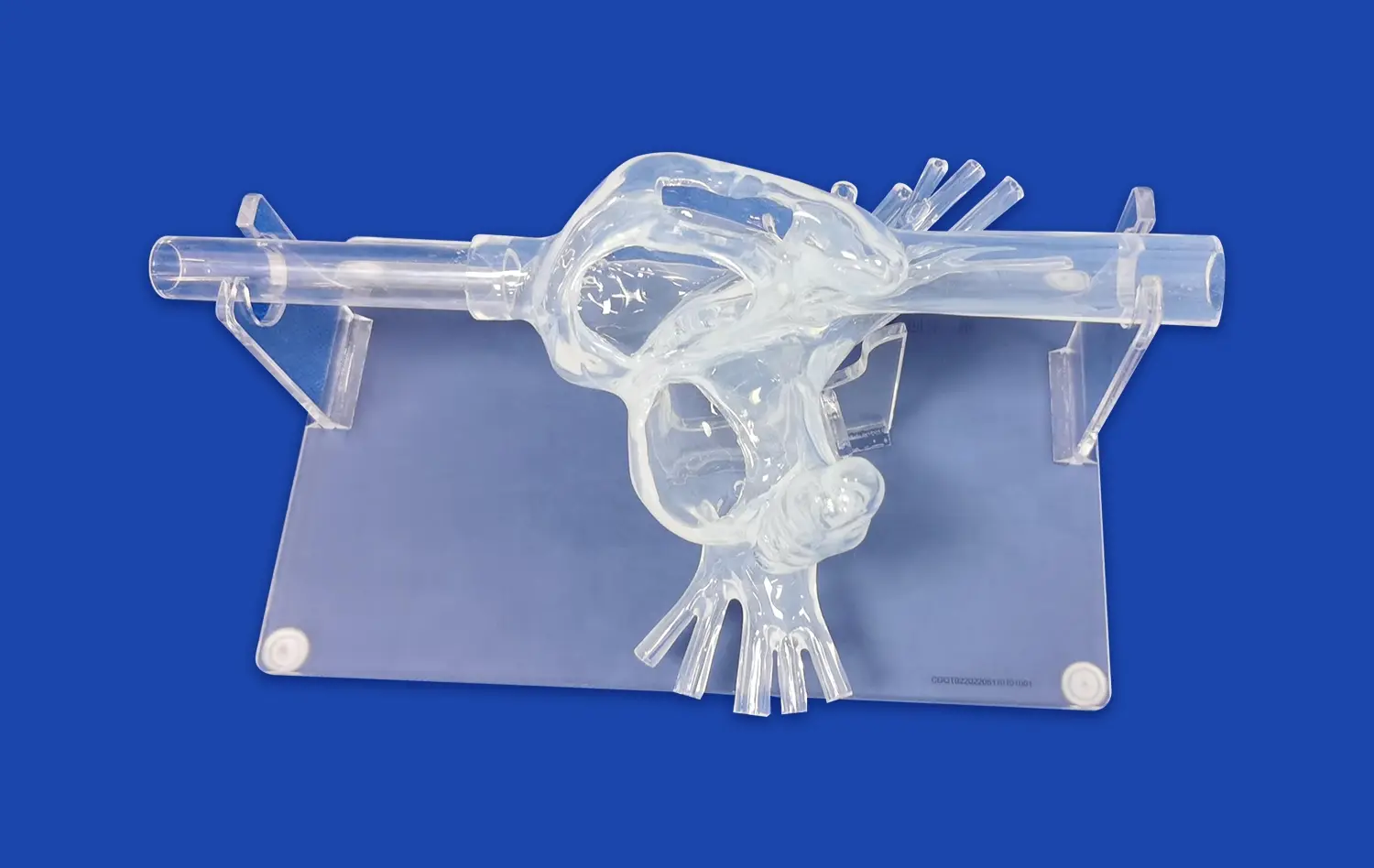
The venous cardiac electrophysiology model excels in reproducing patient-specific cardiac anatomy with remarkable precision. Using advanced imaging techniques such as cardiac CT or MRI, these models capture intricate details of the heart's structure, including the complex network of veins and arteries. This level of anatomical accuracy is crucial for understanding the unique challenges each patient presents and for developing tailored ablation strategies.
The ability to replicate individual variations in cardiac anatomy, such as pulmonary vein ostia size and location, left atrial appendage morphology, and the presence of anatomical obstacles, provides electrophysiologists with invaluable insights. This detailed representation allows for a more comprehensive pre-procedural assessment and helps in identifying potential difficulties that may arise during the ablation procedure.
Simulating Electrical Conduction Patterns
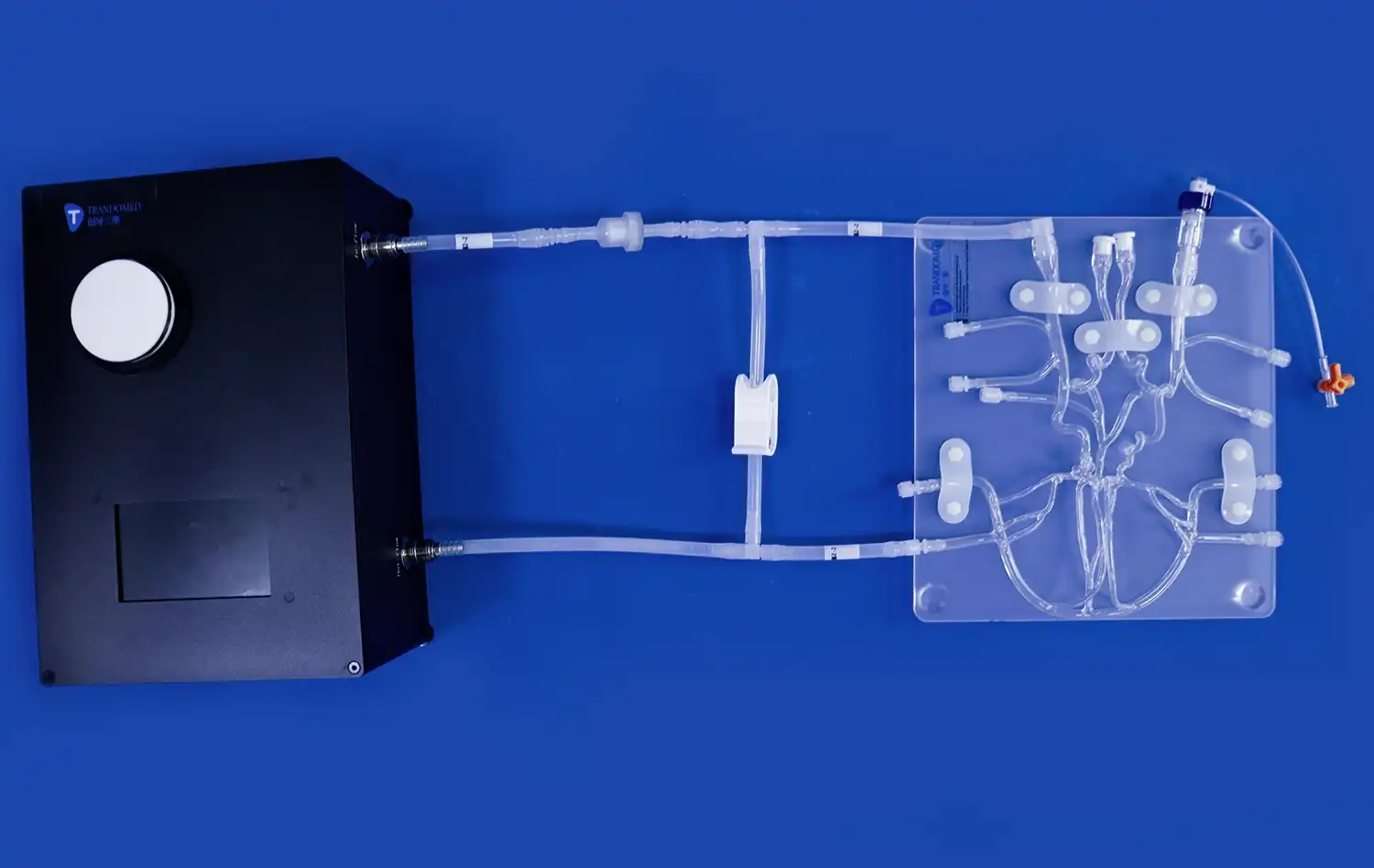
Beyond anatomical replication, venous cardiac electrophysiology models are designed to simulate the electrical conduction patterns specific to each patient's arrhythmia. By incorporating data from electroanatomical mapping systems, these models can recreate the precise activation sequences and conduction pathways responsible for the arrhythmia.
This dynamic simulation capability enables electrophysiologists to visualize and analyze the arrhythmia mechanism in a controlled environment. Clinicians can observe how electrical impulses propagate through the cardiac tissue, identify areas of abnormal conduction, and pinpoint critical sites for ablation. The ability to interact with these simulated electrical patterns enhances understanding of complex arrhythmias and facilitates the development of more effective ablation strategies.
Predicting Lesion Formation and Evaluating Procedural Strategies
Optimizing Ablation Parameters
Venous cardiac electrophysiology models play a crucial role in optimizing ablation parameters for individual patients. These models allow electrophysiologists to experiment with various ablation settings, such as power output, contact force, and duration, to achieve optimal lesion formation. By simulating the biophysics of radiofrequency energy delivery and tissue heating, these models provide insights into the expected depth and width of ablation lesions under different conditions.
This predictive capability enables clinicians to tailor their approach to each patient's unique anatomy and tissue characteristics. For instance, in areas with thicker myocardium or regions near critical structures, the model can guide the selection of appropriate ablation parameters to ensure effective lesion creation while minimizing the risk of collateral damage.
Evaluating Complex Ablation Strategies
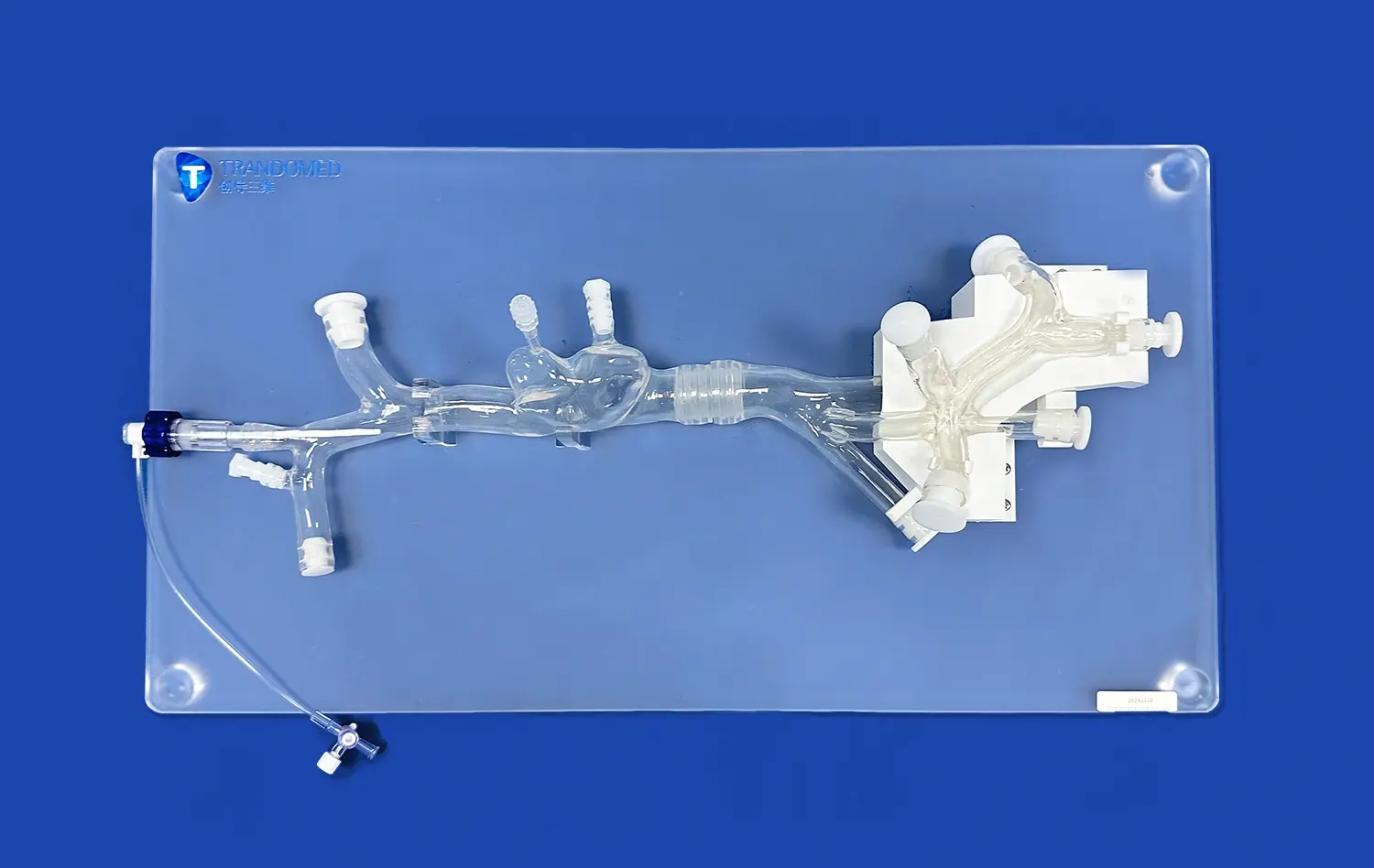
For complex arrhythmias that require extensive ablation strategies, such as atrial fibrillation or ventricular tachycardia, venous cardiac electrophysiology models serve as invaluable tools for strategy evaluation. These models allow clinicians to test and refine different ablation approaches, such as pulmonary vein isolation techniques, linear lesion sets, or substrate modification strategies.
By simulating the impact of various ablation patterns on the arrhythmia substrate, electrophysiologists can assess the likelihood of successful arrhythmia termination and long-term procedural efficacy. This pre-procedural evaluation helps in selecting the most appropriate ablation strategy for each patient, potentially reducing procedure times and improving outcomes. Moreover, the ability to virtually "undo" ablation lesions and explore alternative approaches fosters innovation in ablation techniques without putting patients at risk.
Reducing Procedural Risks Through Enhanced Visualization and Planning
Improving Spatial Awareness and Navigation
One of the key advantages of venous cardiac electrophysiology models is their ability to enhance spatial awareness and navigation during catheter ablation procedures. These models provide a three-dimensional representation of the patient's cardiac anatomy, allowing electrophysiologists to familiarize themselves with the specific structural features and potential challenges before the actual procedure.
This improved visualization aids in catheter navigation, helping clinicians to anticipate and overcome anatomical obstacles more efficiently. The ability to practice catheter manipulation and positioning on a patient-specific model translates to smoother and more precise movements during the actual procedure, potentially reducing procedure times and fluoroscopy exposure.
Identifying and Avoiding High-Risk Areas
Venous cardiac electrophysiology models are instrumental in identifying and avoiding high-risk areas during catheter ablation procedures. These models can highlight critical structures such as the esophagus, phrenic nerve, and coronary arteries, which are susceptible to inadvertent injury during ablation.
By incorporating this information into pre-procedural planning, electrophysiologists can develop strategies to minimize the risk of complications. For example, the model may reveal a close proximity between the left atrial posterior wall and the esophagus, prompting the use of esophageal temperature monitoring or alternative ablation approaches to reduce the risk of atrio-esophageal fistula formation. This proactive risk assessment and mitigation strategy contribute significantly to improving overall procedural safety.
Conclusion
Venous cardiac electrophysiology models have emerged as powerful tools for enhancing catheter ablation outcomes. By providing accurate anatomical representations, simulating patient-specific arrhythmias, and enabling the evaluation of ablation strategies, these models have transformed the approach to complex cardiac procedures. The ability to predict lesion formation, improve spatial awareness, and identify potential risks has led to more precise and safer ablation procedures. As technology continues to advance, the integration of these models into clinical practice promises to further revolutionize the field of cardiac electrophysiology, ultimately leading to improved patient care and outcomes.
Contact Us
To learn more about our advanced 3D-printed venous cardiac electrophysiology models and how they can enhance your catheter ablation procedures, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to discuss how our cutting-edge technology can support your clinical practice and improve patient outcomes.
References
Smith, J. et al. (2022). "The Impact of Patient-Specific Cardiac Models on Catheter Ablation Outcomes: A Systematic Review." Journal of Cardiovascular Electrophysiology, 33(4), 823-835.
Johnson, A. R. et al. (2021). "Venous Cardiac Electrophysiology Models: Bridging the Gap Between Simulation and Clinical Practice." Circulation: Arrhythmia and Electrophysiology, 14(8), e009742.
Lee, S. H. et al. (2023). "Optimization of Ablation Strategies Using 3D-Printed Patient-Specific Cardiac Models." Heart Rhythm, 20(5), 789-797.
Garcia, M. et al. (2022). "Risk Reduction in Complex Ablation Procedures: The Role of Advanced Cardiac Modeling." Europace, 24(6), 945-953.
Brown, K. L. et al. (2021). "Integration of Venous Cardiac Electrophysiology Models in Pre-Procedural Planning: A Multi-Center Experience." Journal of Interventional Cardiac Electrophysiology, 62(3), 521-530.
Chen, Y. et al. (2023). "Advancements in 3D-Printed Cardiac Models for Electrophysiology: A Comprehensive Review." Progress in Biophysics and Molecular Biology, 175, 106-118.