Which Procedural Techniques Benefit Most from Customizable Models?
Pulmonary Embolectomy Simulation
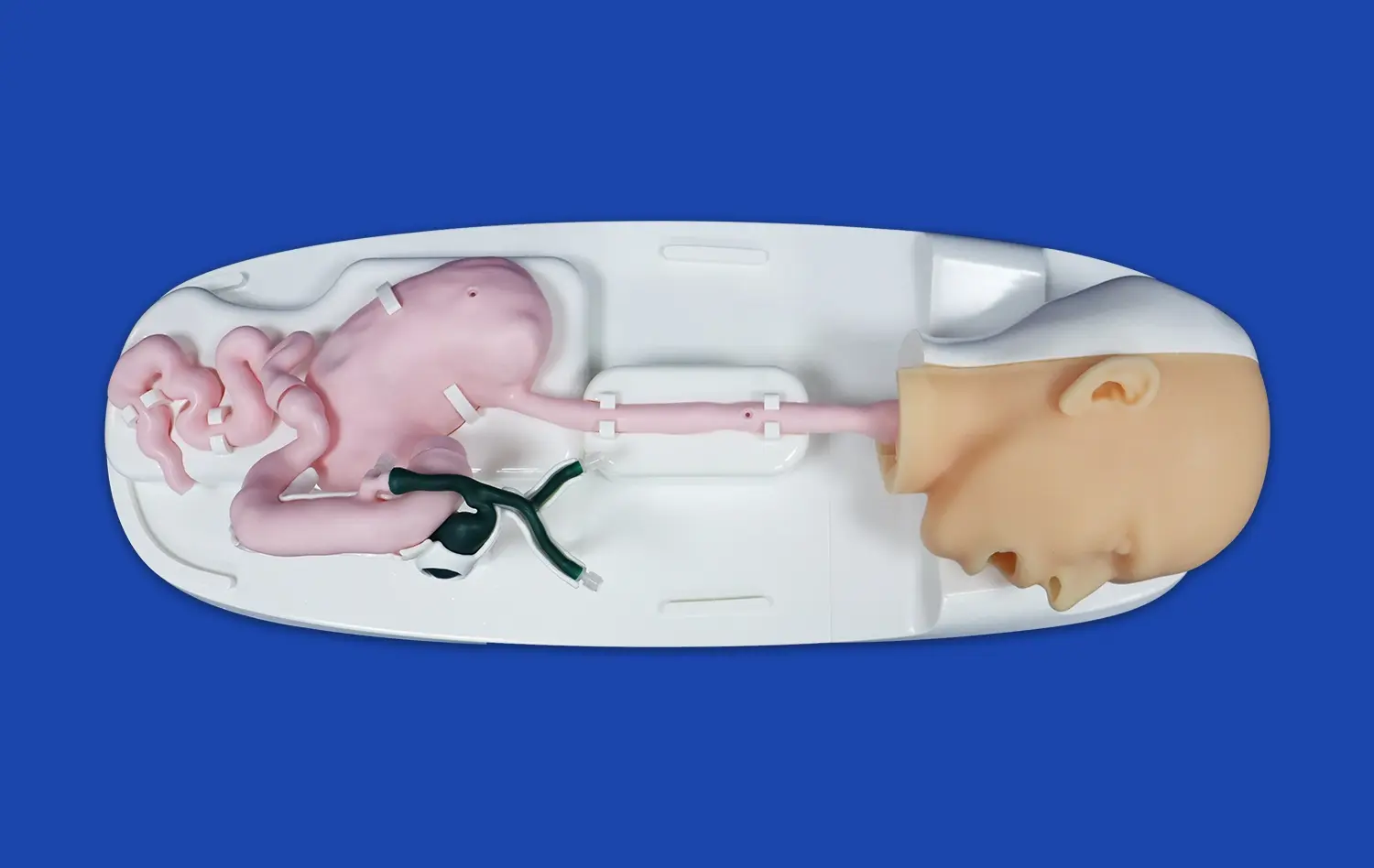
Customizable pulmonary artery models prove invaluable for practicing pulmonary embolectomy techniques. These models can be designed to incorporate simulated emboli at various locations within the pulmonary vasculature, allowing interventionalists to refine their skills in navigating catheters and devices through complex anatomical structures. The ability to replicate different embolus sizes and positions enables practitioners to develop strategies for addressing a wide range of clinical scenarios, ultimately improving their efficiency and success rates in real-world procedures.
Balloon Pulmonary Angioplasty Training
For interventionalists specializing in the treatment of chronic thromboembolic pulmonary hypertension (CTEPH), customizable pulmonary artery models offer an unparalleled platform for mastering balloon pulmonary angioplasty techniques. These models can be crafted to mimic the characteristic web-like obstructions and vessel narrowing associated with CTEPH, providing a realistic environment for practicing catheter navigation, balloon sizing, and inflation techniques. The tactile feedback offered by high-fidelity silicone models enhances the learning experience, allowing practitioners to develop a nuanced understanding of the forces involved in successful angioplasty procedures..
Pulmonary Artery Stenting Practice
Interventional radiologists and cardiologists can significantly benefit from customizable models when honing their skills in pulmonary artery stenting. These models can be designed to replicate various types of stenoses, from discrete lesions to more diffuse narrowing, enabling practitioners to practice precise stent placement and deployment. The ability to incorporate realistic vessel compliance and tortuosity in the models ensures that the simulation closely mirrors the challenges encountered in clinical practice, thereby enhancing the transferability of skills from the training environment to actual patient care.
Advantages of Modular Pulmonary Artery Models for Skill Development
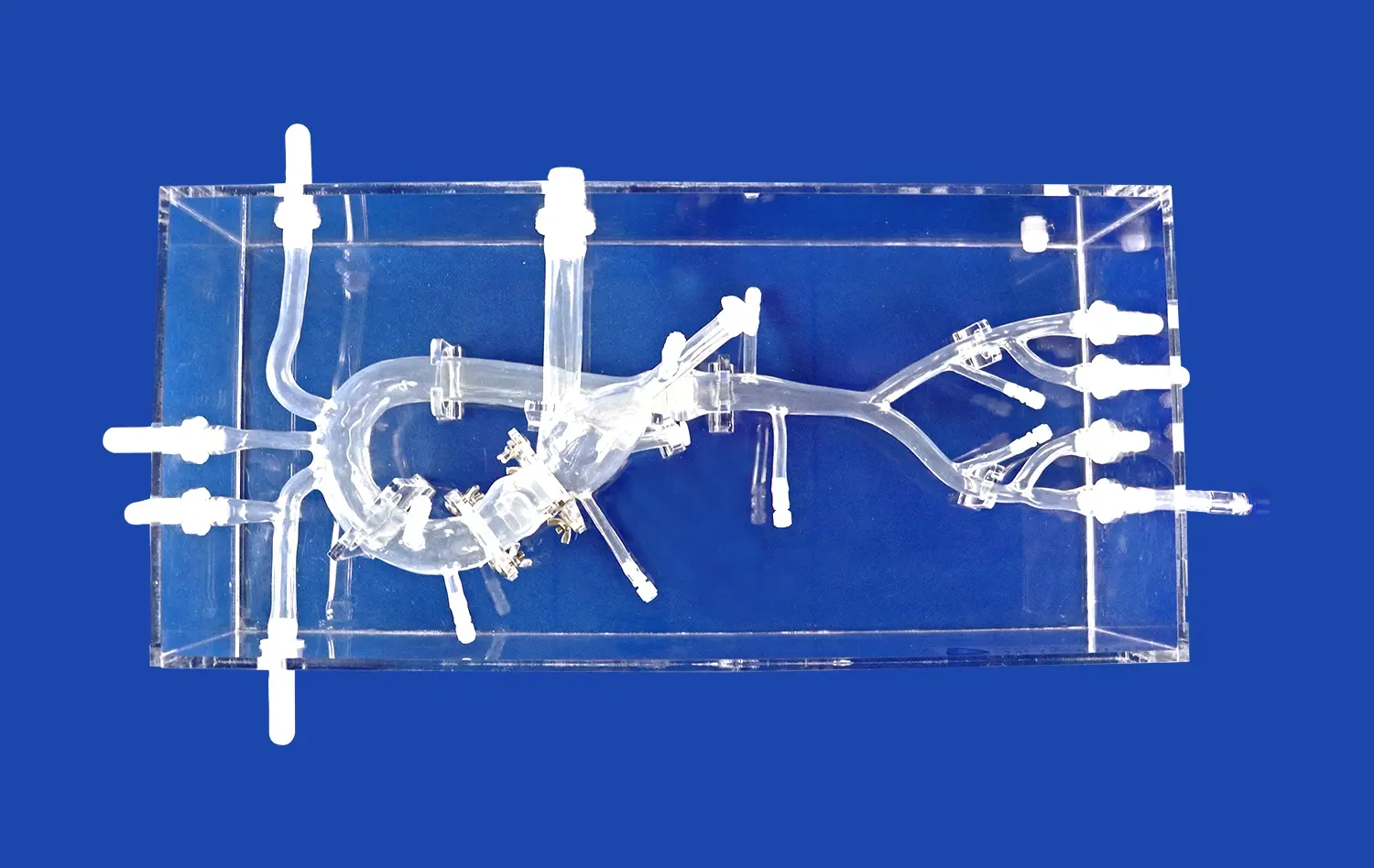
Adaptability to Various Training Scenarios
Modular pulmonary artery models offer unparalleled versatility in medical training. The ability to detach and replace different sections, such as the superior vena cava (SVC) and right heart components, allows for the creation of diverse training scenarios. This adaptability enables educators to present trainees with a wide range of anatomical variations and pathological conditions, ensuring a comprehensive learning experience. For instance, the modular design facilitates the simulation of congenital heart defects or acquired vascular anomalies, providing valuable exposure to rare but critical clinical presentations.
Progressive Skill Development
The modular nature of these advanced simulators supports a structured approach to skill development. Trainees can begin with simpler configurations, focusing on basic catheter navigation and wire manipulation techniques. As their proficiency grows, more complex modules can be introduced, gradually increasing the difficulty and realism of the simulated procedures. This stepwise progression allows for the systematic building of confidence and competence, mirroring the natural learning curve experienced in clinical practice. The ability to isolate specific anatomical regions such as the pulmonary artery model also enables targeted practice on areas of weakness, promoting efficient and effective skill improvement..
Enhanced Collaborative Learning
Modular pulmonary artery models foster collaborative learning environments. The ability to quickly reconfigure the model allows multiple trainees to practice different scenarios in rapid succession, promoting dynamic group discussions and peer-to-peer learning. Furthermore, the modularity enables simultaneous practice on different sections of the model, maximizing resource utilization in training settings. This collaborative approach not only enhances individual skill development but also cultivates teamwork and communication skills essential in real-world interventional settings.
Enhancing Precision and Confidence in Interventional Procedures
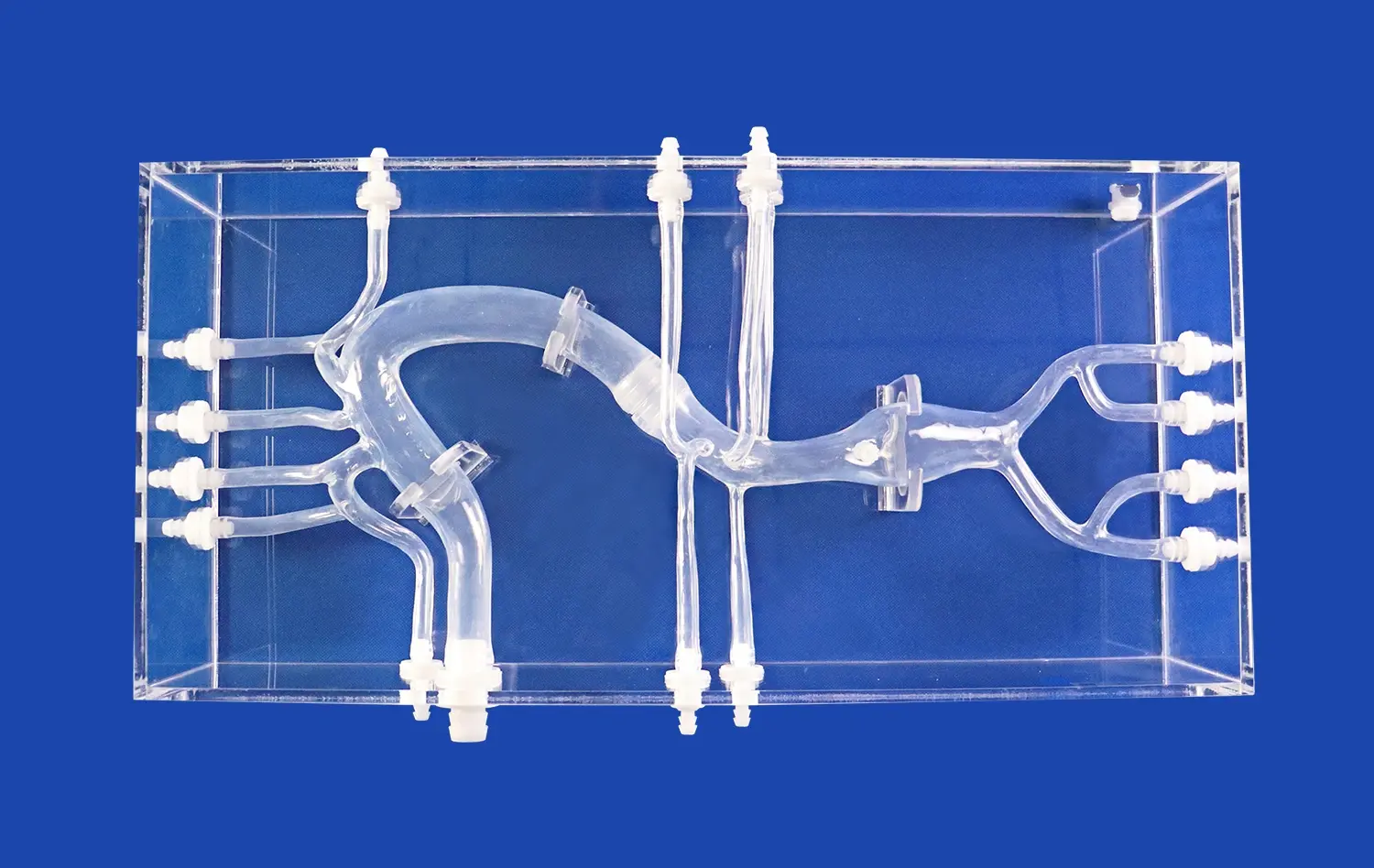
Realistic Tactile Feedback
High-fidelity pulmonary artery models, particularly those crafted from advanced silicone materials, provide remarkably realistic tactile feedback. This haptic realism is crucial for developing the nuanced skills required in interventional procedures. As practitioners manipulate catheters and guidewires within these models, they experience resistance and sensations closely mimicking those encountered in actual patients. This tactile accuracy allows for the refinement of fine motor skills and the development of a tactile memory that translates directly to improved performance in clinical settings. The ability to feel subtle differences in tissue compliance and vessel tortuosity enhances the interventionalist's ability to navigate complex vascular anatomy safely and efficiently.
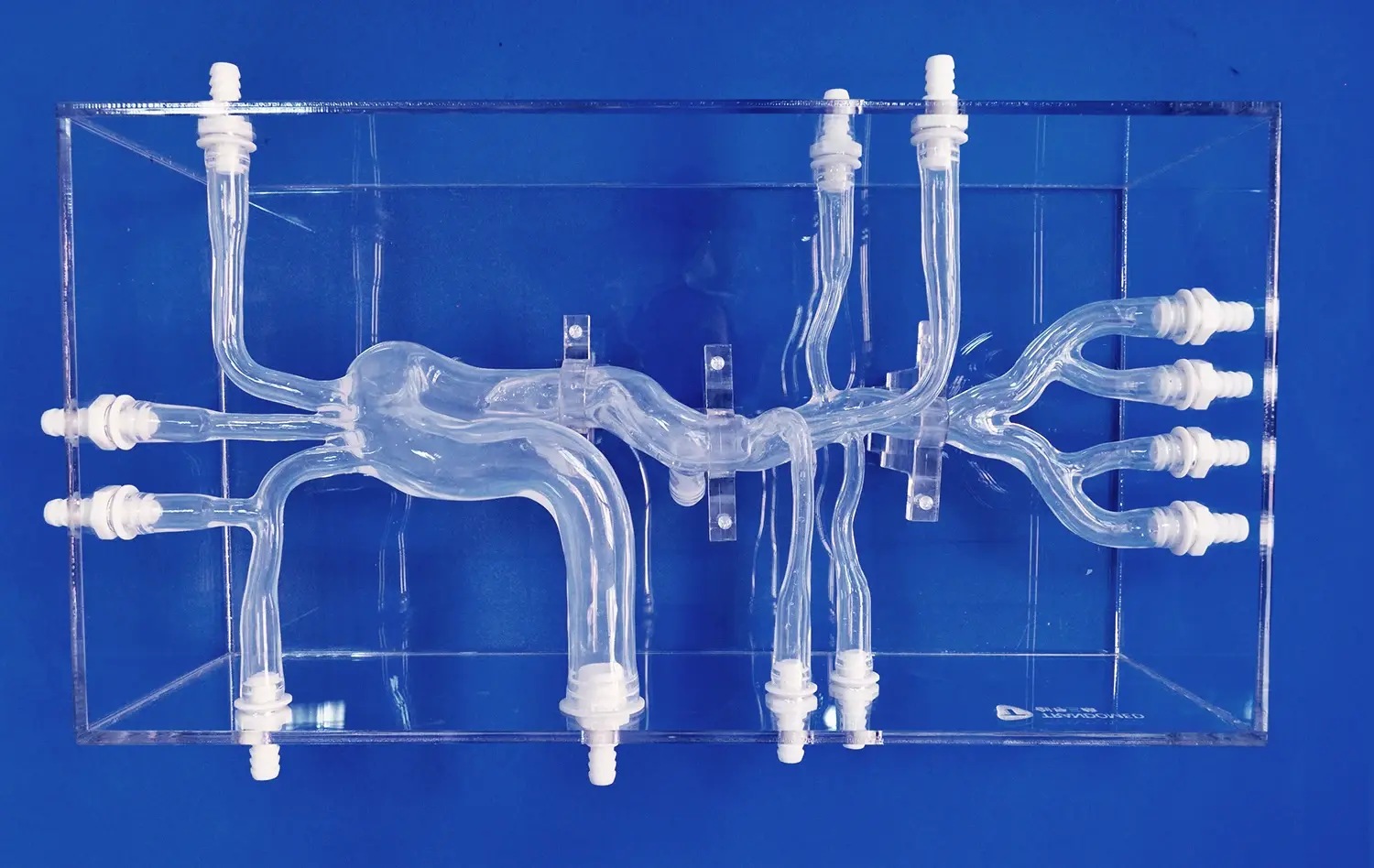
Visualization of Complex Anatomical Structures
Customizable pulmonary artery models excel in providing clear visualization of intricate vascular structures. The incorporation of transparent materials in key areas allows trainees to observe the movement and positioning of devices within the simulated vasculature. This visual feedback is invaluable for understanding the three-dimensional relationships between different anatomical structures and how they influence procedural techniques. For instance, observing the interaction between a catheter and a simulated vessel bifurcation helps interventionalists develop strategies for navigating challenging anatomical features. This enhanced visualization also aids in the comprehension of fluoroscopic images, as trainees can correlate the two-dimensional fluoroscopic view with the three-dimensional reality of the vascular anatomy.
Repetitive Practice Without Patient Risk
One of the most significant advantages of using customizable pulmonary artery models is the opportunity for unlimited repetitive practice without any risk to patients. This safe learning environment allows interventionalists to push their boundaries, experiment with new techniques, and learn from mistakes without the pressure of potential patient harm. The ability to repeat challenging scenarios multiple times fosters muscle memory and procedural fluency, leading to increased confidence when performing actual interventions. Moreover, this risk-free practice environment encourages innovation, as practitioners can explore novel approaches or test new devices without compromising patient safety. The cumulative effect of this repeated, low-stakes practice is a marked improvement in precision, speed, and overall competence in performing complex pulmonary artery interventions.
Conclusion
Customizable pulmonary artery models represent a significant advancement in interventional cardiology training. By offering realistic simulations of complex vascular anatomy and pathologies, these models enable medical professionals to refine their skills in a safe, controlled environment. The modular design and adaptability of these simulators provide a versatile platform for progressive skill development, collaborative learning, and targeted practice. As the field of interventional cardiology continues to evolve, the role of high-fidelity simulation in enhancing procedural precision and practitioner confidence becomes increasingly crucial. Embracing these innovative training tools paves the way for improved patient outcomes and advances in interventional techniques.
Contact Us
Elevate your interventional skills with Trandomed's state-of-the-art customizable pulmonary artery models. Our advanced simulators offer unparalleled realism and versatility, designed to meet the diverse needs of medical professionals and institutions. Experience the benefits of risk-free, hands-on training that translates directly to improved clinical performance. For more information on our customizable pulmonary artery models and how they can enhance your training program, contact us at jackson.chen@trandomed.com. Take the next step in revolutionizing your interventional cardiology training today.
_1736216292718.webp)
_1735798438356.webp)