Aneurysm models have revolutionized neurosurgical training and planning, offering a game-changing approach to improving surgical precision. These intricate replicas of cerebral vasculature provide neurosurgeons with a hands-on, risk-free environment to hone their skills and strategize complex procedures. By incorporating lifelike aneurysms and anatomically accurate blood vessels, these models enable practitioners to visualize, practice, and perfect their techniques before entering the operating room. The result is enhanced surgical confidence, reduced procedural risks, and ultimately, better patient outcomes. As medical technology advances, the role of high-fidelity aneurysm simulation in neurosurgical education and preoperative planning continues to grow, promising a future of safer, more effective treatments for this life-threatening condition.
How Do Simulation Models Reduce Surgical Risk?
Enhancing Preoperative Planning
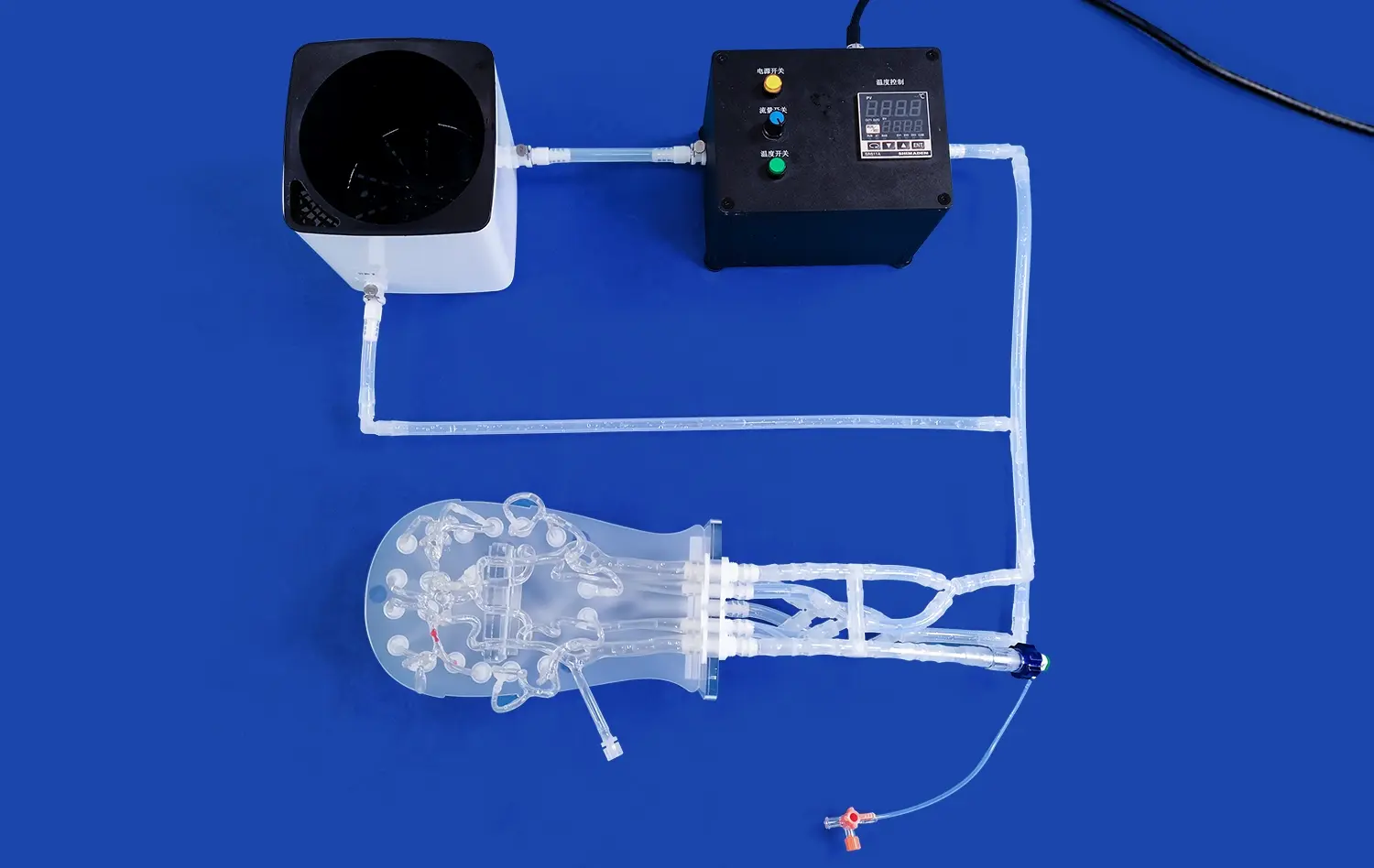
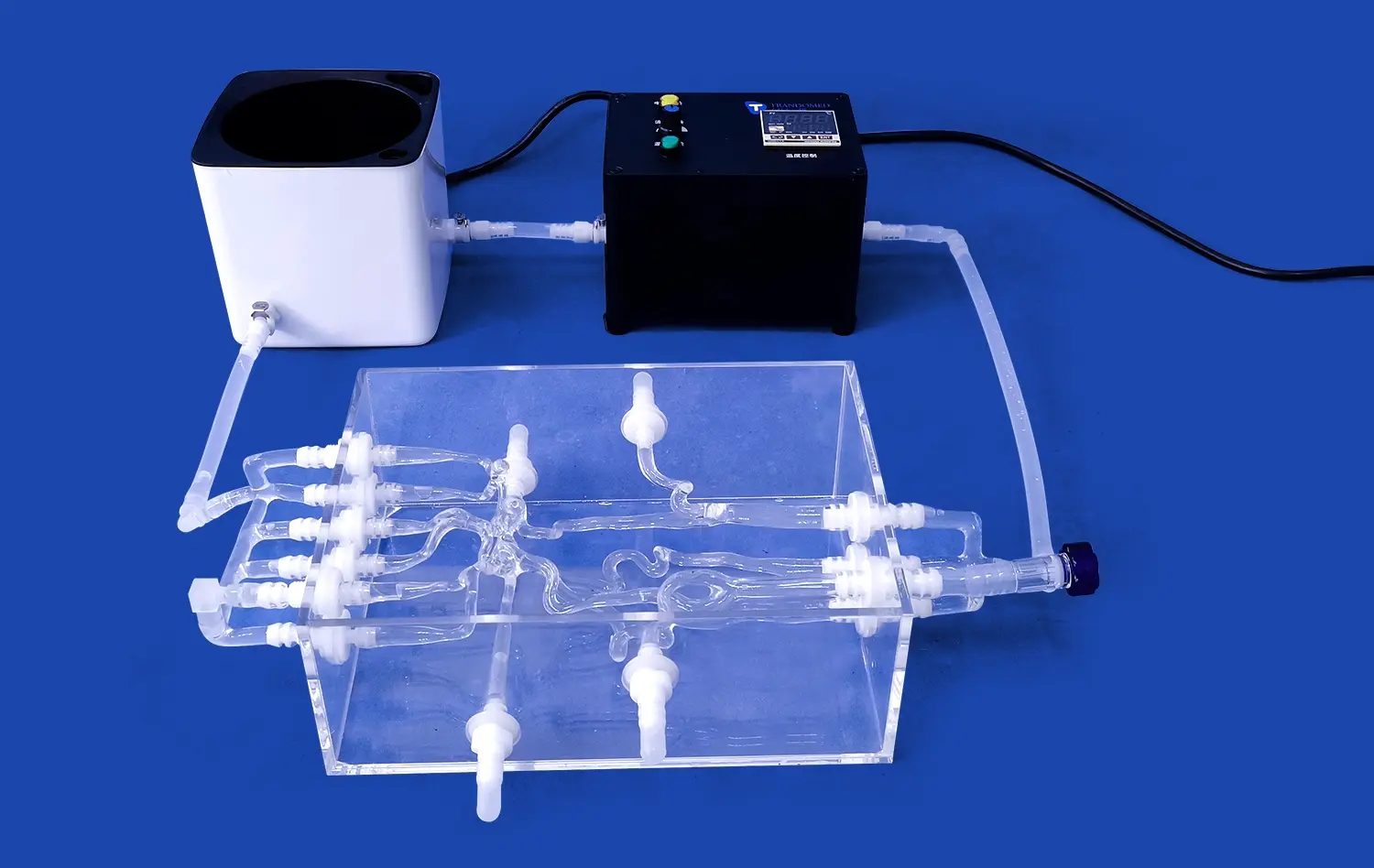
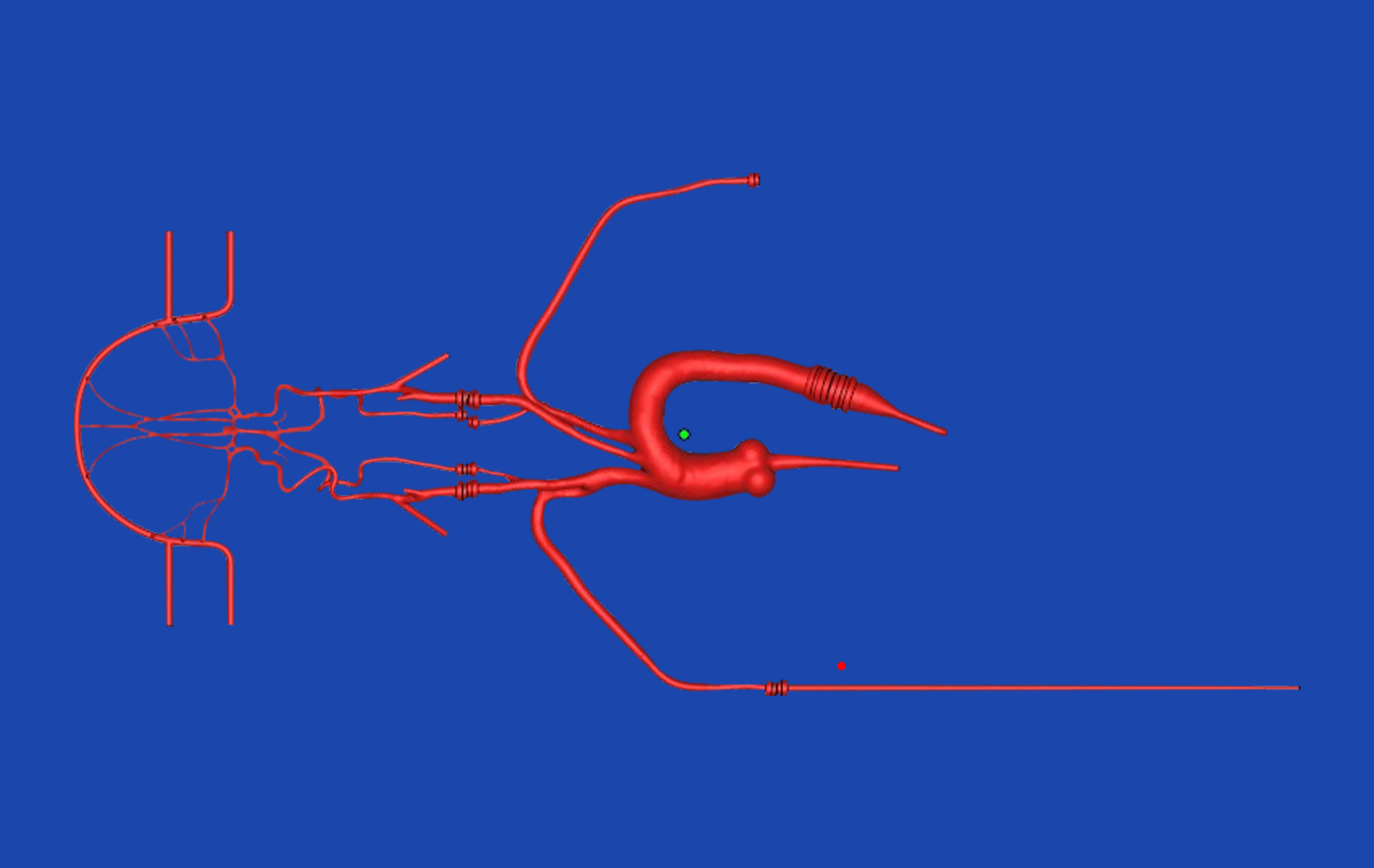
Simulation models, particularly those replicating intracranial vascular structures with aneurysms, play a crucial role in reducing surgical risks by enabling thorough preoperative planning. These models, such as the SJX011 Intracranial Vascular with Aneurysm Model, provide surgeons with a tangible, three-dimensional representation of the patient's unique cerebral vasculature. This allows for a detailed examination of the aneurysm's size, shape, and location in relation to surrounding arteries.
By studying these models, neurosurgeons can:
- Identify potential challenges and complications before surgery
- Determine the optimal approach for aneurysm clipping or coiling
- Practice and refine their techniques on a patient-specific model
- Reduce operative time and improve surgical outcomes
Improving Spatial Awareness
One of the key benefits of using aneurysm simulation models is the enhancement of a surgeon's spatial awareness. The complex, three-dimensional nature of cerebral vasculature can be challenging to fully comprehend from two-dimensional imaging alone. High-fidelity models that accurately replicate the tortuous internal carotid artery, along with the anterior and middle cerebral arteries, provide surgeons with a tactile understanding of the spatial relationships within the brain.
This improved spatial awareness translates to:
- Better navigation during minimally invasive procedures
- Reduced risk of inadvertently damaging nearby healthy tissue
- Increased confidence in executing surgical maneuvers
- Enhanced ability to adapt to unexpected anatomical variations
Facilitating Team Communication
Aneurysm models serve as powerful communication tools within surgical teams. By providing a shared, tangible reference point, these models facilitate discussions between neurosurgeons, interventional radiologists, and other team members. This collaborative approach to surgical planning can lead to:
- Improved coordination during complex procedures
- Better anticipation of potential complications
- More effective distribution of roles and responsibilities
- Enhanced overall team performance in the operating room
Training for Clipping and Coiling Procedures
Mastering Aneurysm Clipping Techniques
Aneurysm clipping is a delicate neurosurgical procedure that requires precision and extensive practice. High-fidelity aneurysm models provide an ideal platform for surgeons to refine their clipping techniques. These models, featuring replaceable aneurysm lesions, allow for repeated practice of clip placement, ensuring optimal occlusion of the aneurysm while preserving blood flow to vital brain tissues.
Key benefits of training with aneurysm models for clipping procedures include:
- Perfecting clip selection and positioning
- Improving hand-eye coordination in a 3D space
- Practicing management of intraoperative ruptures
- Developing strategies for complex aneurysm morphologies
Enhancing Endovascular Coiling Skills
Endovascular coiling has emerged as a minimally invasive alternative to surgical clipping for many aneurysms. Training on sophisticated aneurysm models allows interventional neuroradiologists and neurosurgeons to hone their coiling techniques in a risk-free environment. Models that simulate the aneurysm tamponade operation provide realistic feedback, helping practitioners improve their skills in navigating catheters, deploying coils, and managing potential complications.
Advantages of coiling practice on aneurysm models include:
- Refining catheter navigation through tortuous vessels
- Mastering coil placement and packing density
- Practicing adjunctive techniques like balloon-assisted coiling
- Developing strategies for wide-necked or complex aneurysms
Simulating Hybrid Approaches
As treatment strategies for complex aneurysms evolve, hybrid approaches combining open surgical and endovascular techniques are becoming more common. Advanced aneurysm models that allow for both clipping and coiling simulations provide an invaluable training ground for these innovative procedures. By practicing on these versatile models, neurovascular teams can:
- Develop coordinated strategies for complex cases
- Improve decision-making in choosing between clipping and coiling
- Enhance skills in transitioning between open and endovascular approaches
- Prepare for potential complications unique to hybrid procedures
Advancing Microsurgical Techniques with High-Fidelity Models
Perfecting Microdissection Skills
High-fidelity aneurysm models play a crucial role in advancing microsurgical techniques by providing a realistic platform for perfecting microdissection skills. These models, such as the SJX011 Intracranial Vascular with Aneurysm Model, meticulously replicate the delicate structures of the cerebral vasculature, allowing neurosurgeons to practice precise dissection techniques under microscopic visualization.
Benefits of microdissection training on aneurysm models include:
- Enhancing fine motor skills essential for neurovascular surgery
- Improving tissue handling and minimizing trauma to surrounding structures
- Mastering the use of microsurgical instruments in confined spaces
- Developing strategies for exposing aneurysms while preserving perforating arteries
Innovating Bypass Techniques
Complex aneurysms sometimes require bypass procedures to maintain blood flow while excluding the aneurysm from circulation. High-fidelity models that incorporate replaceable aneurysm lesions and customizable vascular anatomy provide an excellent platform for innovating and refining bypass techniques. Neurosurgeons can practice various bypass configurations, including:
- Superficial temporal artery to middle cerebral artery (STA-MCA) bypass
- High-flow bypass using saphenous vein or radial artery grafts
- In situ bypass techniques for complex anterior circulation aneurysms
- Excimer laser-assisted non-occlusive anastomosis (ELANA) technique
Exploring Novel Approaches
The field of neurovascular surgery is continually evolving, with new techniques and technologies emerging to address challenging aneurysms. High-fidelity aneurysm models serve as an invaluable tool for exploring and developing these novel approaches. By providing a safe and reproducible environment for experimentation, these models facilitate:
- Testing of new clip designs and application techniques
- Development of minimally invasive corridor approaches to deep-seated aneurysms
- Refinement of endoscope-assisted microsurgical techniques
- Evaluation of emerging technologies like augmented reality in aneurysm surgery
Conclusion
The integration of high-fidelity aneurysm models into neurosurgical training and preoperative planning has marked a significant leap forward in improving surgical precision and patient outcomes. These sophisticated tools provide an unparalleled opportunity for surgeons to hone their skills, innovate new techniques, and tackle complex cases with increased confidence. As the technology behind these models continues to advance, we can anticipate even more realistic simulations that bridge the gap between training and actual surgical scenarios. The future of neurovascular surgery looks promising, with aneurysm models playing a pivotal role in shaping more skilled surgeons and safer, more effective treatments for patients with this life-threatening condition.
Contact Us
At Trandomed, we are committed to advancing the field of neurosurgery through our state-of-the-art aneurysm models. Our team of experts is dedicated to providing customized solutions that meet the unique needs of medical professionals and institutions worldwide. To learn more about how our high-fidelity models can enhance your surgical training program or research initiatives, please contact us at jackson.chen@trandomed.com. Together, we can work towards a future of improved surgical outcomes and enhanced patient care in the treatment of cerebral aneurysms.
References
Lawton, M. T., & Lang, M. J. (2019). The role of simulation in neurosurgical education: a survey of 99 United States neurosurgery program directors. World Neurosurgery, 122, e439-e446.
Benet, A., Plata-Bello, J., Abla, A. A., Acevedo-Bolton, G., Saloner, D., & Lawton, M. T. (2015). Implantation of 3D-printed patient-specific aneurysm models into cadaveric specimens: a new training paradigm to allow for improvements in cerebrovascular surgery and research. BioMed Research International, 2015.
Winkler-Schwartz, A., Bajunaid, K., Mullah, M. A., Marwa, I., Alotaibi, F. E., Fares, J., ... & Del Maestro, R. F. (2016). Bimanual psychomotor performance in neurosurgical resident applicants assessed using NeuroTouch, a virtual reality simulator. Journal of Surgical Education, 73(6), 942-953.
Choque-Velasquez, J., Colasanti, R., Resendiz-Nieves, J. C., Gonzáles-Echevarría, K. E., Raj, R., Jahromi, B. R., ... & Hernesniemi, J. (2018). Prototaping: 3D printing of the cranial vault for neurosurgical simulation. World Neurosurgery, 109, 356-361.
Mashiko, T., Otani, K., Kawano, R., Konno, T., Kaneko, N., Ito, Y., & Watanabe, E. (2015). Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping. World Neurosurgery, 83(3), 351-361.
Tabani, H., Morone, P. J., Byrne, R. W., & Agarwal, N. (2018). Virtual and augmented reality in neurosurgical education: a systematic review. Neurosurgical Focus, 45(4), E18.
_1734507415405.webp)
_1734507815464.webp)