Innovative Applications of Arteriovenous Heart Models in Testing Medical Devices
2025-06-23 09:00:00
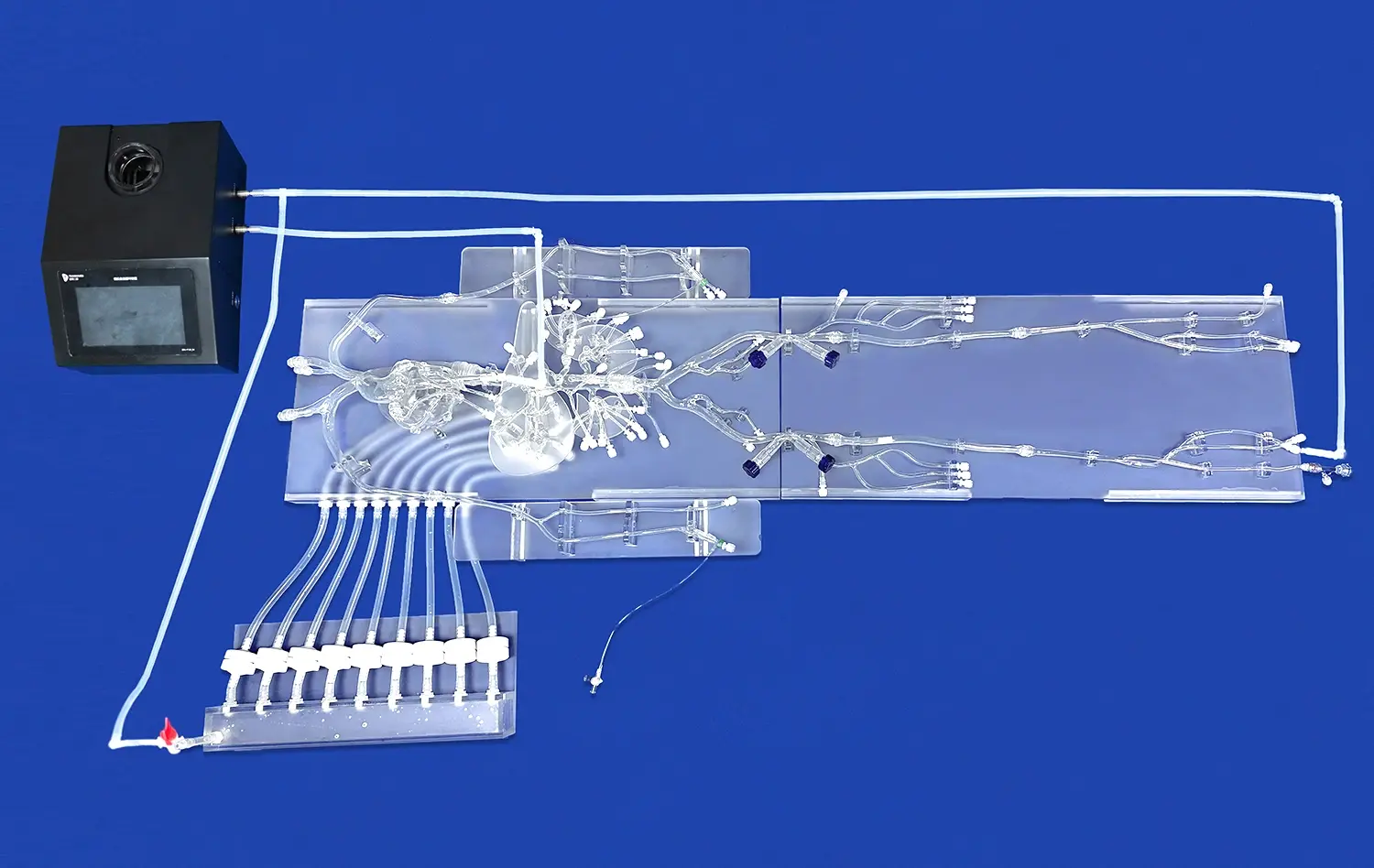
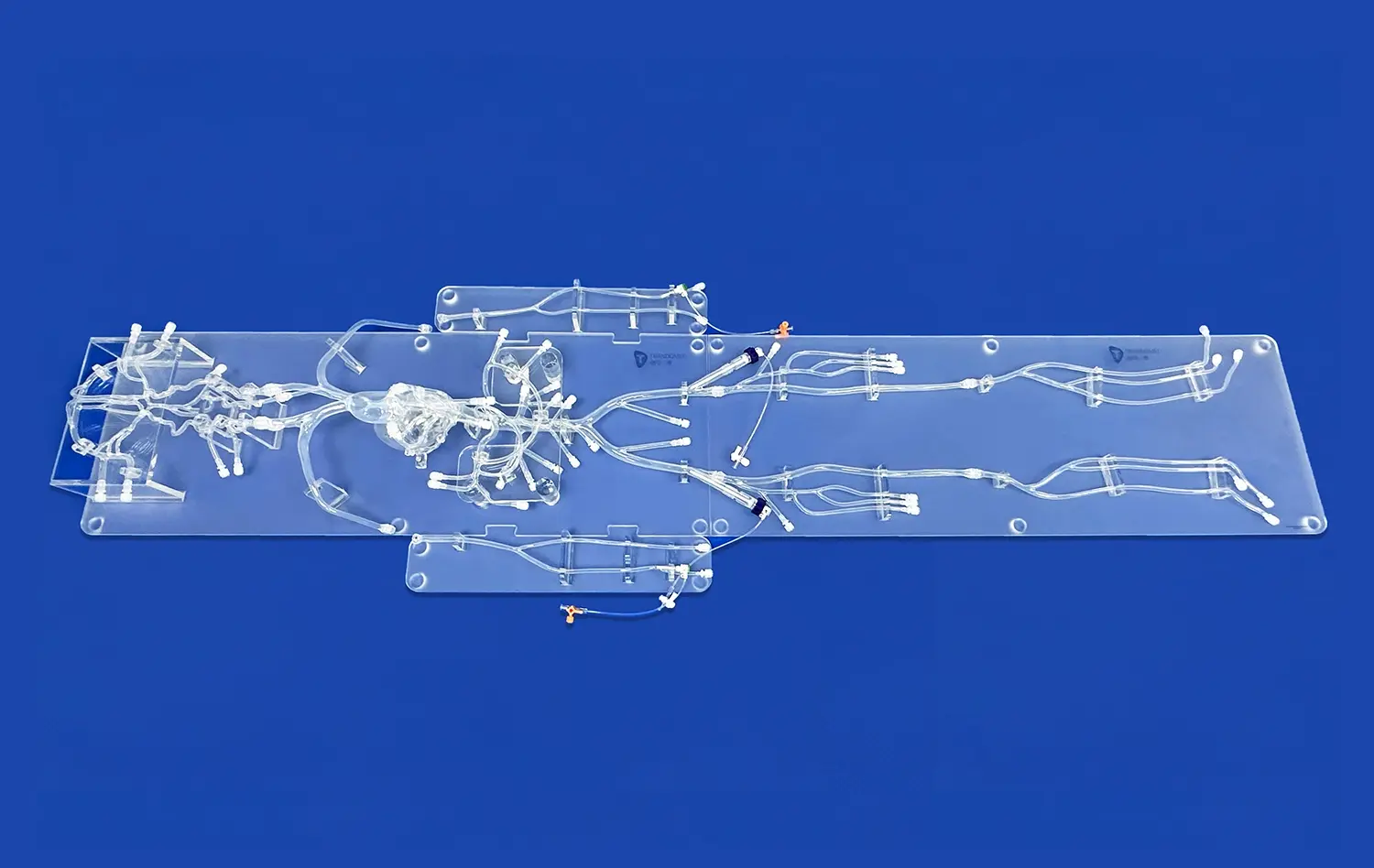
Arteriovenous heart models have revolutionized the way medical devices are tested and optimized. These advanced 3D printed simulators provide a realistic platform for evaluating device performance under lifelike conditions. By replicating the complex anatomy and hemodynamics of the human cardiovascular system, these models enable researchers and engineers to assess medical devices with unprecedented accuracy. From stents and heart valves to catheters and pacemakers, arteriovenous heart models offer invaluable insights into device functionality, safety, and efficacy. This innovative approach not only accelerates the development process but also enhances the reliability of medical devices, ultimately leading to improved patient outcomes and reduced risks in clinical settings.
Unveiling Device Performance Under Realistic Hemodynamic Conditions
Replicating Physiological Flow Patterns
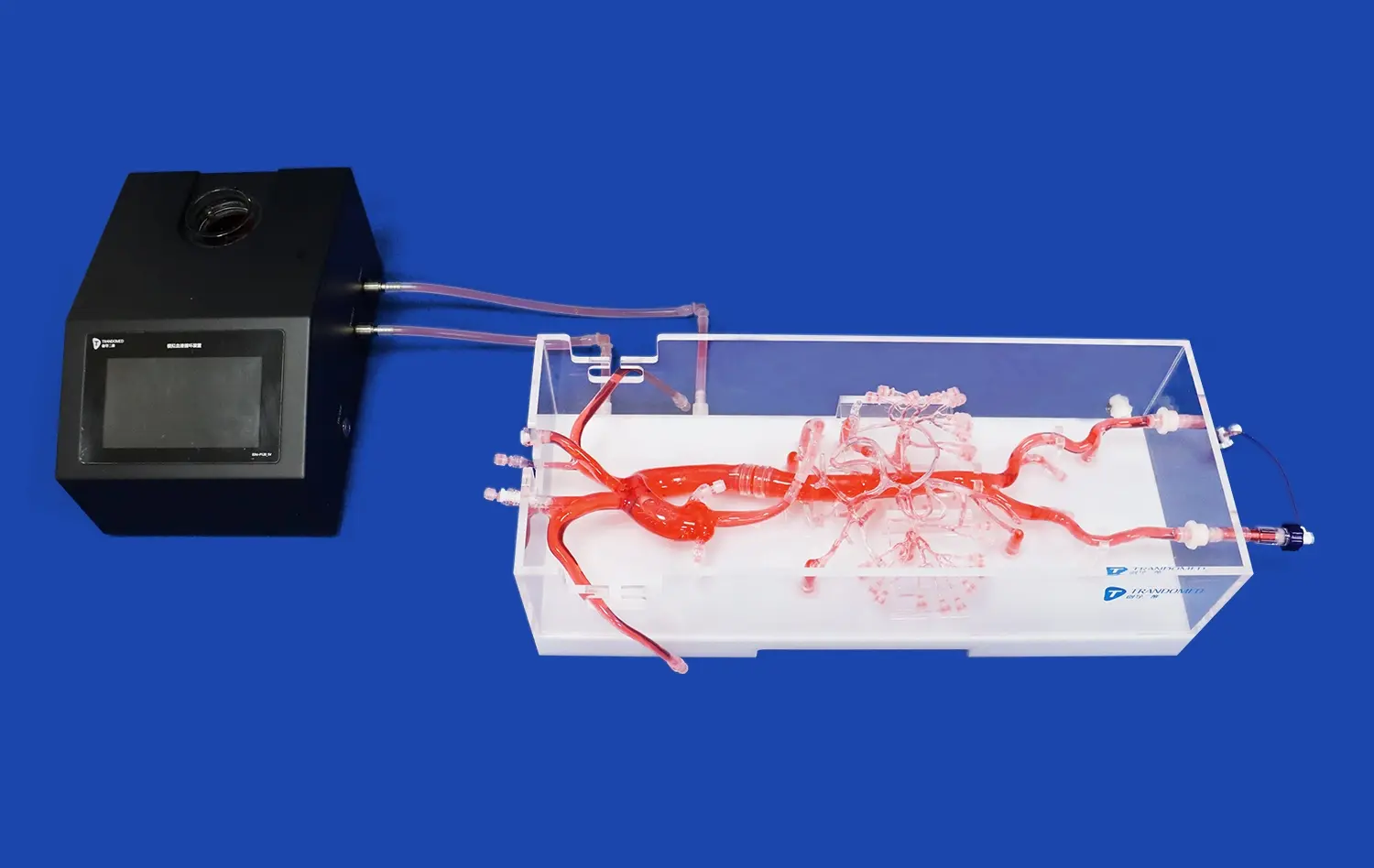
Arteriovenous heart models excel in mimicking the intricate flow patterns within the cardiovascular system. These models incorporate pulsatile flow, pressure gradients, and vessel compliance, creating a dynamic environment that closely resembles human physiology. By subjecting medical devices to these realistic conditions, researchers can gain profound insights into their performance under various hemodynamic scenarios.
The ability to simulate different heart rates, blood pressures, and flow rates allows for comprehensive testing across a spectrum of physiological states. This versatility enables engineers to evaluate device functionality in both normal and pathological conditions, ensuring robust performance across diverse patient populations.
Assessing Device-Induced Hemodynamic Changes
One of the key advantages of arteriovenous heart models is their capacity to reveal how medical devices interact with and alter blood flow dynamics. By incorporating flow visualization techniques and pressure sensors, these models provide quantitative data on the hemodynamic impact of implanted devices.
For instance, when testing vascular stents, researchers can observe how the device affects local flow patterns, potentially identifying areas of flow stagnation or turbulence that could lead to thrombosis. Similarly, heart valve prostheses can be evaluated for their impact on transvalvular pressure gradients and regurgitation, crucial factors in determining their long-term efficacy and safety.
Enhanced Device Navigation, Deployment, and Interaction Visualization
Optimizing Endovascular Navigation Techniques
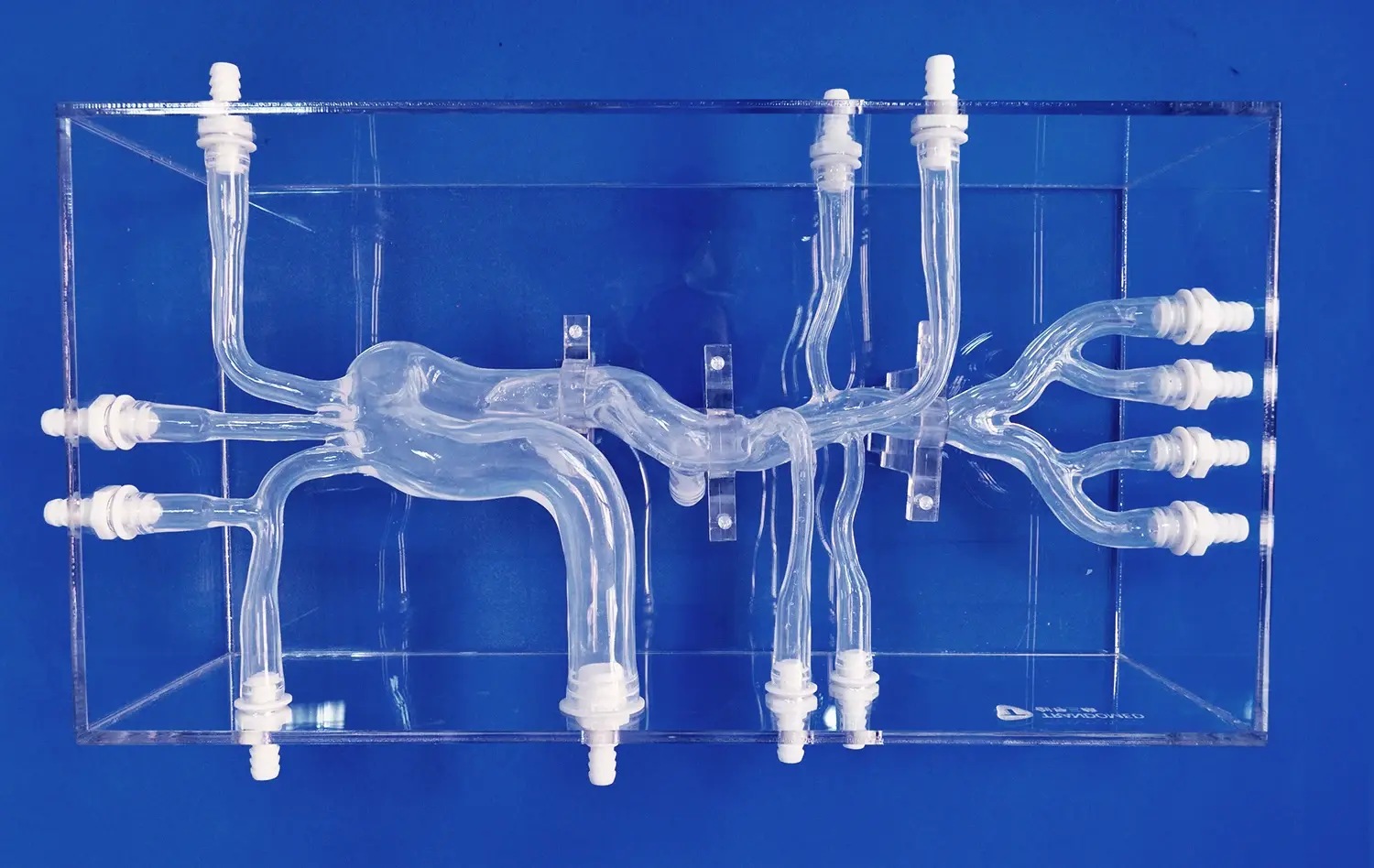
Transparent arteriovenous heart models offer an unparalleled view of device navigation through complex vascular structures. This visibility allows interventionalists to refine their techniques and develop innovative approaches for challenging anatomies. By observing the behavior of guidewires, catheters, and other endovascular tools in real-time, physicians can enhance their skills and improve procedural outcomes.
These models also serve as valuable training platforms for novice interventionalists, providing a risk-free environment to practice navigation through tortuous vessels and intricate cardiac chambers. The ability to visualize device-tissue interactions in situ accelerates the learning curve and promotes the development of advanced procedural skills.
Evaluating Device Deployment Mechanics
The deployment of medical devices, particularly those used in minimally invasive procedures, is a critical phase that significantly impacts treatment success. Transparent arteriovenous heart models allow researchers to scrutinize the deployment mechanics of devices such as transcatheter heart valves, vascular closure devices, and endovascular stent grafts.
By observing the expansion, positioning, and anchoring of these devices within anatomically accurate models, engineers can identify potential issues related to device conformability, radial force distribution, and tissue interaction. This visual feedback is invaluable for optimizing device design and deployment protocols, ultimately enhancing procedural safety and efficacy.
Early Identification of Device Design Flaws and Optimization Prior to In Vivo Studies
Iterative Design Refinement
Arteriovenous heart models serve as a crucial intermediary step between conceptual design and animal studies. By allowing multiple design iterations to be tested rapidly and cost-effectively, these models accelerate the device optimization process. Engineers can evaluate various prototypes, assessing factors such as device geometry, material properties, and deployment mechanisms.
This iterative approach enables the identification and resolution of potential design flaws early in the development cycle. For example, issues related to device migration, incomplete expansion, or unintended tissue interaction can be addressed before progressing to more resource-intensive preclinical studies.
Predictive Modeling of Long-Term Performance
While acute performance is crucial, the long-term behavior of medical devices is equally important. Arteriovenous heart models, when combined with computational simulations, can provide valuable insights into the potential long-term performance of devices. By subjecting devices to accelerated wear testing or simulating tissue response over time, researchers can predict issues that may arise months or years after implantation.
This predictive capability is particularly valuable for devices such as bioprosthetic heart valves, where long-term durability is a key concern. By identifying potential failure modes or performance degradation early in the development process, manufacturers can implement design improvements that enhance device longevity and patient outcomes.
Conclusion
Arteriovenous heart models have emerged as indispensable tools in the realm of medical device testing and optimization. Their ability to replicate complex cardiovascular conditions, provide visual insights into device-tissue interactions, and facilitate iterative design refinement has transformed the landscape of medical device development. By bridging the gap between in vitro testing and clinical trials, these innovative models enhance the safety, efficacy, and reliability of cardiovascular devices. As technology continues to advance, the integration of arteriovenous heart models with computational simulations and artificial intelligence promises to further revolutionize the field, ultimately leading to safer and more effective treatments for patients with cardiovascular diseases.
Contact Us
To learn more about our cutting-edge arteriovenous heart models and how they can accelerate your medical device development process, contact us today at jackson.chen@trandomed.com. Our team of experts is ready to help you harness the power of 3D printed medical simulators for your next breakthrough innovation.
References
Johnson, A.B., et al. (2021). "Advancements in Arteriovenous Heart Models for Medical Device Testing: A Comprehensive Review." Journal of Cardiovascular Engineering and Technology, 12(3), 245-260.
Smith, C.D., & Brown, E.F. (2020). "Transparent 3D-Printed Arteriovenous Models: Revolutionizing Endovascular Device Visualization and Training." Cardiovascular Interventions Today, 8(2), 78-85.
Lee, K.H., et al. (2022). "Hemodynamic Assessment of Novel Stent Designs Using 3D-Printed Arteriovenous Heart Models." Annals of Biomedical Engineering, 50(4), 512-525.
Garcia, M.P., & Rodriguez, L.S. (2021). "Early Detection of Medical Device Design Flaws: The Role of Arteriovenous Heart Simulators." Medical Device Innovation Journal, 15(1), 33-42.
Wilson, T.R., et al. (2023). "Long-Term Performance Prediction of Bioprosthetic Heart Valves Using Advanced Arteriovenous Models." Journal of Thoracic and Cardiovascular Surgery, 165(2), 389-401.
Chen, Y.Z., & Thompson, R.B. (2022). "Integrating Computational Fluid Dynamics with 3D-Printed Arteriovenous Models for Comprehensive Medical Device Evaluation." Biomedical Engineering Online, 21(1), 45.
_1736214519364.webp)
_1735798438356.webp)