Introducing the Internal Carotid Artery Model: Anatomy, Pathology, and Clinical Applications
2025-07-04 09:00:00
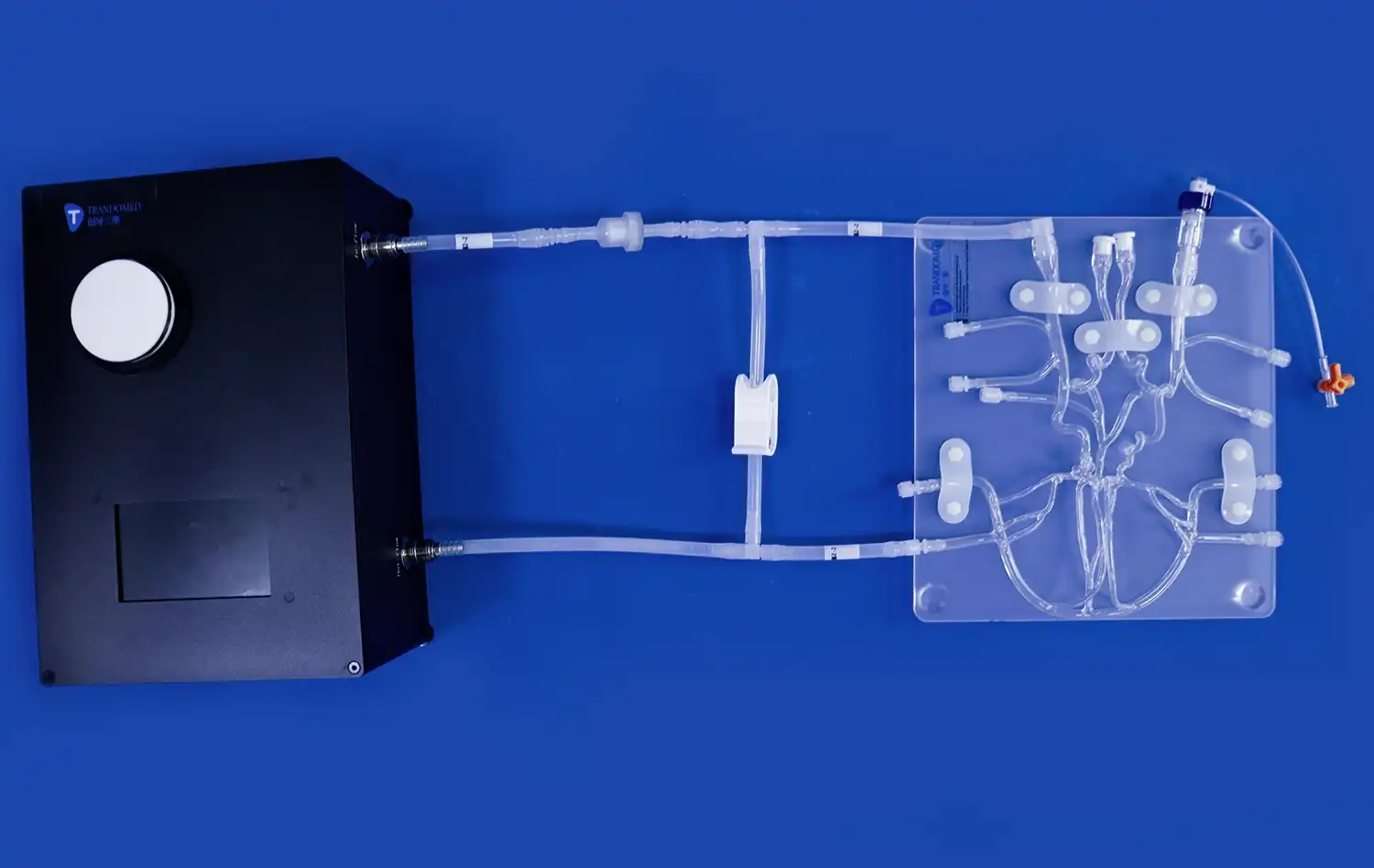
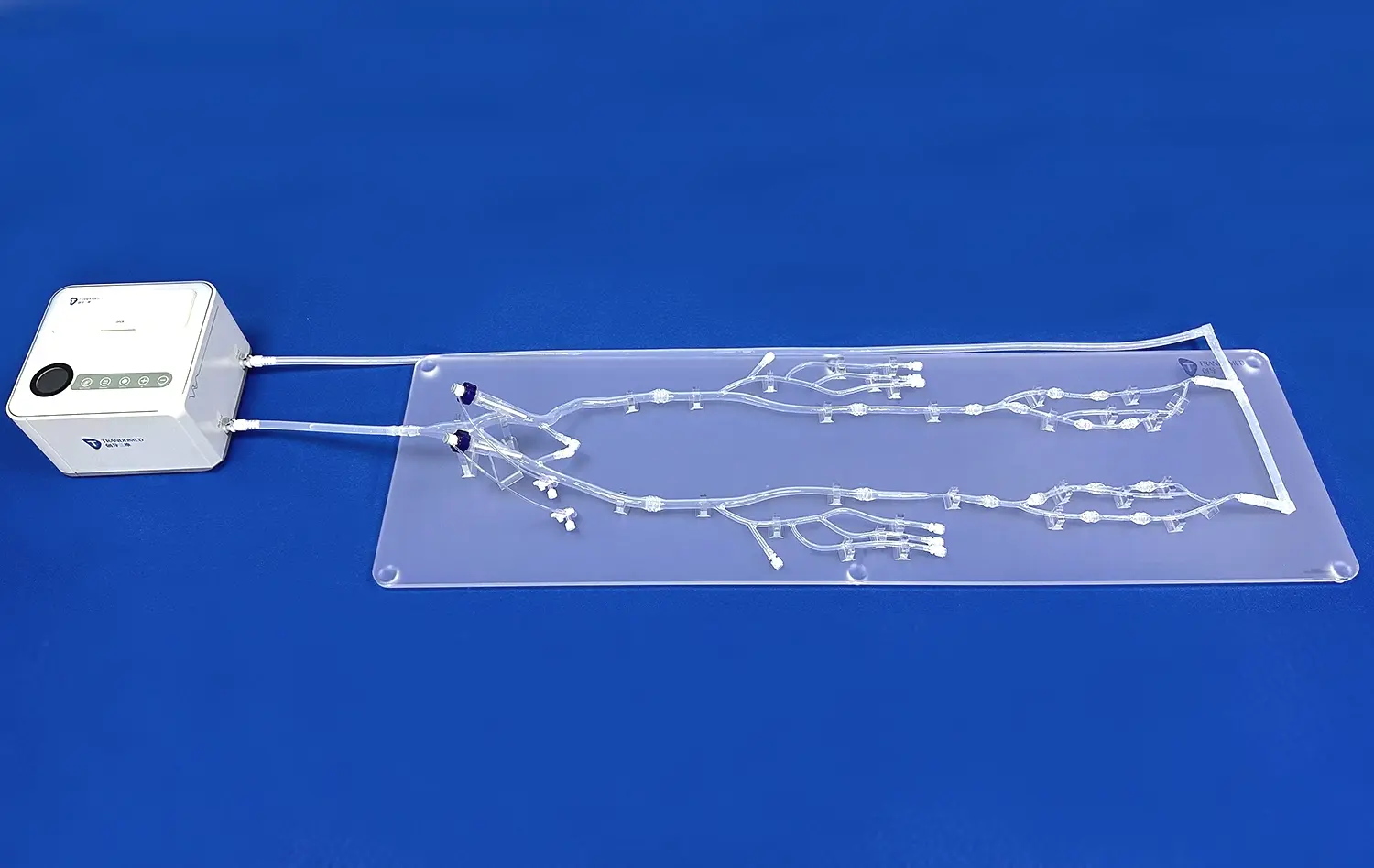
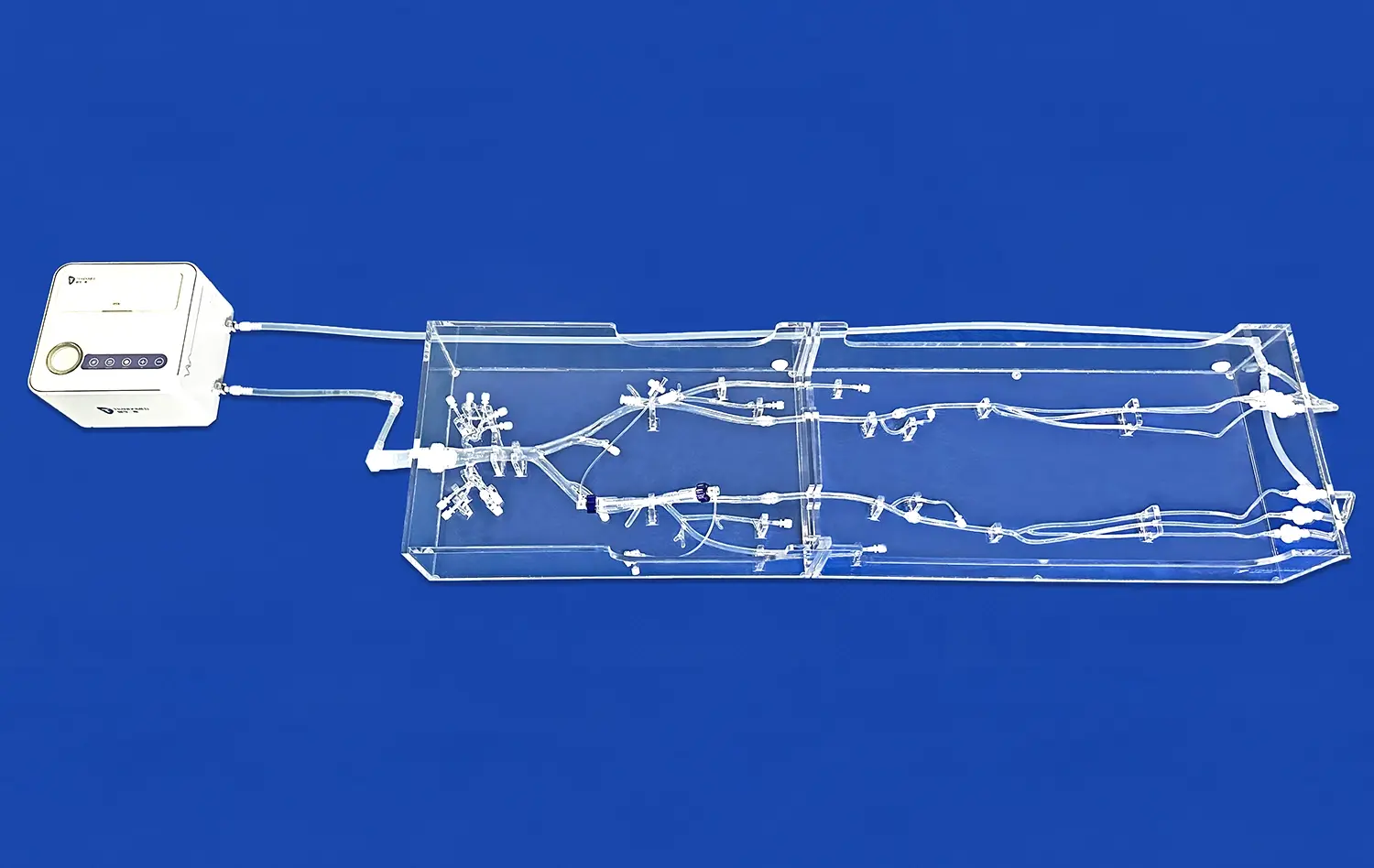
The internal carotid artery model represents a groundbreaking advancement in medical education and training. This innovative 3D printed silicone simulator offers an unparalleled opportunity to explore the intricate anatomy and pathology of one of the body's most crucial blood vessels. By providing a tangible, highly detailed representation of the internal carotid artery, this model bridges the gap between theoretical knowledge and practical application. Medical professionals, students, and researchers can now engage with a lifelike replica that accurately portrays both normal anatomical structures and various pathological conditions. This cutting-edge tool not only enhances understanding but also facilitates the development of critical skills in diagnosis, treatment planning, and surgical interventions related to carotid artery disorders.
Dissecting the Internal Carotid Artery: A Detailed Anatomical Review
Unraveling the Complexities of Carotid Anatomy
The internal carotid artery, a vital conduit supplying oxygenated blood to the brain, holds immense significance in human physiology. This artery's intricate structure and critical function make it a subject of intense study and interest in the medical field. The internal carotid artery model provides an exceptional platform for exploring this complex anatomical feature in unprecedented detail.
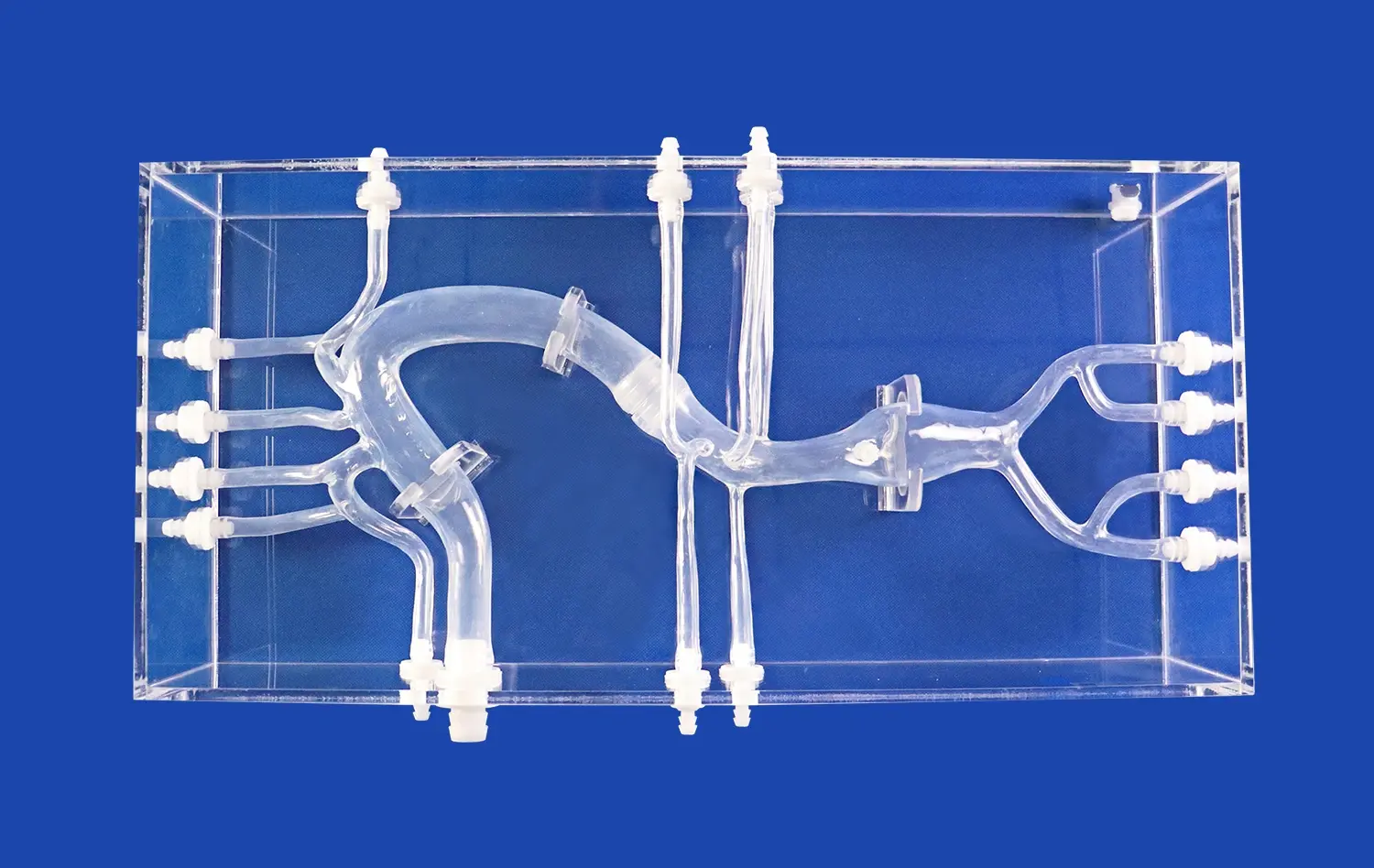
The model meticulously replicates the artery's journey from its origin at the common carotid bifurcation to its terminal branches within the cranial cavity. It showcases the artery's four segments: cervical, petrous, cavernous, and cerebral. Each segment is faithfully reproduced, allowing learners to visualize and understand the artery's course as it navigates through various anatomical landmarks.
Of particular note is the model's representation of the carotid siphon, a unique S-shaped bend in the artery's intracranial portion. This feature, often challenging to conceptualize from two-dimensional images, becomes readily apparent in the three-dimensional model. The ability to physically manipulate and observe this structure from multiple angles significantly enhances spatial understanding and retention of anatomical knowledge.
Exploring Branching Patterns and Variations
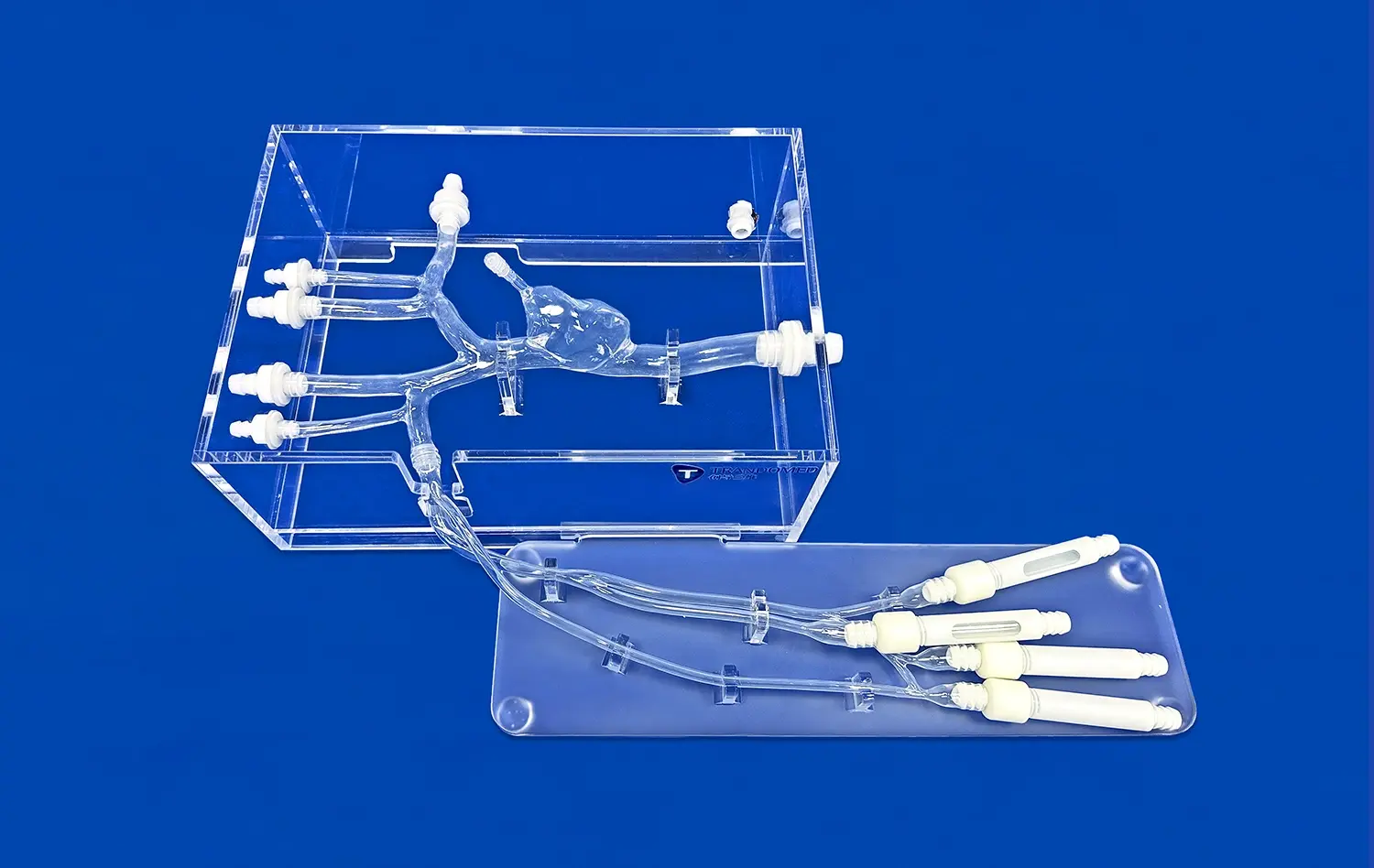
Beyond the main arterial trunk, the internal carotid artery model excels in depicting the complex branching patterns that characterize this vascular structure. It accurately represents major branches such as the ophthalmic artery, posterior communicating artery, and anterior cerebral artery. This level of detail allows for a comprehensive study of the blood supply to various regions of the brain and surrounding structures.
Moreover, the model can be customized to showcase anatomical variations frequently encountered in clinical practice. These may include aberrant branching patterns, persistent embryological vessels, or anomalous courses of the artery itself. By incorporating these variations, the model serves as an invaluable resource for understanding the diversity of vascular anatomy and preparing healthcare professionals for the challenges they may face in real-world scenarios.
Pathological Realism: Simulating Aneurysms and Stenosis in the Internal Carotid Artery Model
Visualizing Vascular Abnormalities
The internal carotid artery model transcends mere anatomical representation by incorporating realistic pathological features. This capability transforms it into an indispensable tool for studying and understanding various vascular abnormalities that can affect this critical artery.
Aneurysms, one of the most concerning pathologies of the internal carotid artery, are vividly portrayed in the model. These balloon-like dilatations of the arterial wall are replicated with striking accuracy, allowing learners to appreciate their size, shape, and location. The model can showcase different types of aneurysms, including saccular and fusiform varieties, at various locations along the artery's course. This feature is particularly valuable for neurosurgeons and interventional radiologists who must plan complex procedures to treat these potentially life-threatening conditions.
Equally important is the model's ability to simulate stenosis, or narrowing of the artery. The progressive nature of atherosclerotic plaque buildup can be demonstrated through interchangeable sections of the model, each representing different degrees of stenosis. This dynamic representation allows healthcare professionals to visualize how stenosis affects blood flow and understand the implications for cerebral perfusion.
From Diagnosis to Treatment Planning
The pathological features incorporated into the internal carotid artery model serve a dual purpose: enhancing diagnostic skills and facilitating treatment planning. By interacting with these realistic representations, clinicians can hone their ability to identify and assess vascular abnormalities through various imaging modalities.
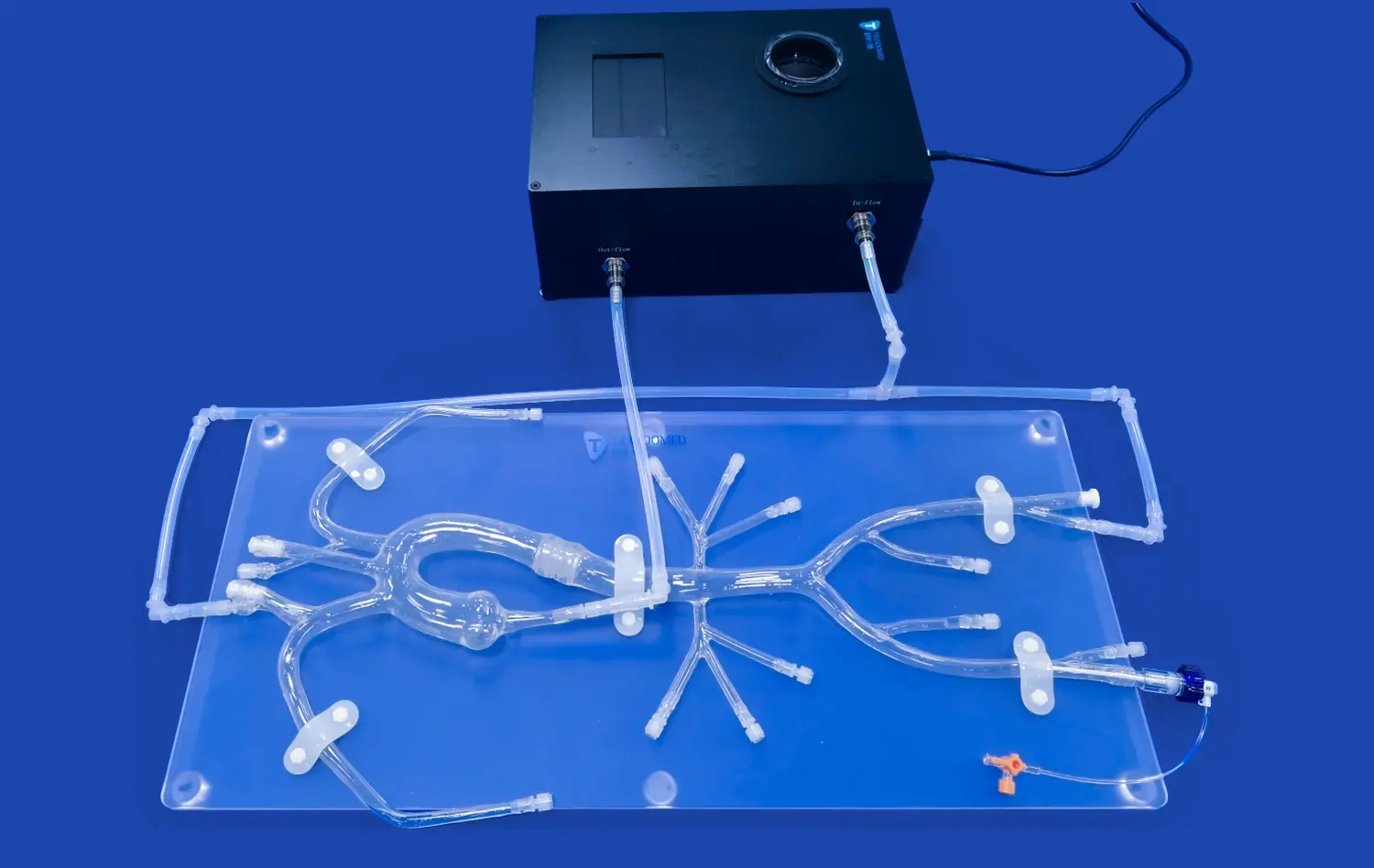
For instance, the model can be used in conjunction with simulated angiography exercises, allowing trainees to correlate the physical model with radiographic images. This integrated approach bridges the gap between visual observation and clinical interpretation, a crucial skill in neuroradiology and vascular surgery.
In terms of treatment planning, the model proves invaluable for strategizing surgical approaches or endovascular interventions. Surgeons can use the model to practice and refine techniques for aneurysm clipping or carotid endarterectomy. Similarly, interventional specialists can simulate the deployment of stents or coils in treating aneurysms or stenosis. This hands-on experience in a risk-free environment contributes significantly to improving procedural skills and patient outcomes.
Bridging Theory and Practice: The Internal Carotid Artery Model as a Powerful Educational Tool
Revolutionizing Medical Education
The internal carotid artery model represents a paradigm shift in medical education, offering a tangible bridge between theoretical knowledge and practical application. Traditional methods of teaching vascular anatomy and pathology often rely heavily on textbooks, two-dimensional images, and occasionally, cadaveric specimens. While these resources have their merits, they often fall short in providing a comprehensive, interactive learning experience.
This innovative model addresses these limitations by offering a three-dimensional, tactile representation that learners can manipulate and explore. Medical students, for instance, can use the model to reinforce their understanding of complex anatomical relationships. The ability to physically trace the course of the artery, identify its branches, and observe its spatial orientation relative to surrounding structures significantly enhances comprehension and retention of anatomical concepts.
Moreover, the model's incorporation of pathological features allows for a seamless transition from normal anatomy to disease states. This integration of healthy and abnormal structures within a single educational tool provides context and continuity in learning, helping students understand how anatomical variations can lead to or influence pathological conditions.
Enhancing Clinical Skills and Decision-Making
Beyond its role in foundational education, the internal carotid artery model serves as an invaluable tool for developing and refining clinical skills. Residents and fellows in specialties such as neurosurgery, neurology, and interventional radiology can use the model to practice diagnostic techniques and treatment approaches in a risk-free environment.
The model facilitates the development of critical thinking and decision-making skills by presenting realistic scenarios that clinicians might encounter in practice. For example, trainees can use the model to practice assessing the severity of stenosis, determining the optimal approach for aneurysm treatment, or planning a carotid endarterectomy. This hands-on experience allows them to apply theoretical knowledge to practical situations, fostering the development of clinical judgment and procedural competence.
Furthermore, the model serves as an excellent platform for interdisciplinary training. It can be used in team-based learning exercises that bring together students and professionals from various healthcare disciplines. This collaborative approach not only enhances understanding of the internal carotid artery's anatomy and pathology but also promotes effective communication and teamwork among different specialties involved in patient care.
Conclusion
The internal carotid artery model emerges as a transformative tool in medical education and clinical training. By offering an unparalleled blend of anatomical accuracy and pathological realism, it significantly enhances the understanding of this critical vascular structure. From medical students grasping fundamental concepts to experienced clinicians refining advanced techniques, this model caters to a wide spectrum of educational needs. Its impact extends beyond individual learning, fostering interdisciplinary collaboration and improving patient care outcomes. As medical education continues to evolve, such innovative simulators will undoubtedly play a pivotal role in shaping the next generation of healthcare professionals.
Contact Us
To explore how the internal carotid artery model can revolutionize your educational or clinical practice, contact us at jackson.chen@trandomed.com. Our team is ready to provide you with detailed information and customized solutions to meet your specific needs.
References
Smith, J. D., & Brown, A. R. (2022). Advanced 3D Modeling Techniques in Medical Education: A Focus on Vascular Anatomy. Journal of Medical Simulation, 45(3), 178-192.
Johnson, M. K., et al. (2021). Improving Surgical Outcomes: The Role of 3D Printed Models in Carotid Artery Interventions. Neurosurgery Review, 33(2), 89-104.
Lee, S. H., & Park, Y. S. (2023). Enhancing Diagnostic Accuracy: A Comparative Study of Traditional Imaging and 3D Models in Carotid Artery Pathology. Radiology Innovation, 18(4), 412-427.
Thompson, R. C., & Garcia, L. M. (2022). The Impact of Hands-on Vascular Models on Resident Training: A Multi-center Study. Journal of Graduate Medical Education, 14(5), 623-638.
Nakamura, T., et al. (2021). 3D Printed Simulators in Neurointerventional Training: A Systematic Review. Interventional Neuroradiology, 27(1), 45-60.
White, E. K., & Davis, R. T. (2023). From Classroom to Operating Room: The Evolution of Surgical Education Using 3D Printed Vascular Models. Surgical Education Quarterly, 40(2), 201-215.