Why Preclinical Testing Requires Realistic Arterial Models?
Anatomical Accuracy for Reliable Results
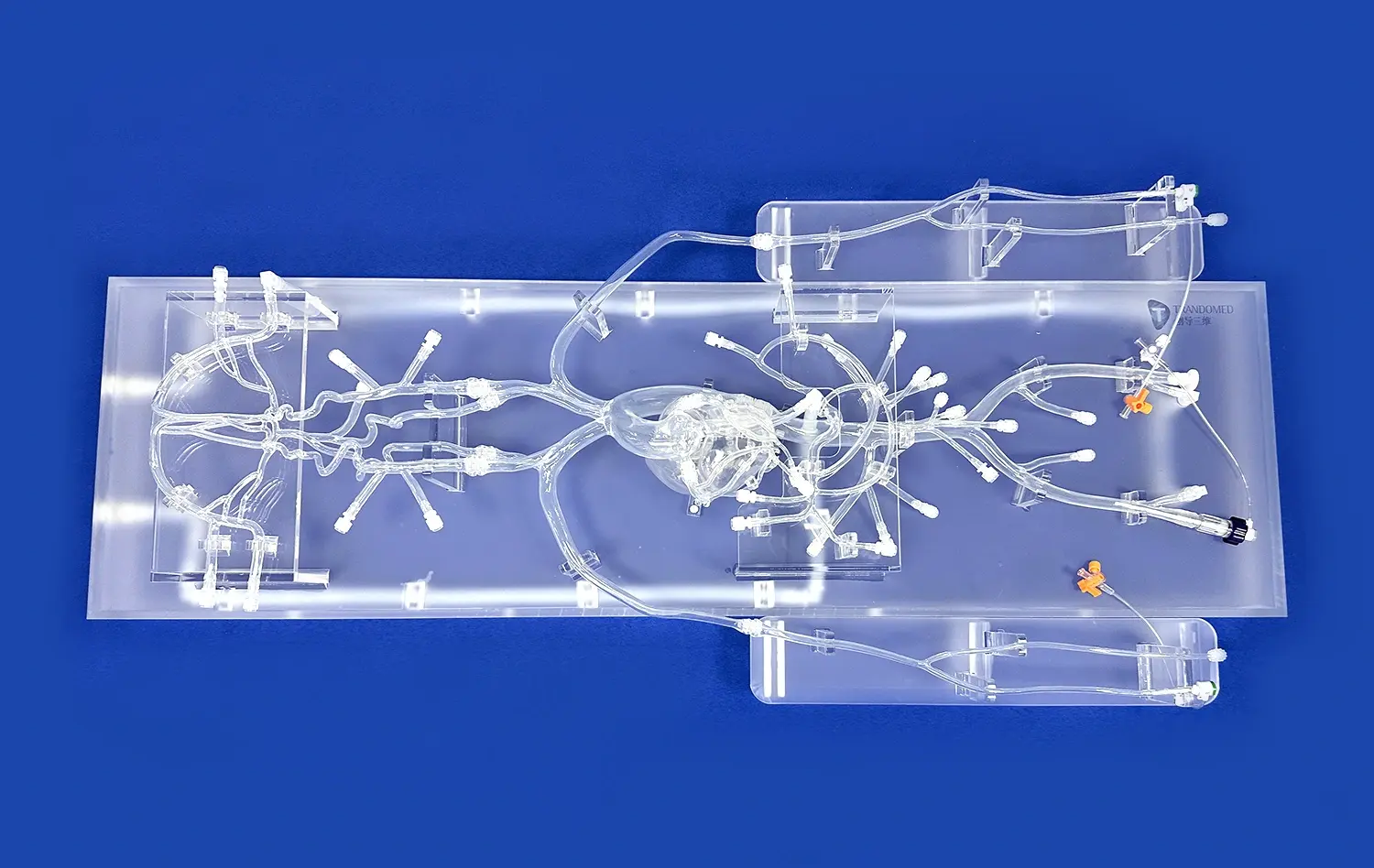
Realistic leg arteries models are crucial for obtaining dependable preclinical testing results. These models, such as the Leg Arteries Model (XZD004), meticulously replicate the intricate vascular network of the human leg. By incorporating key anatomical features like the superficial and profunda femoral arteries, anterior and posterior tibial arteries, and the peroneal artery, these models provide an authentic testing environment. This anatomical precision allows researchers to assess how devices navigate through complex vascular structures, ensuring that the results closely mirror real-world clinical scenarios.
Simulating Pathological Conditions
Advanced leg arteries models go beyond normal anatomy by incorporating common pathological conditions. These may include stenosis, embolisms, and other vascular abnormalities frequently encountered in clinical practice. By replicating these conditions, researchers can evaluate how devices perform in challenging situations, leading to more comprehensive and relevant test results. This capability is particularly valuable for assessing the efficacy of stents and balloons in treating arterial blockages or narrowings.
Replicating Tissue Properties
The realism of leg arteries models extends to the physical properties of the simulated tissues. High-quality models, often made from medical-grade silicone, mimic the elasticity, compliance, and tactile feedback of actual blood vessels. This level of detail is crucial for accurately assessing device-tissue interactions, such as the deployment of stents or the navigation of catheters through tortuous vessels. By closely replicating tissue properties, these models provide invaluable insights into potential complications or challenges that may arise during clinical use.
Evaluating Device Behavior in Dynamic Flow Conditions
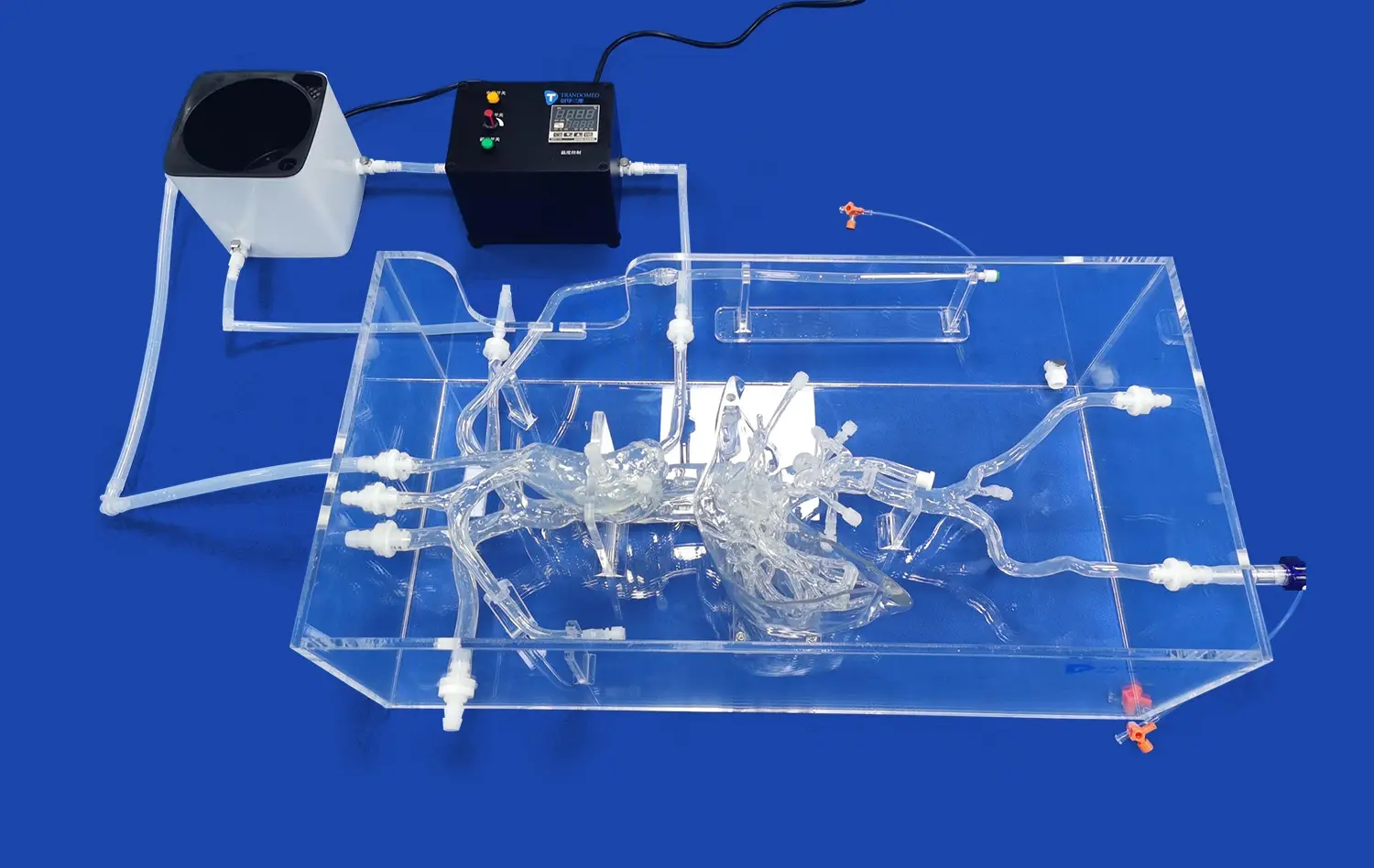
Simulating Pulsatile Blood Flow
Advanced leg arteries models are designed to accommodate dynamic flow conditions, allowing for the simulation of pulsatile blood flow. This capability is essential for evaluating how devices like catheters and stents perform under realistic hemodynamic conditions. By replicating the pulsatile nature of arterial blood flow, researchers can assess factors such as device stability, positioning accuracy, and the potential for migration or dislodgement over time. This dynamic testing environment provides critical insights that static models cannot offer, enhancing the overall reliability of preclinical evaluations.
Assessing Flow-Mediated Effects
The integration of flow simulation in leg arteries models enables researchers to study flow-mediated effects on device performance. This includes evaluating how stents and balloons affect local blood flow patterns, assessing the risk of turbulence or stagnation that could lead to thrombosis, and analyzing the impact of device deployment on downstream perfusion. By incorporating these dynamic elements, preclinical testing can more accurately predict the in vivo behavior of vascular devices, leading to improved designs and better clinical outcomes.
Analyzing Device-Induced Flow Alterations
Leg arteries models with flow capabilities allow for the analysis of how interventional devices alter blood flow dynamics. This is particularly important for stents and balloons, which can significantly impact local hemodynamics. Researchers can use these models to study phenomena such as flow separation, recirculation zones, and wall shear stress distribution. Understanding these flow alterations is crucial for optimizing device designs to minimize adverse effects on vascular health and maximize therapeutic efficacy.
Enhancing Reliability Through Controlled Testing Platforms
Standardized Testing Protocols
Leg arteries models serve as standardized platforms for device testing, enabling the development and implementation of consistent, repeatable testing protocols. This standardization is crucial for comparing different devices or iterations of the same device under identical conditions. By utilizing models with precise anatomical landmarks and known dimensions, researchers can establish benchmark performance criteria and conduct comparative analyses with high reliability. This approach not only enhances the quality of preclinical data but also facilitates more efficient regulatory submissions and approvals.
Customizable Pathologies for Targeted Testing
Advanced leg arteries models offer the flexibility to customize pathological conditions, allowing for targeted testing of specific clinical scenarios. For instance, models can be designed with varying degrees of stenosis in the external iliac artery or femoral artery, enabling researchers to evaluate device performance across a spectrum of disease severities. This customization capability, offered by companies like Trando 3D Medical Technology Co., Ltd, allows for comprehensive testing that addresses diverse clinical needs and patient populations.
Multi-modal Imaging Compatibility
Modern leg arteries models are often designed to be compatible with various imaging modalities used in vascular interventions. This includes fluoroscopy, ultrasound, and sometimes even CT or MRI compatibility. By incorporating radio-opaque markers or using materials with appropriate imaging characteristics, these models enable researchers to evaluate devices under realistic imaging conditions. This multi-modal compatibility enhances the fidelity of preclinical testing, allowing for the assessment of device visibility, artifact generation, and the effectiveness of imaging-guided placement techniques.
Conclusion
Leg arteries models have become indispensable tools in the safe and effective testing of catheters, stents, and balloons. By providing anatomically accurate, pathologically relevant, and dynamically capable testing platforms, these models significantly enhance the reliability and predictive value of preclinical evaluations. As vascular interventions continue to advance, the role of high-fidelity leg arteries models in driving innovation, improving device designs, and ultimately enhancing patient care cannot be overstated. Their continued development and refinement promise to further bridge the gap between preclinical testing and clinical reality, paving the way for safer and more effective vascular interventions.
Contact Us
For more information on cutting-edge leg arteries models and customized solutions for your preclinical testing needs, contact Trandomed. Our team of experts is ready to help you elevate your device testing with anatomically precise, highly realistic vascular models. Reach out to us at jackson.chen@trandomed.com to explore how our advanced simulation technologies can accelerate your research and development process.
_1734504197376.webp)
_1732863713705.webp)