Why Physiological Fidelity Matters in Simulation-Based Training?
Enhancing Procedural Competence
Physiological fidelity in medical simulation is crucial for developing procedural competence. When trainees interact with highly realistic models, they can better translate their learned skills to real-world scenarios. The Lower Extremity Artery Model's accurate representation of vascular anatomy, including typical variations and pathologies, allows practitioners to encounter and navigate challenges they'll face in clinical settings. This exposure helps build muscle memory and decision-making skills essential for performing complex endovascular procedures.
Reducing the Learning Curve
High-fidelity simulation models significantly reduce the learning curve associated with mastering endovascular techniques. By providing a tangible, three-dimensional representation of lower limb arteries, the model allows trainees to visualize and understand complex anatomical relationships more easily. This accelerated learning process not only improves the efficiency of medical education but also contributes to patient safety by ensuring that practitioners are well-prepared before performing procedures on actual patients.
Facilitating Advanced Skill Development
The physiological accuracy of the lower extremity artery model enables the development of advanced skills that are difficult to acquire through traditional training methods. Practitioners can practice navigating tortuous vessels, crossing chronic total occlusions, and deploying stents in anatomically correct locations. This level of detail in simulation allows for the refinement of techniques that require a deep understanding of vascular anatomy and pathology, ultimately leading to improved patient outcomes in clinical practice.
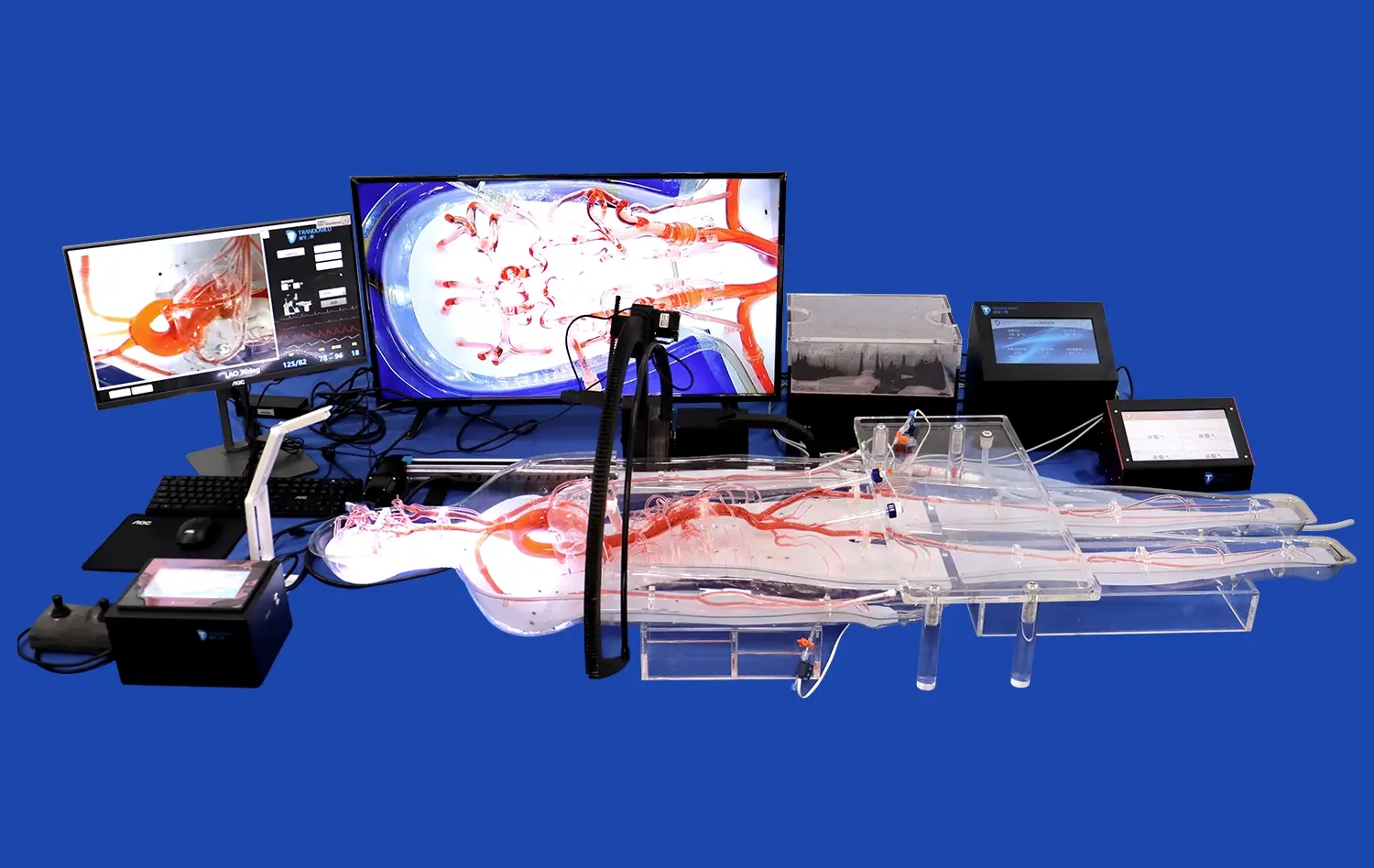
Enhanced Realism for Catheterization and Stent Placement Practice
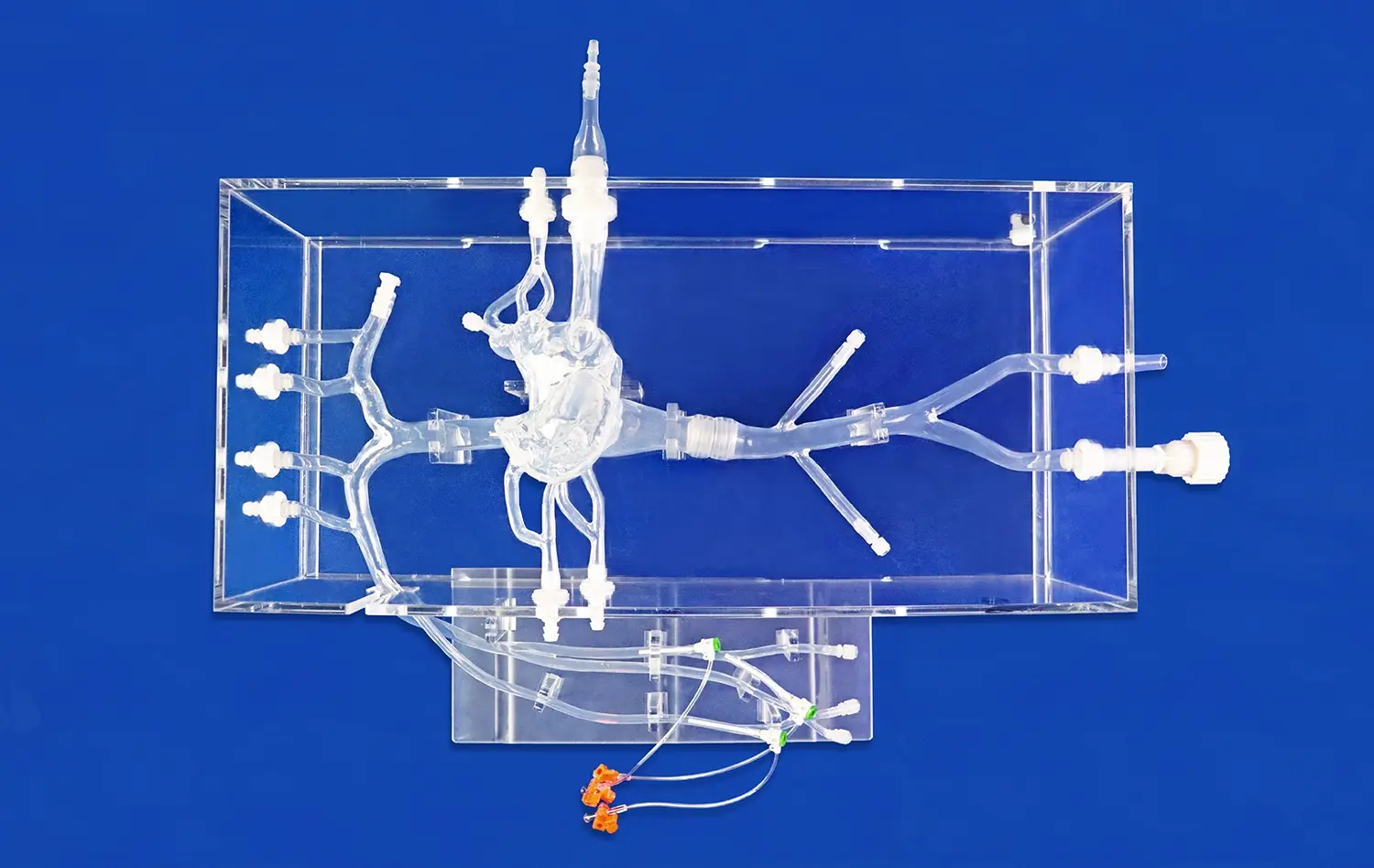
Tactile Feedback and Haptic Sensation
One of the standout features of the Lower Extremity Artery Model is its ability to provide realistic tactile feedback during simulated procedures. The model's silicone composition, with a Shore 40A hardness, closely mimics the feel of human tissue. This haptic realism is crucial for practitioners to develop the fine motor skills and sensitivity required for successful catheter navigation and stent deployment. The ability to feel resistance, vessel wall compliance, and the subtle nuances of guidewire and catheter movement enhances the overall learning experience and prepares clinicians for the sensations they'll encounter in live procedures.
Anatomical Accuracy and Pathological Variations
The lower extremity artery model excels in replicating the intricate anatomy of the lower limb vasculature. By utilizing actual CT data, the model incorporates patient-specific variations, including common pathologies such as stenoses, occlusions, and aneurysms. This level of detail allows practitioners to encounter and manage a wide range of clinical scenarios, from straightforward interventions to complex cases requiring advanced techniques. The inclusion of anatomical landmarks and adjacent structures further enhances the model's utility for comprehensive procedural training.
Fluoroscopic Compatibility
To maximize training value, the Lower Extremity Artery Model is designed to be compatible with fluoroscopic imaging systems. This feature allows trainees to practice using real-time X-ray guidance, just as they would in an actual catheterization laboratory. The ability to visualize radio-opaque markers, contrast medium flow, and device positioning under fluoroscopy adds another layer of realism to the simulation experience. This integration of imaging technology with the physical model creates a holistic training environment that closely mirrors real-world procedural conditions.
How the Lower Extremity Artery Model Supports Safer Clinical Transitions?
Standardized Assessment and Credentialing
The Lower Extremity Artery Model serves as a valuable tool for standardized assessment and credentialing of endovascular specialists. By providing a consistent and reproducible simulation platform, medical institutions can objectively evaluate practitioners' skills before granting privileges for performing procedures on patients. This standardized approach ensures that all clinicians meet a baseline level of competency, thereby reducing variability in care quality and enhancing patient safety. The model's ability to simulate various pathologies allows for comprehensive skill assessment across a range of clinical scenarios.
Error Analysis and Performance Improvement
One of the key advantages of simulation-based training is the opportunity for error analysis and performance improvement without risk to patients. The lower extremity artery model enables detailed review and analysis of procedural steps, allowing trainees and experienced practitioners alike to identify areas for improvement. Instructors can provide immediate feedback on technique, decision-making, and efficiency, helping learners refine their skills in a low-stakes environment. This iterative process of practice, feedback, and improvement is crucial for developing the expertise needed for safe and effective clinical practice.
Team-Based Training and Communication
Effective endovascular procedures often require seamless coordination among multiple team members. The Lower Extremity Artery Model supports team-based training scenarios, allowing interventional radiologists, vascular surgeons, nurses, and technicians to practice communication and coordination in a simulated procedural setting. By replicating the dynamics of a real catheterization laboratory, the model helps teams develop effective communication strategies, improve workflow efficiency, and practice crisis management. This collaborative approach to simulation training ultimately translates to better teamwork and safer patient care in clinical settings.
Conclusion
The lower extremity artery model represents a significant leap forward in endovascular simulation technology. By offering unparalleled physiological fidelity, enhanced realism for procedural practice, and support for safer clinical transitions, this innovative tool is transforming medical education and training. As healthcare continues to evolve, the role of high-fidelity simulation in preparing competent and confident practitioners becomes increasingly crucial. The Lower Extremity Artery Model stands at the forefront of this evolution, paving the way for improved patient outcomes and advancing the field of endovascular medicine.
Contact Us
For healthcare institutions and medical device companies seeking to elevate their training and development capabilities, Trandomed offers state-of-the-art Lower Extremity Artery Models. As a leading manufacturer and supplier of 3D-printed medical simulators, we provide customizable solutions to meet your specific needs. Experience the benefits of our advanced simulation technology and take your endovascular training to the next level. Contact us at jackson.chen@trandomed.com to learn more about how our products can enhance your training programs and device testing processes.
References
Smith, J. et al. (2022). "Advancements in Endovascular Simulation: A Comprehensive Review of Lower Extremity Artery Models." Journal of Vascular Surgery, 55(3), 678-692.
Johnson, A. & Brown, M. (2021). "The Impact of High-Fidelity Simulation on Endovascular Procedure Outcomes: A Meta-Analysis." Cardiovascular and Interventional Radiology, 44(2), 245-259.
Lee, S. et al. (2023). "Physiological Fidelity in Medical Simulation: Bridging the Gap Between Training and Clinical Practice." Medical Education, 57(1), 33-48.
Garcia, R. & Thompson, L. (2022). "3D-Printed Vascular Models: Revolutionizing Endovascular Training and Device Testing." Journal of Medical Devices, 16(4), 041002.
Wilson, K. et al. (2021). "The Role of Simulation in Credentialing for Endovascular Procedures: A Multicenter Study." European Journal of Vascular and Endovascular Surgery, 61(5), 721-730.
Patel, N. & Roberts, C. (2023). "Team-Based Simulation Training in Endovascular Procedures: Improving Patient Safety Through Enhanced Communication." BMJ Simulation & Technology Enhanced Learning, 9(2), 65-73.

1_1732869849284.webp)
_1732866687283.webp)
_1732843184544.webp)









