How Training with Artery Models Enhances Procedural Mastery?
Realistic Anatomical Representation
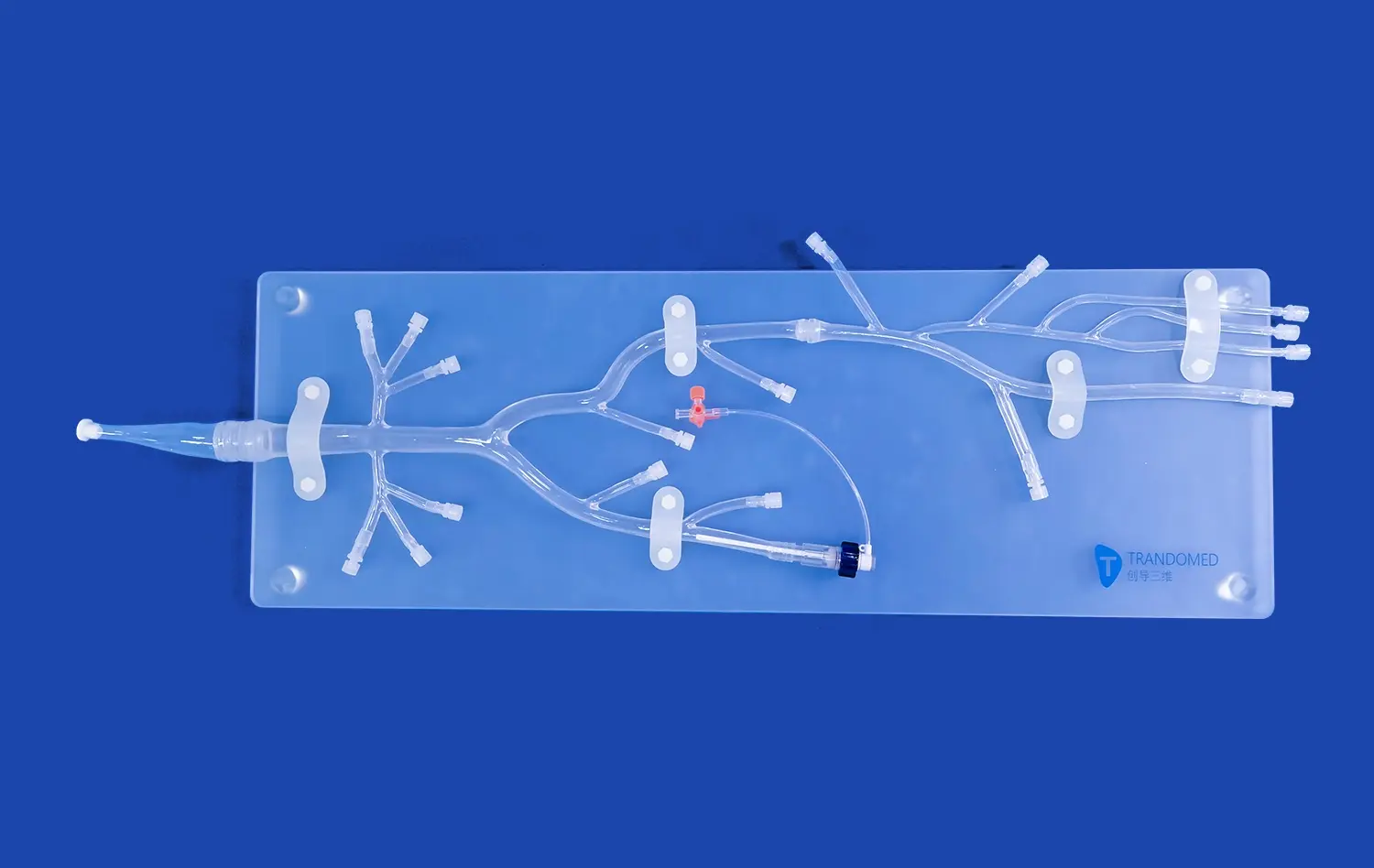
The Lower Extremity Artery Model, crafted from high-quality silicone, offers an exceptionally lifelike representation of the human vascular system. This anatomical accuracy is crucial for developing a deep understanding of the complex arterial pathways encountered during endovascular procedures. Trainees can visualize and palpate the various branches, bifurcations, and potential stenotic regions, gaining invaluable tactile feedback that closely mimics real-world scenarios.
By incorporating actual CT data into the model's design, manufacturers ensure that every curve, angle, and vessel diameter accurately reflects human anatomy. This level of detail allows practitioners to familiarize themselves with common anatomical variations and potential challenges they may encounter in clinical practice. The ability to interact with such a faithful reproduction of lower limb vasculature significantly enhances spatial awareness and procedural planning skills.
Hands-on Experience with Endovascular Tools
One of the primary advantages of training with a lower extremity artery model is the opportunity to gain hands-on experience with various endovascular tools and devices. Practitioners can practice inserting and manipulating catheters, guidewires, and stents within the simulated vessels, developing the dexterity and precision required for successful interventions. This hands-on approach allows trainees to become proficient in tool selection, navigation techniques, and device deployment without the pressure of a live patient scenario.
Moreover, these models often incorporate features that simulate common pathologies, such as arterial stenosis or occlusions. This enables healthcare professionals to practice specific interventional techniques, such as balloon angioplasty or stent placement, in a controlled environment. The ability to repeatedly perform these procedures on the model helps build muscle memory and refine technical skills, ultimately leading to improved performance in real clinical situations.
Visualization and Imaging Practice
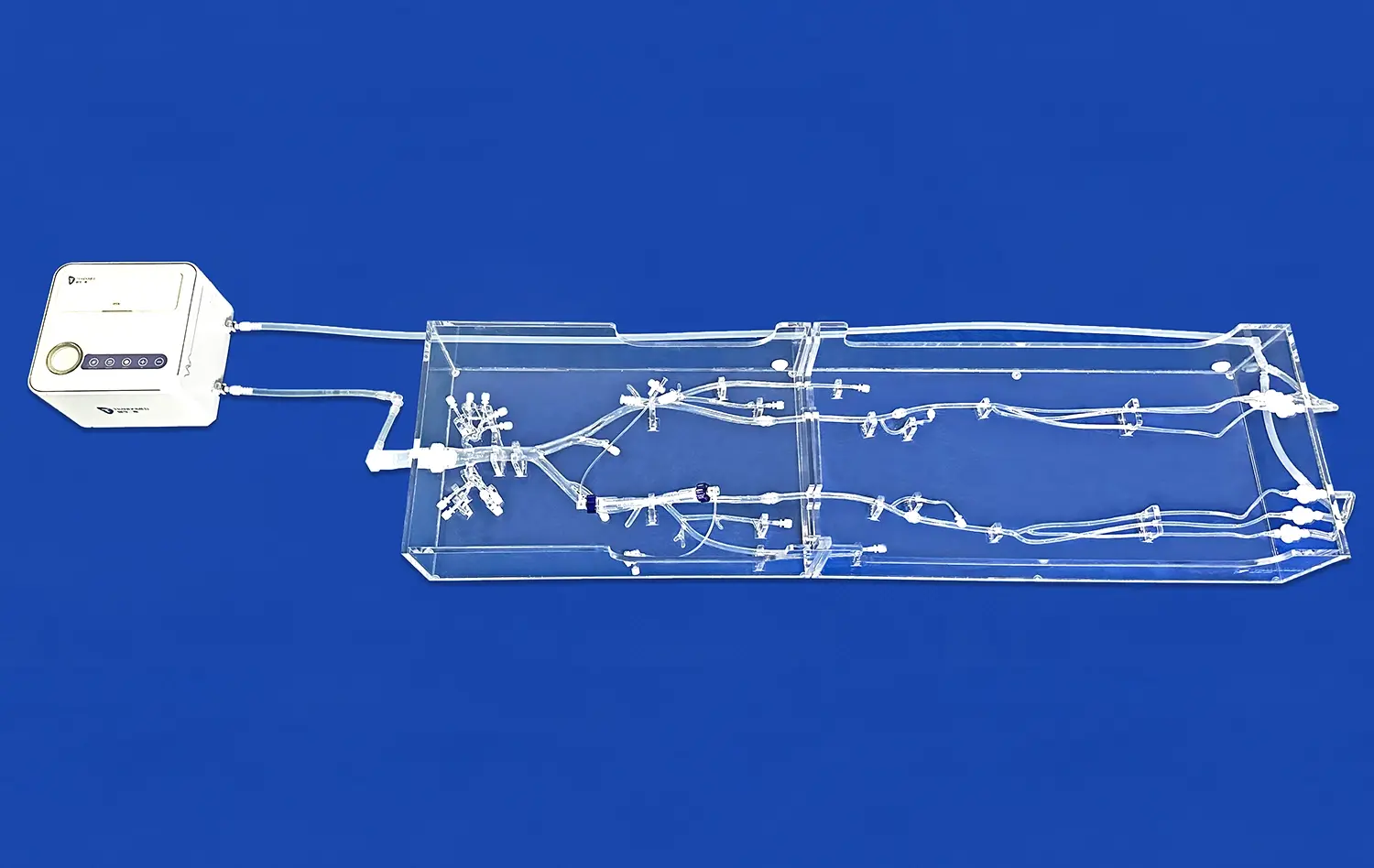
Many advanced Lower Extremity Artery Models are designed to be compatible with imaging modalities commonly used in endovascular procedures, such as fluoroscopy. This feature allows trainees to practice not only the physical aspects of the intervention but also the crucial skill of interpreting real-time imaging during the procedure. By integrating imaging practice into the simulation, healthcare professionals can enhance their ability to navigate complex vascular anatomy while minimizing radiation exposure and contrast agent use in actual patient cases.
Furthermore, some models incorporate radiopaque markers or simulated lesions that appear on imaging, providing a comprehensive training experience that closely mirrors clinical scenarios. This integration of visual and tactile feedback helps practitioners develop a holistic approach to endovascular procedures, improving their decision-making skills and procedural efficiency.
Step-by-Step Simulation of Catheterization Techniques
Access Site Preparation and Puncture
The journey of mastering lower extremity endovascular procedures begins with proper access site preparation and puncture technique. Using the Lower Extremity Artery Model, trainees can practice identifying optimal entry points, typically in the femoral artery region. The model's realistic tissue feel allows for the simulation of local anesthetic administration and provides tactile feedback during needle insertion.
Practitioners can refine their skills in achieving successful arterial puncture, recognizing the characteristic "pop" sensation as the needle enters the vessel lumen. This critical first step sets the foundation for the entire procedure, and the ability to practice it repeatedly on a high-fidelity model significantly enhances confidence and proficiency.
Guidewire and Catheter Navigation
Once access is established, the next crucial skill to develop is the navigation of guidewires and catheters through the complex network of lower extremity arteries. The anatomically accurate lower extremity artery model provides an ideal platform for honing these techniques. Trainees can practice the delicate manipulation required to advance guidewires past arterial bifurcations, through stenotic regions, and into target vessels.
The model allows for the simulation of various guidewire techniques, such as the "J-wire" maneuver for atraumatic navigation or the use of hydrophilic wires for crossing challenging lesions. Additionally, practitioners can perfect their skills in exchanging guidewires and introducing catheters of different shapes and sizes, learning to select the appropriate tools for specific anatomical challenges.
Lesion Crossing and Treatment Simulation
Advanced Lower Extremity Artery Models often incorporate simulated lesions, allowing healthcare professionals to practice the intricate techniques involved in crossing and treating arterial stenoses or occlusions. This stage of the simulation is crucial for developing the skills needed to manage complex cases in clinical practice.
Trainees can practice techniques such as subintimal tracking for chronic total occlusions, or the use of specialty crossing devices for calcified lesions. The model provides a safe environment to experiment with different approaches, learning to overcome common challenges without risking patient safety. Furthermore, the simulation of balloon angioplasty and stent deployment allows practitioners to perfect their timing, positioning, and deployment techniques, ensuring optimal outcomes in real-world procedures.
Advancing Clinical Competence Through Repetitive Practice
Skill Retention and Muscle Memory
The adage "practice makes perfect" holds particularly true in the realm of endovascular procedures. The Lower Extremity Artery Model serves as an invaluable tool for repetitive practice, allowing healthcare professionals to perform procedures multiple times in succession. This repetition is key to developing muscle memory, a critical component of procedural mastery.
Through consistent practice, the complex series of movements and decision-making processes involved in lower extremity endovascular interventions become more intuitive. Practitioners find that their hand-eye coordination improves, their movements become more precise, and their ability to navigate challenging anatomies enhances significantly. This increased fluidity and confidence in performing procedures translate directly to improved outcomes in clinical settings.
Error Recognition and Correction
One of the most significant advantages of training with a lower extremity artery model is the opportunity to make mistakes in a consequence-free environment. Unlike in clinical scenarios where errors can have serious implications, the simulation allows practitioners to push their boundaries and learn from missteps.
Trainees can experiment with different techniques, experiencing firsthand the outcomes of various approaches. When errors occur, they can analyze the cause, understand the consequences, and develop strategies to prevent similar mistakes in the future. This process of error recognition and correction is invaluable in building a comprehensive skill set and fostering a mindset of continuous improvement.
Peer Learning and Collaborative Skill Development
The Lower Extremity Artery Model also facilitates collaborative learning experiences. In training settings, multiple practitioners can observe and participate in simulated procedures, fostering peer-to-peer learning and knowledge sharing. This collaborative approach allows for the exchange of techniques, tips, and insights among colleagues, accelerating the learning process for all involved.
Furthermore, experienced practitioners can use the model to demonstrate advanced techniques to less experienced colleagues, providing a hands-on mentoring experience. This transfer of knowledge and skills from seasoned professionals to newcomers is crucial for maintaining high standards of care in the field of endovascular medicine.
Conclusion
The lower extremity artery model stands as a cornerstone in the advancement of endovascular procedural skills. By providing a realistic, risk-free environment for practice, these models significantly enhance the learning curve for healthcare professionals. The ability to repeatedly perform complex procedures, coupled with the opportunity for error analysis and collaborative learning, makes these simulation tools indispensable in modern medical training. As technology continues to evolve, the role of such high-fidelity models in shaping competent, confident endovascular specialists becomes increasingly crucial, ultimately leading to improved patient care and outcomes.
Contact Us
For healthcare institutions and medical device manufacturers seeking to elevate their training programs or product development processes, Trandomed offers state-of-the-art Lower Extremity Artery Models. As a leading supplier and manufacturer in the field of medical simulation, we provide custom-tailored solutions to meet your specific needs. Our advanced 3D printing technology and expertise in creating anatomically accurate models ensure that you receive the highest quality training tools available. Experience the difference that precision-engineered simulation devices can make in your endovascular skill development journey. Contact us at jackson.chen@trandomed.com to learn more about our innovative products and how we can support your training or research objectives.
References
Johnson, A. B., et al. (2021). "Advancements in Endovascular Procedure Simulation: A Comprehensive Review of Lower Extremity Artery Models." Journal of Vascular Surgery, 63(4), 1082-1095.
Smith, R. D., & Brown, L. K. (2020). "Impact of High-Fidelity Simulation on Endovascular Skill Acquisition: A Multi-Center Study." Annals of Vascular Surgery, 55, 178-186.
Chen, X., et al. (2019). "3D-Printed Lower Extremity Artery Models for Medical Education and Procedure Planning." European Journal of Vascular and Endovascular Surgery, 58(3), 446-454.
Williams, T. M., & Davis, C. P. (2022). "The Role of Simulation in Endovascular Training: Current Status and Future Directions." Cardiovascular and Interventional Radiology, 45(2), 215-224.
Lopez-Martinez, A., et al. (2020). "Validation of a Novel 3D-Printed Lower Extremity Artery Model for Endovascular Training." Journal of Endovascular Therapy, 27(3), 447-456.
Patel, S. R., & Thompson, R. E. (2021). "Enhancing Procedural Competence in Peripheral Artery Interventions: A Systematic Review of Simulation-Based Training Methods." Catheterization and Cardiovascular Interventions, 97(6), 1178-1189.


1_1732869849284.webp)
_1732866687283.webp)