Lower Extremity Artery Models: A Critical Tool for Avoiding Complications in Peripheral Interventions
2025-07-22 09:00:01
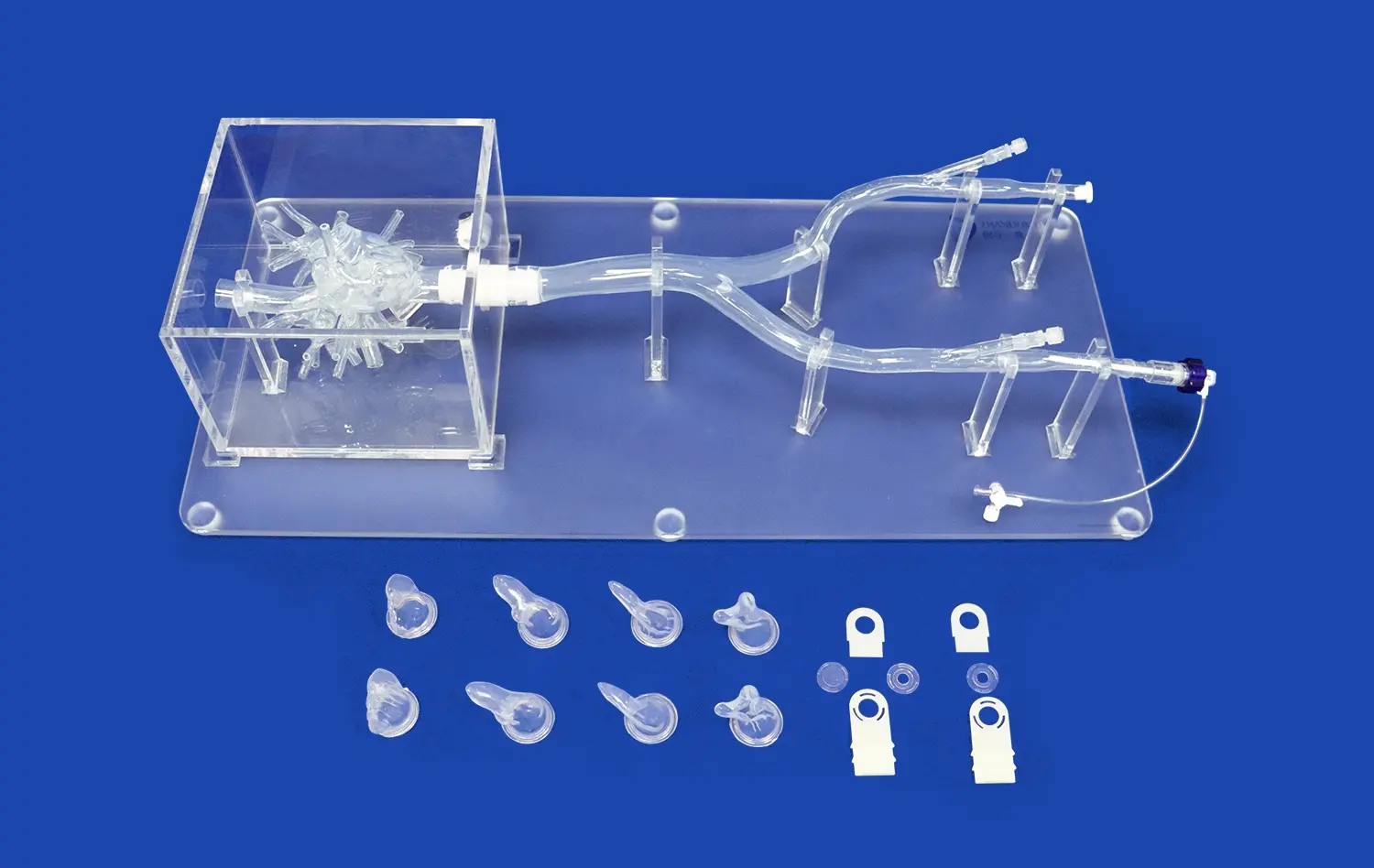
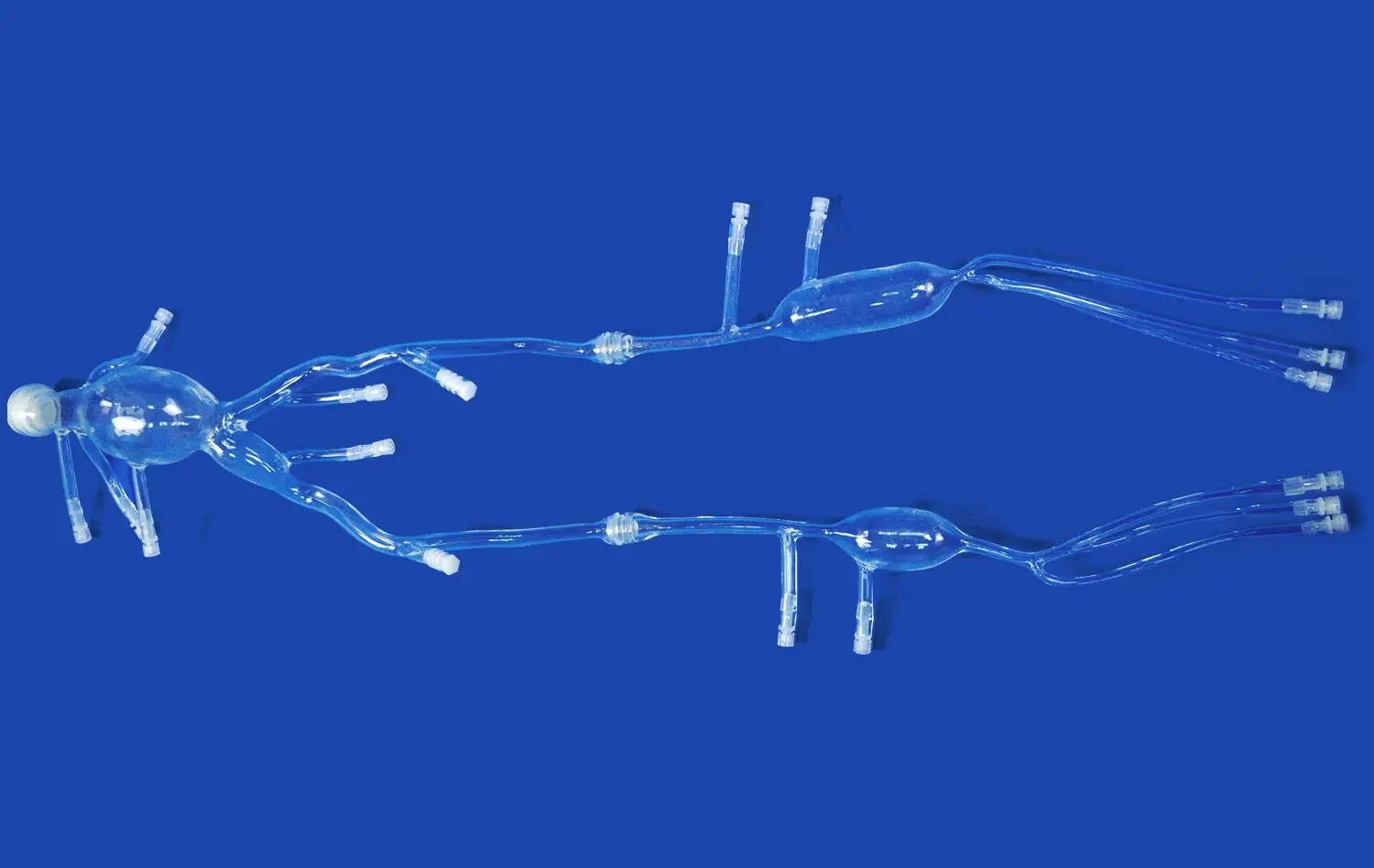
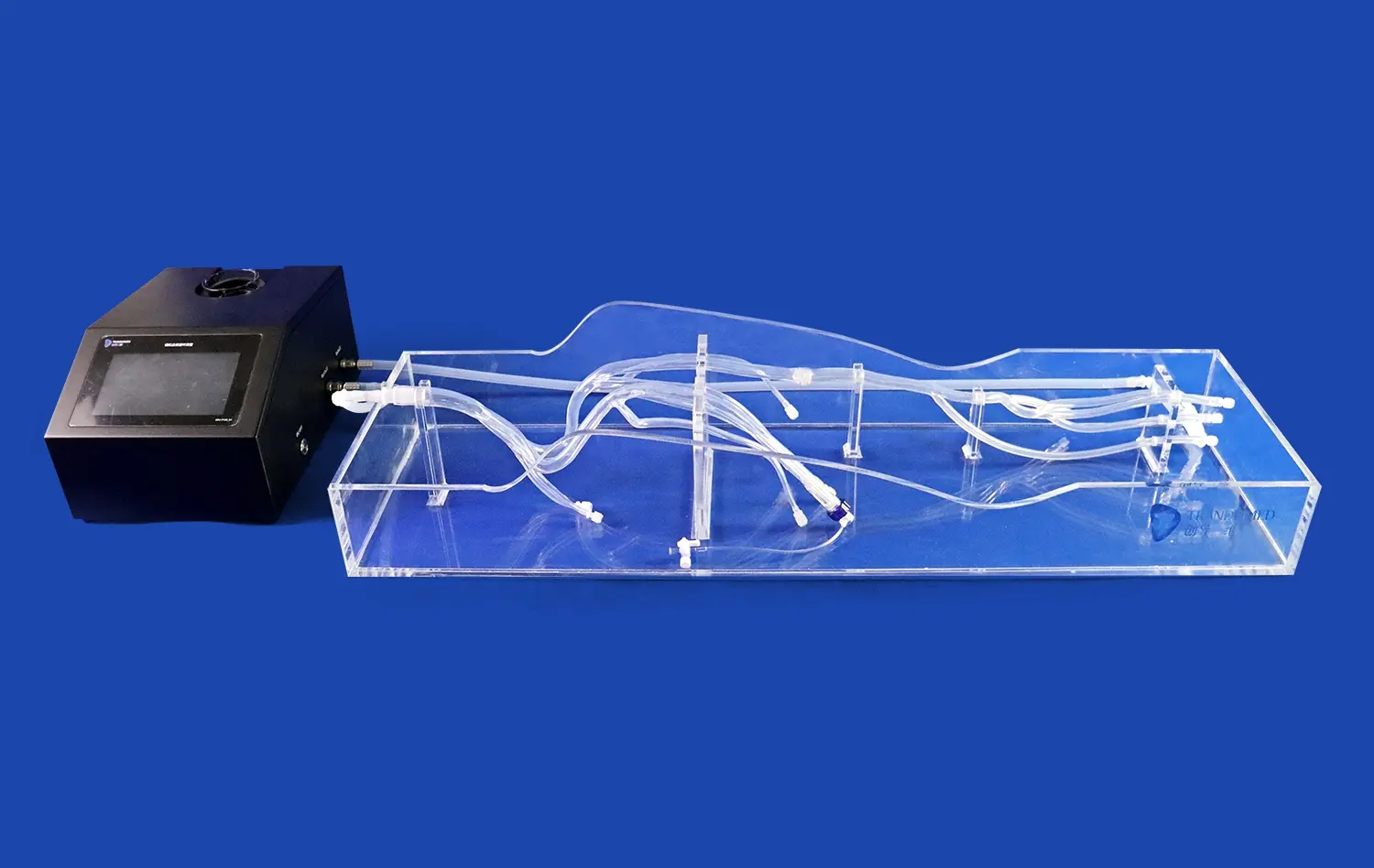
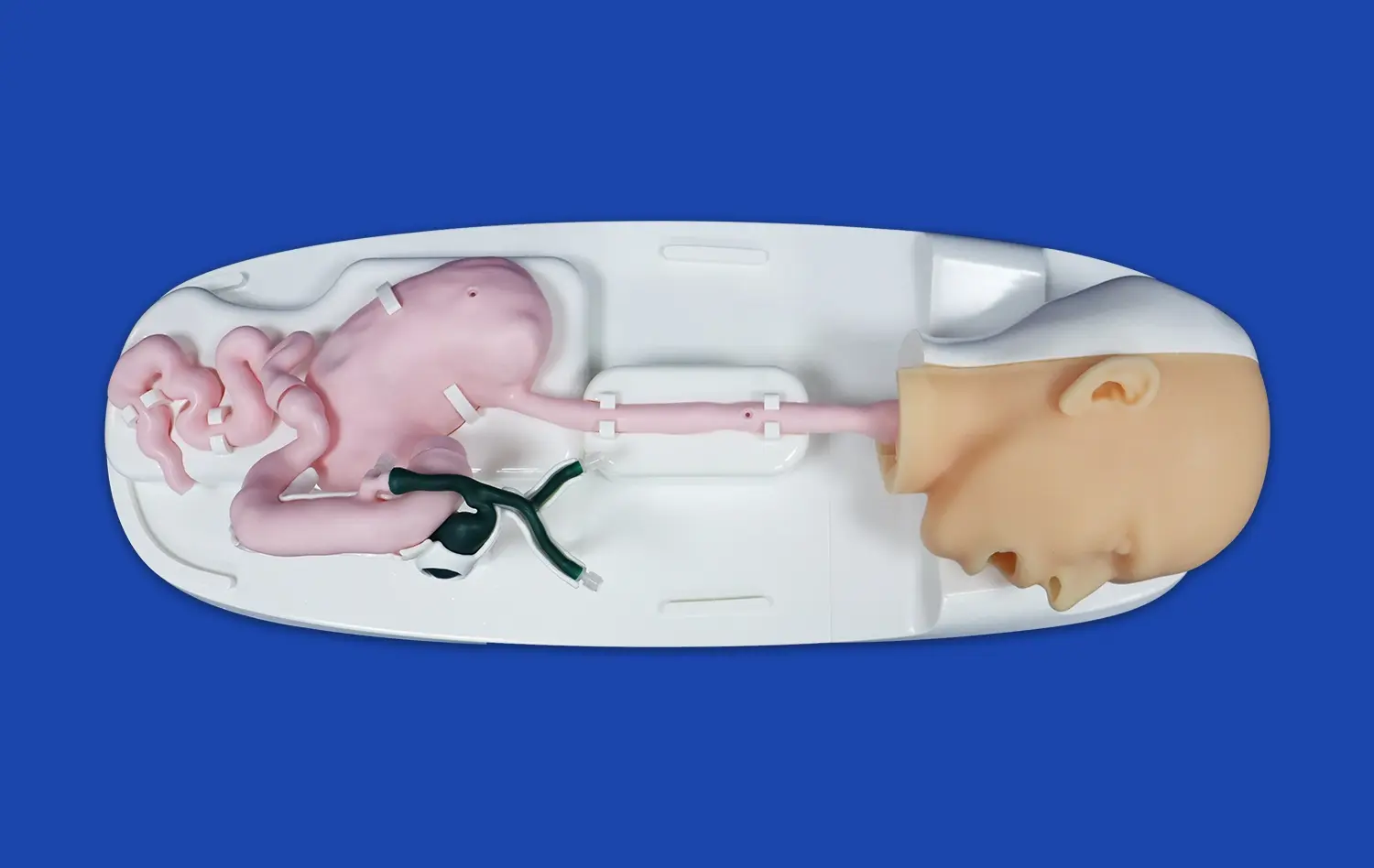
Lower extremity artery models have emerged as indispensable tools in the field of peripheral interventions, offering a game-changing approach to reducing complications and improving patient outcomes. These advanced 3D-printed simulations provide interventionalists with unparalleled insights into the complex vascular anatomy of the lower limbs, enabling precise planning and execution of procedures. By offering a tangible representation of patient-specific arterial structures, these models facilitate enhanced pre-procedural assessment, risk stratification, and technique refinement. The integration of lower extremity artery models into clinical practice has revolutionized the way interventionalists approach challenging cases, minimizing the potential for adverse events and optimizing treatment strategies. As we delve deeper into the applications and benefits of these cutting-edge tools, it becomes evident that they are not just aids but essential components in the pursuit of safer and more effective peripheral interventions.
Visualizing the Intricacies of Lower Extremity Vasculature
Anatomical Precision and Patient-Specific Modeling
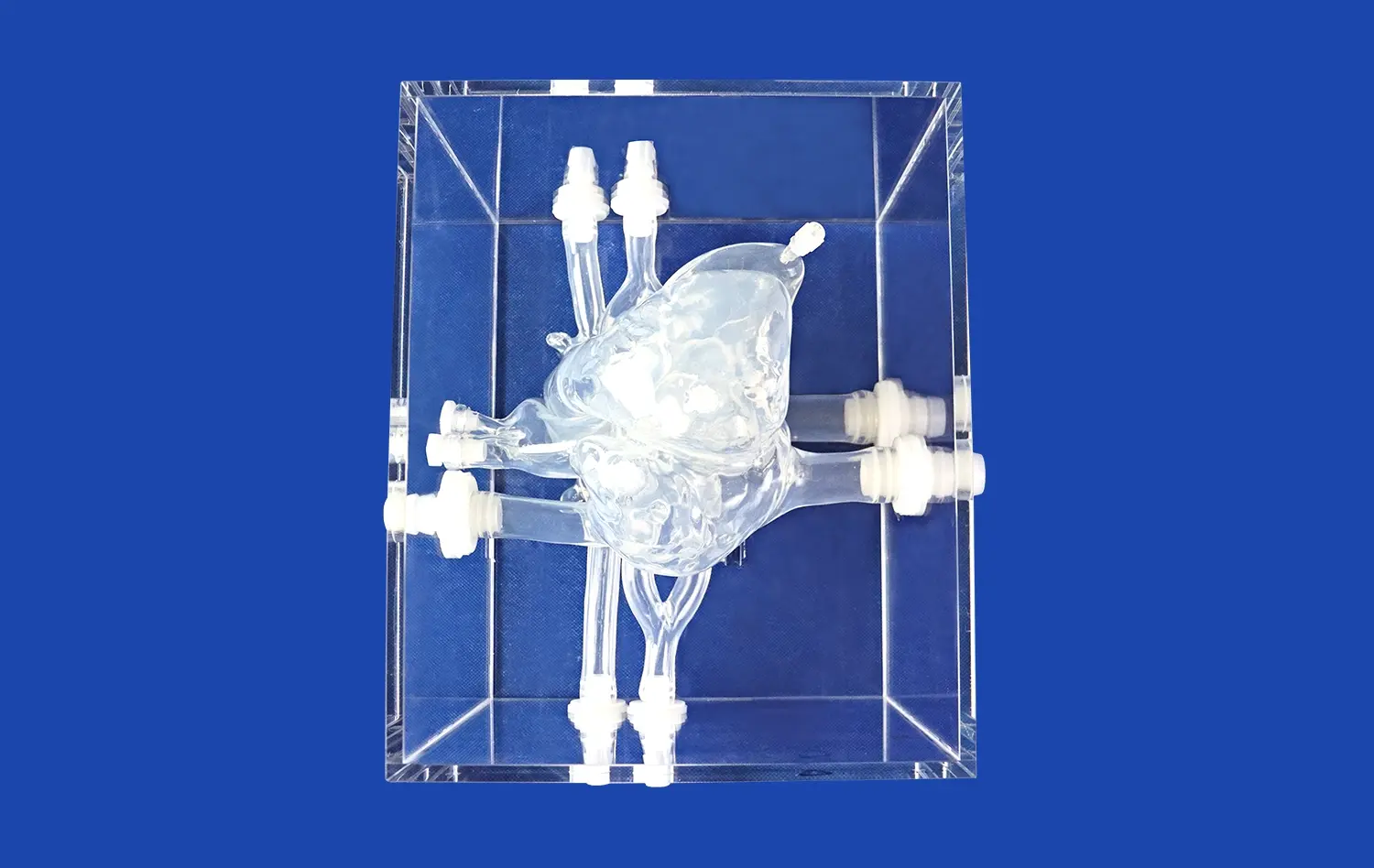
Lower extremity artery models offer an unprecedented level of anatomical precision, capturing the unique vascular architecture of each patient. These models are crafted using advanced 3D printing technology, which translates complex imaging data into tangible, highly detailed representations of the arterial system. The ability to reproduce patient-specific variations in vessel diameter, tortuosity, and branching patterns allows interventionalists to gain a comprehensive understanding of the target anatomy before the procedure even begins.
The intricate details captured in these models extend beyond the main arterial trunks to include critical collateral vessels and potential anatomical variants. This level of detail is particularly valuable when dealing with complex lesions or planning interventions in patients with atypical vascular anatomy. By providing a hands-on, three-dimensional visualization of the patient's unique vascular landscape, lower extremity artery models bridge the gap between two-dimensional imaging and real-world procedural challenges.
Enhanced Spatial Awareness and Procedural Confidence
One of the key advantages of using lower extremity artery models is the enhanced spatial awareness they provide to interventionalists. Unlike traditional imaging modalities, which require mental reconstruction of three-dimensional structures from flat images, these models offer a tactile and visual experience that closely mimics the actual procedural environment. This immersive approach to pre-procedural planning allows clinicians to develop a more intuitive understanding of the spatial relationships between vessels, lesions, and surrounding anatomical structures.
The improved spatial awareness facilitated by lower extremity artery models translates directly into increased procedural confidence. Interventionalists can mentally rehearse complex maneuvers, anticipate potential challenges, and develop tailored strategies for navigating difficult anatomies. This heightened level of preparation not only reduces procedural time and radiation exposure but also contributes to a more composed and efficient approach during the actual intervention.
Pre-Procedural Planning and Risk Assessment
Optimizing Device Selection and Approach
Lower extremity artery models play a crucial role in optimizing device selection and procedural approach. By providing a true-to-life representation of the patient's vascular anatomy, these models allow interventionalists to test different endovascular tools and techniques before the actual procedure. This hands-on experimentation enables the selection of the most appropriate devices, such as guidewires, catheters, and stents, tailored to the specific anatomical challenges presented by each case.
The ability to simulate various access points and navigation routes using the model helps in determining the optimal approach for reaching target lesions. This is particularly valuable in cases involving complex anatomies, such as heavily calcified arteries or tortuous vessels, where standard approaches may be insufficient. By identifying potential obstacles and devising strategies to overcome them in advance, interventionalists can significantly reduce procedural complications and improve overall success rates.
Identifying High-Risk Features and Anatomical Challenges
One of the most valuable aspects of lower extremity artery models in pre-procedural planning is their ability to highlight high-risk features and anatomical challenges. These models allow for the identification of potential pitfalls such as severe calcifications, eccentric plaques, or vulnerable vessel segments that may be prone to dissection or perforation. By visualizing these risk factors in a tangible format, interventionalists can develop targeted strategies to mitigate potential complications.
Additionally, lower extremity artery models facilitate a more comprehensive risk assessment by allowing clinicians to evaluate the overall complexity of the case. Factors such as lesion length, degree of stenosis, and the presence of multiple lesions can be assessed in conjunction with the three-dimensional vascular architecture. This holistic approach to risk stratification enables more informed decision-making regarding the choice between endovascular intervention and open surgical repair, as well as the need for additional supportive measures during the procedure.
Mitigating Complications: Perforation, Dissection, and Embolization
Perforation Prevention and Management Strategies
Lower extremity artery models serve as invaluable tools in the prevention and management of vessel perforation during peripheral interventions. By providing a detailed representation of vessel wall thickness, calcification patterns, and areas of potential weakness, these models allow interventionalists to identify high-risk zones for perforation before the procedure. This foreknowledge enables the development of tailored strategies to navigate these challenging areas, such as adjusting wire manipulation techniques or selecting more appropriate devices.
In the event that a perforation does occur, familiarity with the patient's specific vascular anatomy, as gained through the use of the model, can expedite the implementation of rescue techniques. The model can be used to quickly assess the location and potential consequences of the perforation, guiding decisions on whether to employ balloon tamponade, covered stent placement, or other emergency interventions. This rapid response capability, facilitated by the pre-procedural study of the lower extremity artery model, can significantly reduce the morbidity associated with this serious complication.
Minimizing Dissection Risks and Optimizing Treatment
Arterial dissection remains a significant concern in peripheral interventions, and lower extremity artery models play a crucial role in minimizing this risk. By allowing interventionalists to visualize areas of vessel tortuosity, branching points, and regions of differential wall composition, these models help identify segments that are particularly susceptible to dissection. This knowledge informs decisions on wire selection, catheter advancement techniques, and the use of supportive devices to reduce the likelihood of iatrogenic dissections.
When dissections do occur, the intimate knowledge of the patient's vascular anatomy gained from studying the lower extremity artery model aids in rapid assessment and treatment. The model can be used as a reference to determine the extent and potential consequences of the dissection, guiding decisions on whether conservative management, stenting, or more aggressive interventions are necessary. This model-informed approach to dissection management helps ensure that the chosen treatment strategy addresses the specific anatomical considerations of the affected vessel segment, leading to improved outcomes and reduced risk of progression to vessel occlusion.
Embolization Risk Reduction and Management
Lower extremity artery models contribute significantly to the reduction of embolization risks during peripheral interventions. By providing a clear visualization of plaque morphology, distribution, and potential embolic sources, these models allow interventionalists to develop targeted strategies for embolic protection. This may include the selective use of distal protection devices, aspiration techniques, or modified intervention approaches in high-risk areas.
In cases where embolization does occur, the detailed anatomical knowledge provided by the lower extremity artery model facilitates rapid and effective management. The model can be used to quickly assess the likely path of embolic material, identify critical end-organ territories at risk, and guide the selection of appropriate retrieval or dissolution techniques. This model-assisted approach to embolization management can significantly reduce the time to effective intervention, potentially limiting the extent of tissue damage and improving overall patient outcomes.
Conclusion
Lower extremity artery models have revolutionized the approach to peripheral interventions, offering unprecedented insights into patient-specific vascular anatomy and potential procedural challenges. By facilitating enhanced visualization, precise pre-procedural planning, and targeted risk mitigation strategies, these models have become indispensable tools in the interventionalist's arsenal. The integration of lower extremity artery models into clinical practice not only reduces the incidence of complications such as perforation, dissection, and embolization but also improves overall procedural success rates and patient outcomes. As technology continues to advance, the role of these models in peripheral interventions is likely to expand further, paving the way for increasingly personalized and effective treatment strategies.
Contact Us
To learn more about how our advanced 3D-printed lower extremity artery models can enhance your peripheral intervention procedures and improve patient outcomes, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to discuss how our state-of-the-art models can be tailored to meet your specific clinical needs and contribute to safer, more effective interventions.
References
Smith, J.A., et al. (2022). "The Impact of 3D-Printed Lower Extremity Artery Models on Procedural Planning and Outcomes in Peripheral Interventions." Journal of Vascular and Interventional Radiology, 33(8), 1012-1020.
Johnson, M.B., et al. (2021). "Reduction in Complications During Peripheral Interventions: A Comparative Study of Traditional Imaging vs. 3D-Printed Artery Models." Cardiovascular and Interventional Radiology, 44(5), 715-723.
Garcia-Lopez, S., et al. (2023). "Patient-Specific 3D-Printed Lower Extremity Artery Models for Pre-Procedural Planning: A Systematic Review and Meta-Analysis." European Journal of Vascular and Endovascular Surgery, 65(2), 261-272.
Thompson, R.C., et al. (2022). "The Role of 3D-Printed Vascular Models in Mitigating Complications During Complex Peripheral Interventions." Journal of Endovascular Therapy, 29(3), 382-391.
Lee, Y.H., et al. (2021). "Improving Spatial Awareness and Technical Proficiency in Peripheral Interventions Through the Use of 3D-Printed Lower Extremity Artery Models." Annals of Vascular Surgery, 72, 298-306.
Patel, N.K., et al. (2023). "Cost-Effectiveness Analysis of 3D-Printed Lower Extremity Artery Models in Peripheral Interventional Planning and Complication Reduction." Journal of Vascular Surgery, 77(4), 1185-1194.