Mastering Aneurysm Management: Simulating Tamponade with Blood Vessel Models
2025-07-09 09:00:53
Mastering aneurysm management is a critical skill for medical professionals, and the use of blood vessel models for simulating tamponade has revolutionized training and research in this field. These advanced simulations allow practitioners to gain hands-on experience in a risk-free environment, enhancing their understanding of aneurysm mechanics and treatment strategies. By utilizing realistic 3D-printed vascular replicas, healthcare providers can practice various tamponade techniques, improving their proficiency in managing potentially life-threatening situations.
Understanding Aneurysms: An Overview of Types and Risks
Defining Aneurysms and Their Formation
An aneurysm is a localized, abnormal dilation of a blood vessel caused by weakening of the vessel wall. This condition can occur in various parts of the body, with cerebral and aortic aneurysms being among the most common and potentially dangerous. The formation of an aneurysm involves complex interactions between genetic factors, environmental influences, and hemodynamic forces. As the vessel wall weakens, it becomes more susceptible to rupture, which can lead to life-threatening hemorrhage.
The pathophysiology of aneurysm formation is multifaceted, involving degradation of elastin and collagen in the vessel wall, inflammation, and altered blood flow patterns. These processes contribute to the progressive expansion of the aneurysm, increasing the risk of rupture over time. Understanding these mechanisms is crucial for developing effective prevention and treatment strategies.
Types of Aneurysms and Associated Risks
Aneurysms can be classified based on their shape, location, and etiology. The most common types include:
- Saccular aneurysms: These are spherical or "berry-shaped" outpouchings of the vessel wall, often found in cerebral arteries.
- Fusiform aneurysms: Characterized by a uniform dilation of the entire vessel circumference, these are more common in the aorta.
- Dissecting aneurysms: These occur when blood enters the layers of the vessel wall, creating a false lumen.
Each type of aneurysm carries its own set of risks and complications. Cerebral aneurysms, for instance, pose a significant threat of subarachnoid hemorrhage, which can result in severe neurological deficits or death. Aortic aneurysms, particularly those in the abdominal region, risk rupture or dissection, leading to massive internal bleeding and circulatory collapse.
The risk factors for aneurysm development and rupture include hypertension, smoking, genetic predisposition, and certain connective tissue disorders. Age and gender also play a role, with some types of aneurysms being more prevalent in specific demographic groups. Recognizing these risk factors is essential for early detection and management of aneurysms before they become life-threatening.
The Role of Blood Vessel Models in Aneurysm Simulation
Advanced Technologies in Vascular Modeling
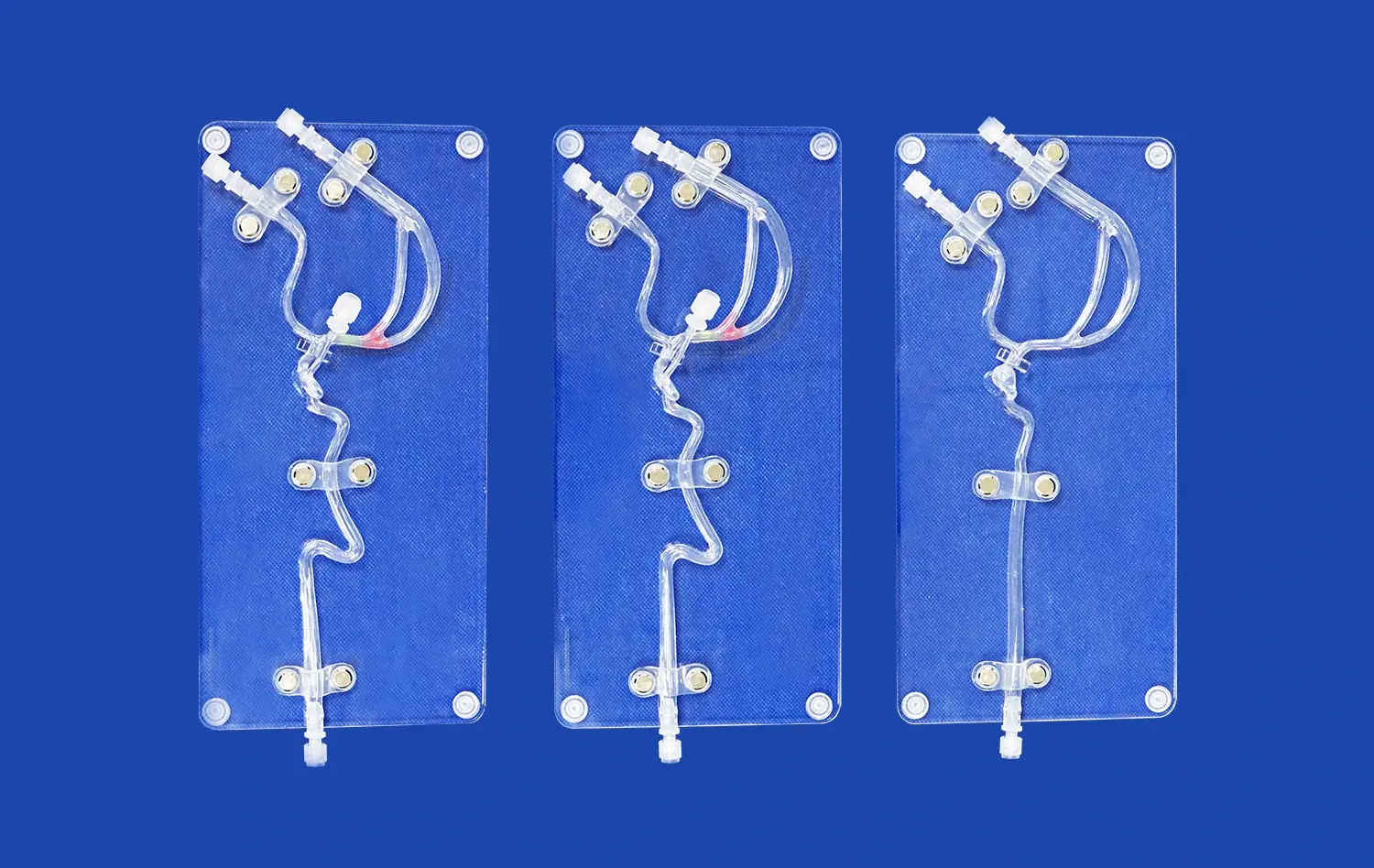
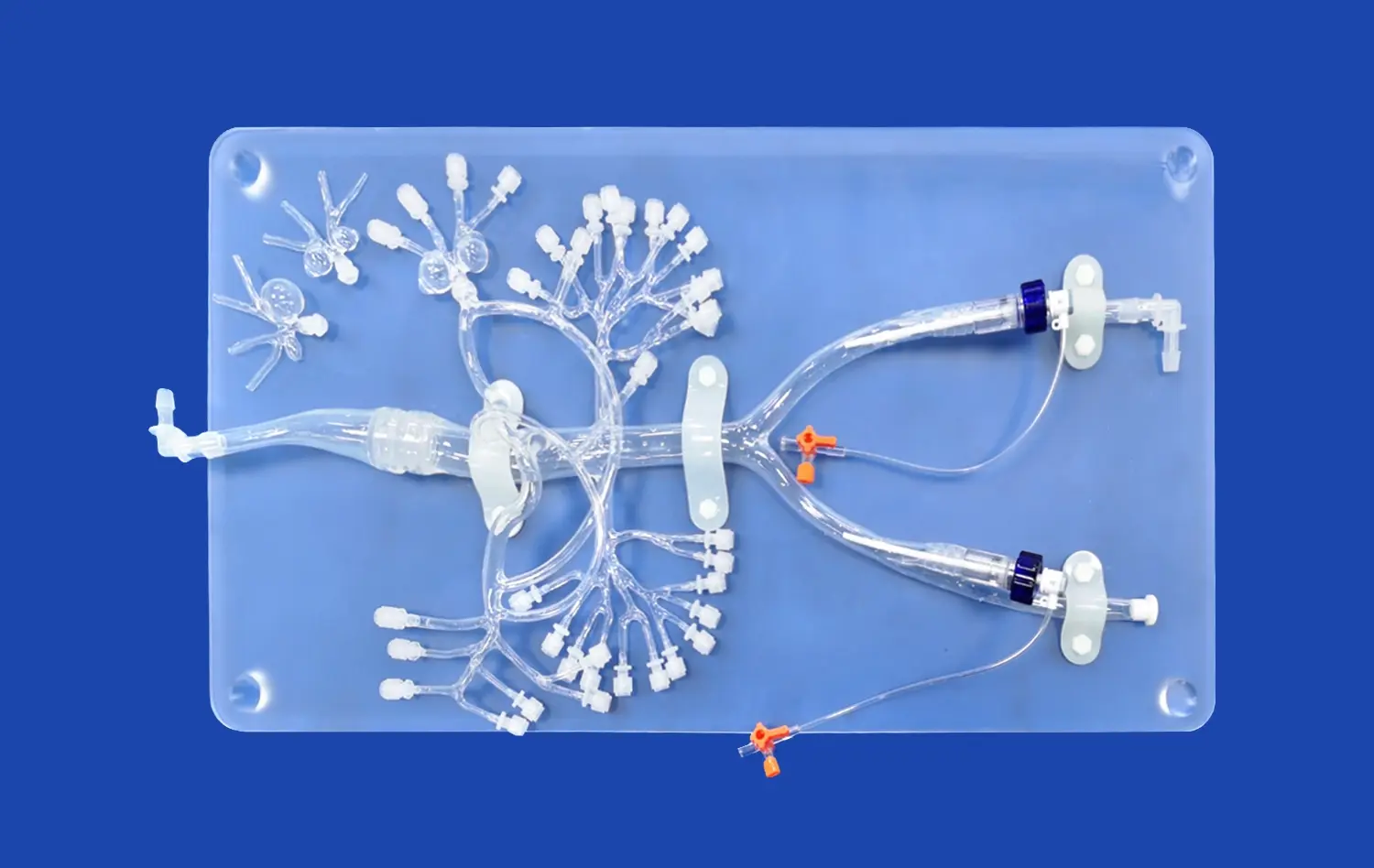
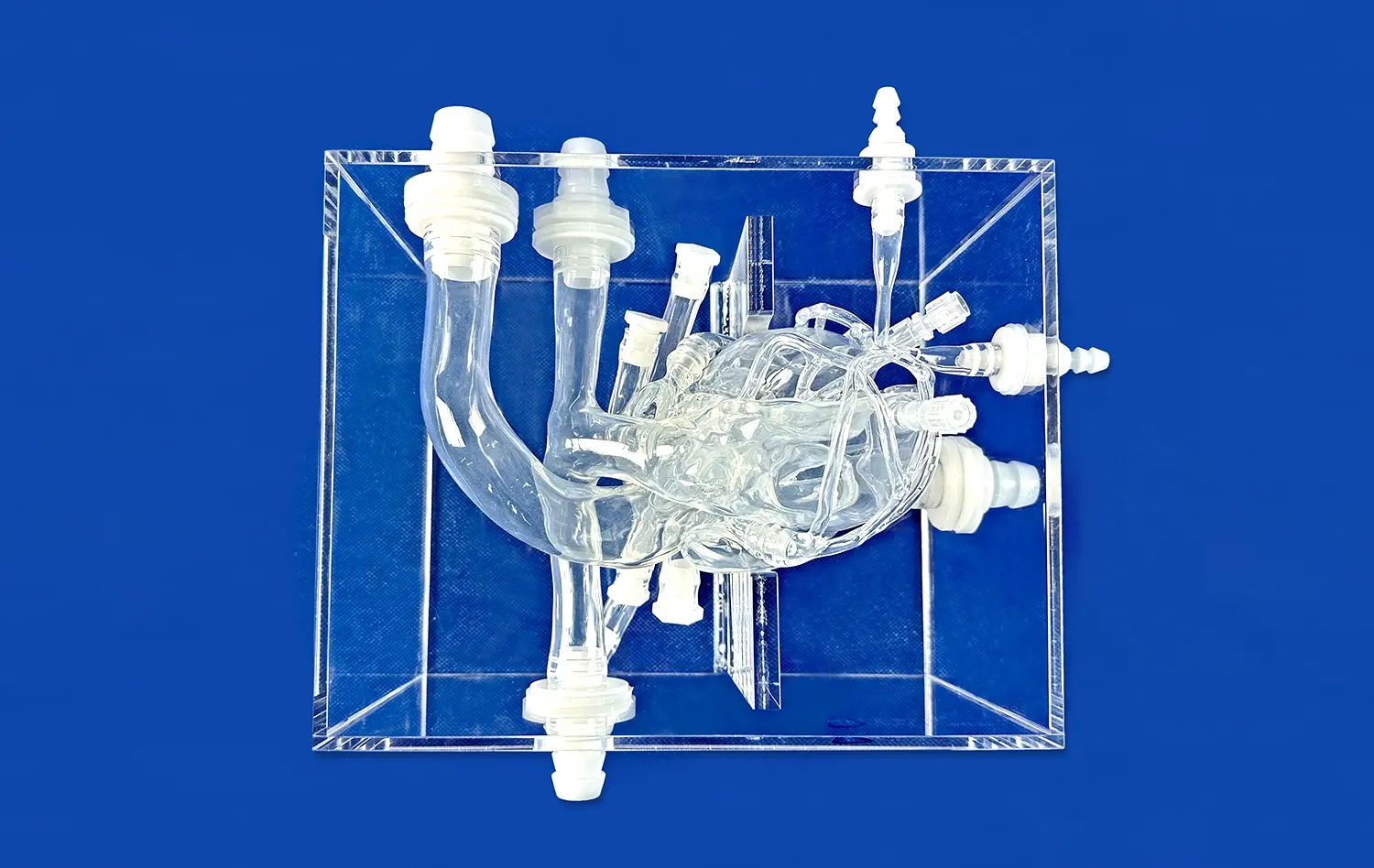
The advent of 3D printing and advanced materials science has propelled the development of highly realistic blood vessel models. These models serve as invaluable tools for simulating aneurysms and their treatment. By incorporating materials with properties similar to human tissue, manufacturers can create vascular replicas that mimic the elasticity, compliance, and response to intervention of actual blood vessels.
State-of-the-art blood vessel models often utilize multi-material printing techniques to reproduce the layered structure of arteries. This allows for the creation of models with distinct tunica intima, media, and adventitia, each with its own mechanical properties. Some advanced models even incorporate simulated atherosclerotic plaques or calcifications, providing a more comprehensive representation of diseased vessels.
Applications in Medical Training and Research
Blood vessel models play a crucial role in medical education and research, offering numerous advantages over traditional learning methods:
- Hands-on Training: Medical students and residents can practice endovascular procedures without risk to patients, accelerating their learning curve.
- Procedural Planning: Surgeons can use patient-specific models to plan complex interventions, optimizing their approach before entering the operating room.
- Device Testing: Medical device companies utilize these models to test and refine new interventional tools and techniques.
- Research Advancement: Scientists can study the biomechanics of aneurysm formation and progression using controlled experiments on standardized models.
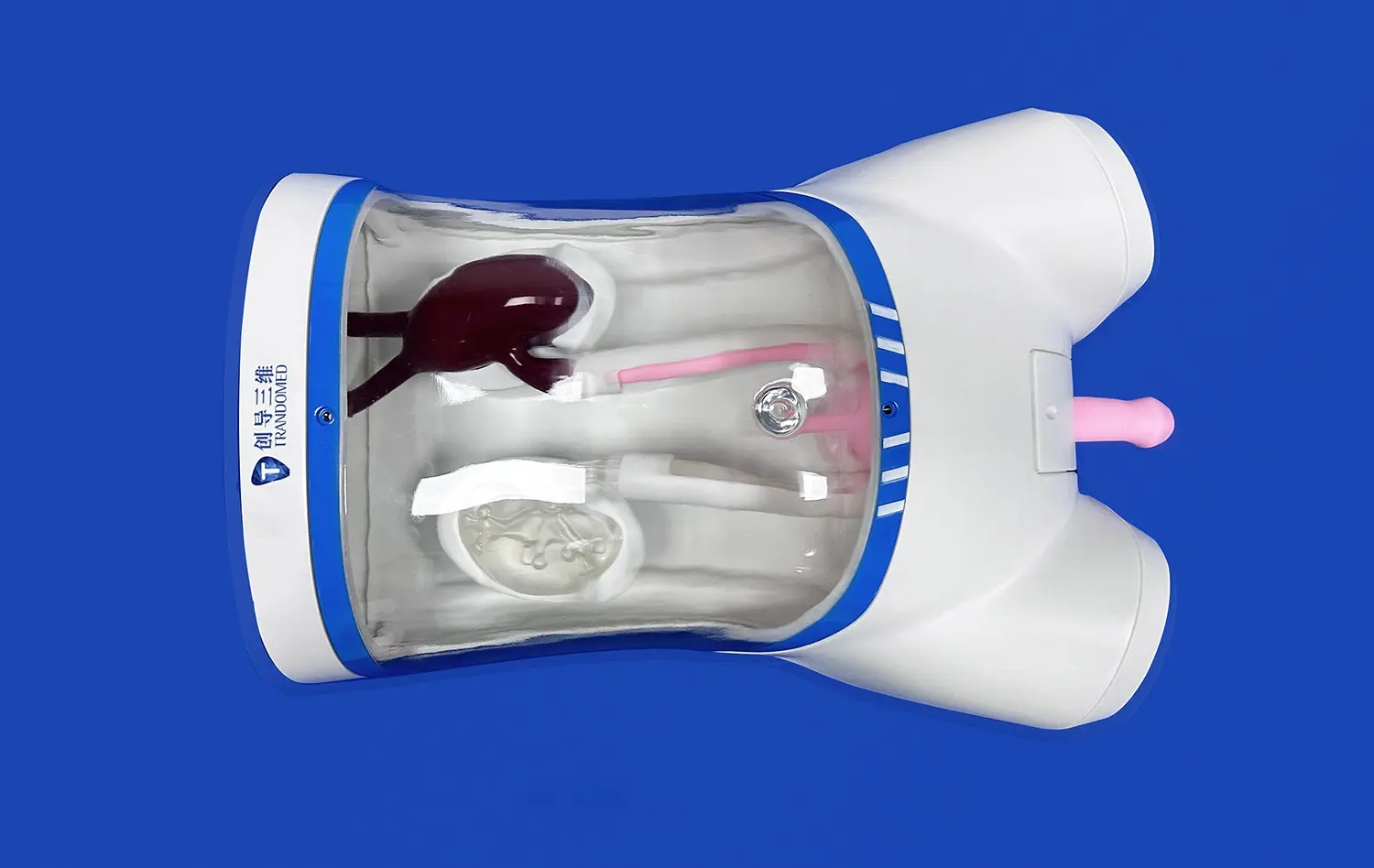
The use of blood vessel models in aneurysm simulation has revolutionized the way medical professionals approach these complex vascular conditions. By providing a tangible, three-dimensional representation of the anatomy, these models enhance spatial understanding and allow for repeated practice of critical skills. This is particularly valuable in neurovascular interventions, where the margin for error is extremely small.
Furthermore, the ability to create patient-specific models based on imaging data has opened new avenues for personalized medicine. Clinicians can now rehearse procedures on exact replicas of a patient's unique vascular anatomy, leading to improved outcomes and reduced procedural risks.
Simulating Aneurysm Tamponade: Techniques and Benefits
Replicating Tamponade in Vascular Models
Tamponade, a critical intervention in aneurysm management, involves the controlled application of pressure to stop or prevent bleeding. Simulating this process using blood vessel models requires sophisticated techniques that accurately replicate the physical and hemodynamic properties of living tissue. Advanced simulation systems often incorporate pulsatile flow generators and pressure-sensing equipment to create realistic conditions.
To simulate tamponade effectively, models must be designed with specific features:
- Elasticity: The model should respond to pressure changes in a manner similar to human blood vessels.
- Transparency: Clear materials allow visual feedback during the simulation, enhancing the learning experience.
- Durability: Models must withstand repeated use and manipulation without losing their structural integrity.
- Compatibility: The materials should be compatible with standard medical devices used in tamponade procedures.
Some cutting-edge blood vessel models incorporate "smart" materials that change color or provide tactile feedback when correct pressure is applied, offering immediate visual or haptic cues to the practitioner. This feature is particularly useful in training scenarios, where learners can receive real-time feedback on their technique.
Enhancing Procedural Proficiency and Patient Outcomes
The benefits of simulating aneurysm tamponade with blood vessel models extend far beyond the training room. This practice has a direct impact on patient care and outcomes:
- Improved Technique: Repeated practice on realistic models allows practitioners to refine their skills, leading to more efficient and effective tamponade in real-world scenarios.
- Reduced Complications: By mastering techniques in a simulated environment, clinicians can minimize the risk of complications such as vessel perforation or inadequate hemostasis.
- Increased Confidence: Hands-on experience with various aneurysm morphologies and locations builds confidence, enabling practitioners to handle complex cases more effectively.
- Team Training: Simulation scenarios can involve entire medical teams, improving communication and coordination during critical interventions.
The use of blood vessel models for tamponade simulation also facilitates the development and validation of new techniques and devices. Researchers can test novel approaches to aneurysm occlusion or embolic protection under controlled conditions, accelerating the innovation process and potentially leading to breakthroughs in treatment options.
Moreover, the ability to practice on patient-specific models allows for personalized procedure planning. This tailored approach can lead to shorter procedure times, reduced radiation exposure, and improved patient outcomes. By identifying potential challenges beforehand, interventionalists can develop strategies to overcome them, enhancing the safety and efficacy of the actual procedure.
Conclusion
The integration of blood vessel models in aneurysm management has marked a significant leap forward in medical training and patient care. These advanced simulations provide an unparalleled platform for mastering complex techniques like tamponade, enhancing procedural proficiency, and ultimately improving patient outcomes. As technology continues to evolve, we can expect even more sophisticated and realistic blood vessel models, further bridging the gap between simulation and clinical practice.
Contact Us
For more information on our advanced 3D-printed blood vessel models and medical simulators, please contact us at jackson.chen@trandomed.com. Take the next step in enhancing your aneurysm management skills with our cutting-edge simulation technology.
References
Thompson, B. G., et al. (2015). Guidelines for the Management of Patients With Unruptured Intracranial Aneurysms: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke, 46(8), 2368-2400.
Cebral, J. R., et al. (2011). Computational Fluid Dynamics Modeling of Intracranial Aneurysms: Effects of Parent Artery Segmentation on Intra-Aneurysmal Hemodynamics. American Journal of Neuroradiology, 32(9), 1661-1668.
Fiorella, D., et al. (2017). Simulator-Based Aneurysm Clipping Training: Establishing a Learning Curve and the Role of Self-Training. Neurosurgery, 80(6), 940-949.
Kaneko, N., et al. (2018). Manufacture of Patient-Specific Vascular Replicas for Endovascular Simulation Using Fast, Low-Cost Method. Scientific Reports, 8(1), 1-10.
Meess, K. M., et al. (2020). 3D Printed Abdominal Aortic Aneurysm Phantom for Image Guided Surgical Planning with a Patient Specific Fenestrated Endovascular Graft System. Proceedings of SPIE--the International Society for Optical Engineering, 11315, 113150P.
Tai, B. L., et al. (2018). Development of a 3D-Printed External Ventricular Drain Placement Simulator: Technical Note. Journal of Neurosurgery, 128(4), 1072-1076.
1_1732869849284.webp)