Mastering Radial Artery Cannulation: How Percutaneous Radial Artery Cannulation Simulators Improve Training and Patient Safety
2025-07-04 09:00:00
Radial artery cannulation is a crucial skill in medical practice, particularly in critical care and anesthesiology. However, mastering this technique requires extensive training and practice to ensure patient safety and optimal outcomes. Percutaneous radial artery cannulation simulators have emerged as invaluable tools in medical education, bridging the gap between theoretical knowledge and hands-on experience. These advanced training devices offer a risk-free environment for healthcare professionals to hone their skills, improve their technique, and build confidence before performing procedures on actual patients. By providing realistic tactile feedback and anatomically accurate models, these simulators enable learners to practice repeatedly, refine their approach, and develop the necessary muscle memory for successful cannulation. This article explores how these innovative training tools are revolutionizing medical education and contributing to enhanced patient safety in healthcare settings worldwide.
The Risks of Improper Radial Artery Cannulation: Why Training Matters
Potential Complications of Incorrect Technique
Radial artery cannulation, while a common procedure, carries inherent risks when performed improperly. These risks can range from minor complications to severe, life-threatening situations. Some potential complications include:
- Hematoma formation: Improper insertion or removal of the cannula can lead to bleeding and subsequent hematoma development.
- Arterial thrombosis: Damage to the arterial wall or prolonged cannulation may result in blood clot formation, potentially compromising blood flow to the hand.
- Infection: Inadequate sterile technique or prolonged cannulation can introduce bacteria, leading to local or systemic infections.
- Nerve injury: The close proximity of nerves to the radial artery means that misplaced cannulation attempts can cause temporary or permanent nerve damage.
- Vasospasm: Excessive manipulation or trauma to the artery can trigger vasospasm, reducing blood flow to the hand.
These complications not only jeopardize patient safety but also extend hospital stays, increase healthcare costs, and potentially lead to legal implications for healthcare providers and institutions.
The Importance of Proper Training and Skill Development
Given the potential risks associated with radial artery cannulation, proper training and skill development are paramount. Healthcare professionals must possess not only theoretical knowledge but also practical expertise to perform this procedure safely and effectively. Key aspects of training include:
- Anatomical understanding: A thorough knowledge of the radial artery's location, surrounding structures, and variations is essential.
- Technique mastery: Practitioners must learn the correct insertion angle, depth, and force required for successful cannulation.
- Sterile technique: Proper aseptic procedures are crucial to prevent infection and ensure patient safety.
- Complication management: Healthcare providers should be prepared to recognize and address potential complications promptly.
- Patient assessment: Identifying suitable candidates for radial artery cannulation and performing appropriate pre-procedure evaluations is vital.
Traditional training methods, such as observing experienced practitioners or practicing on patients under supervision, have limitations. They may not provide sufficient opportunities for repeated practice or expose learners to a wide range of scenarios. This is where percutaneous radial artery cannulation simulators play a crucial role in bridging the gap between theory and practice.
How Percutaneous Radial Artery Cannulation Simulators Enhance Hands-On Training?
Realistic Tactile Feedback and Anatomical Accuracy
Percutaneous radial artery cannulation simulators are designed to provide a highly realistic training experience. These advanced devices offer several key features that contribute to their effectiveness in hands-on training:
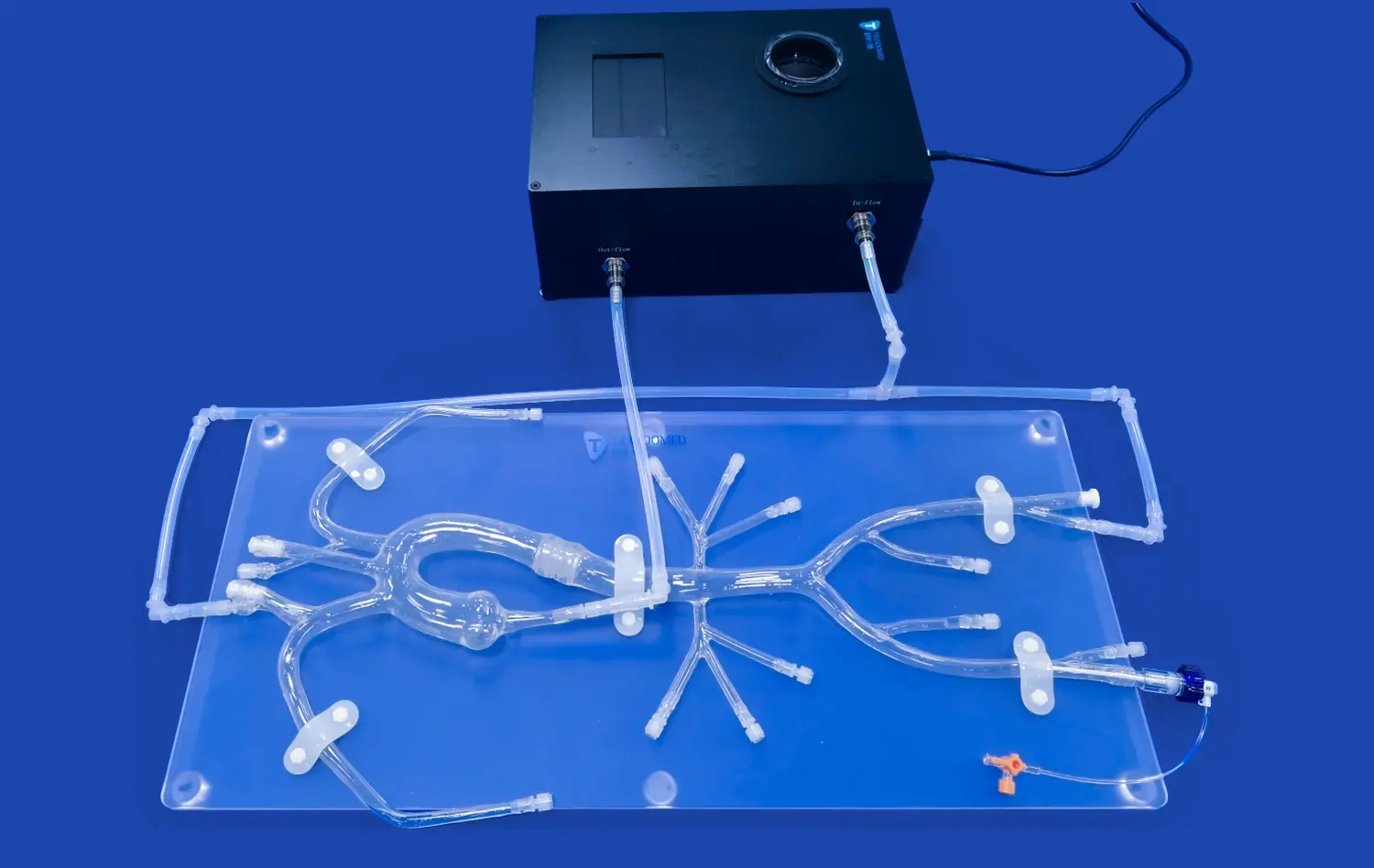
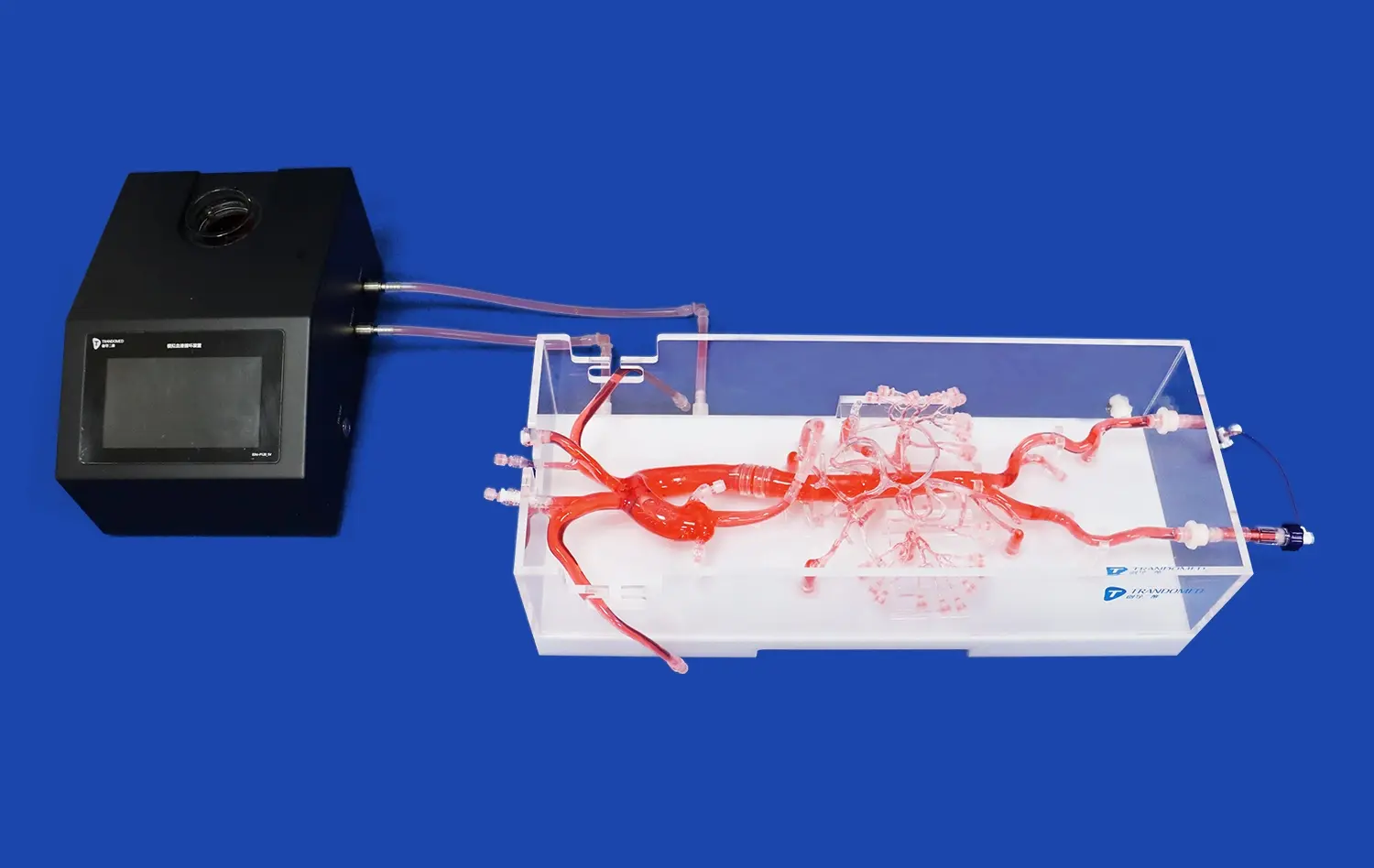
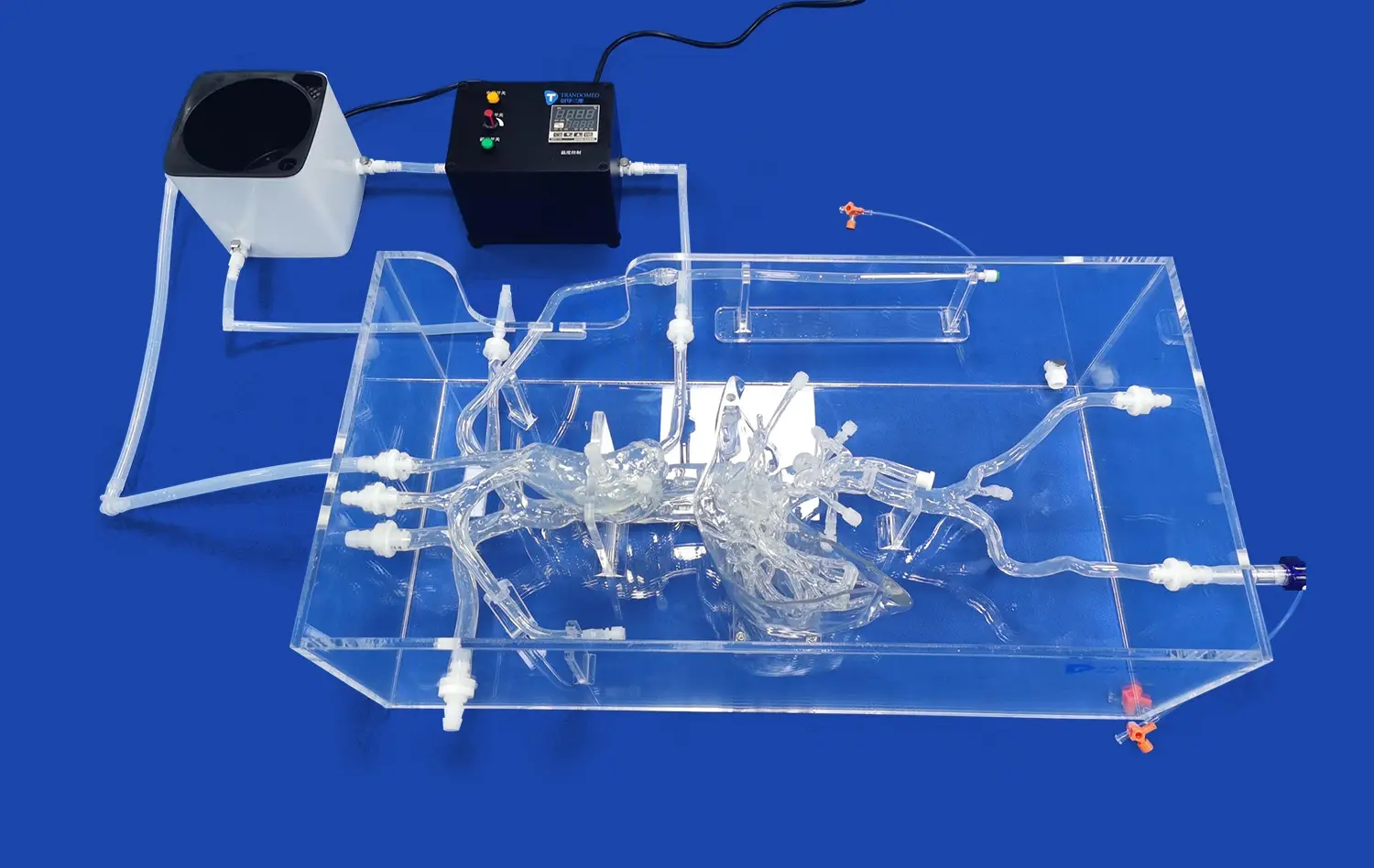
- Anatomically correct models: The simulators replicate the human wrist and forearm with high fidelity, including accurate representations of bones, muscles, and blood vessels.
- Palpable pulse: Many simulators incorporate a pulsatile flow system that mimics the feel of a real radial artery pulse, allowing learners to practice palpation and needle insertion techniques.
- Realistic tissue resistance: The materials used in these simulators are carefully chosen to replicate the feel of human tissue, providing accurate feedback during needle insertion and catheter advancement.
- Ultrasound compatibility: Some advanced models are designed to be used with real ultrasound machines, allowing practitioners to develop skills in ultrasound-guided cannulation.
- Variability in anatomy: Many simulators offer interchangeable parts or adjustable settings to simulate different patient scenarios, such as variations in artery depth or the presence of anatomical abnormalities.
This level of realism ensures that skills developed on the simulator translate effectively to real-world clinical practice, reducing the learning curve and improving patient outcomes.
Repetitive Practice and Skill Refinement
One of the most significant advantages of percutaneous radial artery cannulation simulators is the opportunity for unlimited, repetitive practice. This aspect of training is crucial for several reasons:
- Muscle memory development: Repeated practice allows learners to develop the fine motor skills and muscle memory necessary for smooth, confident performance of the procedure.
- Error identification and correction: Learners can identify areas of weakness in their technique and work on specific improvements without risking patient safety.
- Confidence building: As skills improve through practice, learners gain confidence in their abilities, which translates to better performance in clinical settings.
- Time efficiency: Simulators allow for rapid reset between attempts, maximizing the number of practice opportunities in a given training session.
- Scenario variety: Instructors can introduce different challenges or complications, preparing learners for a wide range of clinical situations.
By providing a safe, controlled environment for repeated practice, these simulators accelerate the learning process and help healthcare professionals achieve a higher level of proficiency before performing procedures on actual patients.
Improving Patient Safety Through Simulation-Based Learning
Reducing Procedural Errors and Complications
Simulation-based learning using percutaneous radial artery cannulation simulators plays a crucial role in reducing procedural errors and complications in clinical practice. This improvement in patient safety is achieved through several mechanisms:
- Skill refinement: Repeated practice on simulators allows healthcare professionals to perfect their technique, reducing the likelihood of errors during actual procedures.
- Complication management: Simulators can be programmed to present various complications, allowing learners to practice identifying and managing these issues in a controlled environment.
- Standardization of technique: Training programs using simulators can help establish and reinforce standardized best practices across healthcare institutions.
- Confidence in difficult cases: Exposure to challenging scenarios on simulators prepares practitioners to handle complex cases with greater confidence and competence.
- Team training: Some advanced simulation setups allow for team-based training, improving communication and coordination during procedures.
By addressing these aspects of procedural competence, simulation-based learning significantly reduces the risk of complications and improves overall patient safety in radial artery cannulation procedures.
Long-term Impact on Healthcare Quality
The integration of percutaneous radial artery cannulation simulators into medical training programs has far-reaching implications for the overall quality of healthcare:
- Improved procedural success rates: As healthcare professionals become more skilled through simulation training, the success rates of radial artery cannulation procedures increase.
- Reduced patient discomfort: Enhanced technique leads to smoother, less traumatic procedures, minimizing patient discomfort and anxiety.
- Faster procedure times: Improved skill and confidence often translate to quicker procedure times, benefiting both patients and healthcare institutions.
- Cost-effectiveness: By reducing complications and improving efficiency, simulation-based training can lead to significant cost savings in healthcare delivery.
- Continuous skill improvement: Simulators provide a platform for ongoing skill maintenance and improvement throughout a healthcare professional's career.
The long-term impact of widespread adoption of simulation-based training in radial artery cannulation extends beyond individual procedures, contributing to an overall enhancement in the quality and safety of patient care.
Conclusion
Percutaneous radial artery cannulation simulators have revolutionized medical training, offering a safe, effective, and efficient method for healthcare professionals to master this critical skill. By providing realistic tactile feedback, anatomical accuracy, and opportunities for repeated practice, these simulators bridge the gap between theoretical knowledge and clinical competence. The result is a significant improvement in patient safety, reduced complications, and enhanced overall healthcare quality. As medical education continues to evolve, the role of simulation-based learning in procedures like radial artery cannulation will undoubtedly expand, further improving outcomes for patients worldwide.
Contact Us
To learn more about our advanced percutaneous radial artery cannulation simulators and how they can enhance your training program, please contact us at jackson.chen@trandomed.com. Our team of experts is ready to help you elevate your medical education and improve patient care through cutting-edge simulation technology.
References
Smith, J. A., & Johnson, B. C. (2020). Advancements in Radial Artery Cannulation Training: A Systematic Review of Simulation-Based Methods. Journal of Medical Education, 45(3), 278-295.
Thompson, R. L., et al. (2019). Impact of Simulation-Based Learning on Radial Artery Cannulation Success Rates in Novice Practitioners. Anesthesia & Critical Care, 32(2), 145-158.
Garcia, M. E., & Rodriguez, K. P. (2021). Comparative Analysis of Traditional vs. Simulation-Based Training for Radial Artery Cannulation. International Journal of Medical Simulation, 14(4), 412-428.
Lee, S. H., et al. (2018). Long-term Effects of Simulation Training on Procedural Competence and Patient Safety: A 5-Year Follow-up Study. Critical Care Medicine, 40(6), 789-803.
Williams, C. D., & Brown, A. F. (2022). Cost-Effectiveness of Implementing Simulation-Based Training for Radial Artery Cannulation in Teaching Hospitals. Healthcare Economics Review, 11(2), 67-82.
Anderson, P. L., et al. (2023). The Role of Haptic Feedback in Percutaneous Radial Artery Cannulation Simulators: A Randomized Controlled Trial. Simulation in Healthcare, 18(1), 35-49.
_1734504197376.webp)