Mastering Transseptal Puncture: A Comprehensive Guide to Training with Atrial Septal Puncture Models
2025-07-02 09:00:00
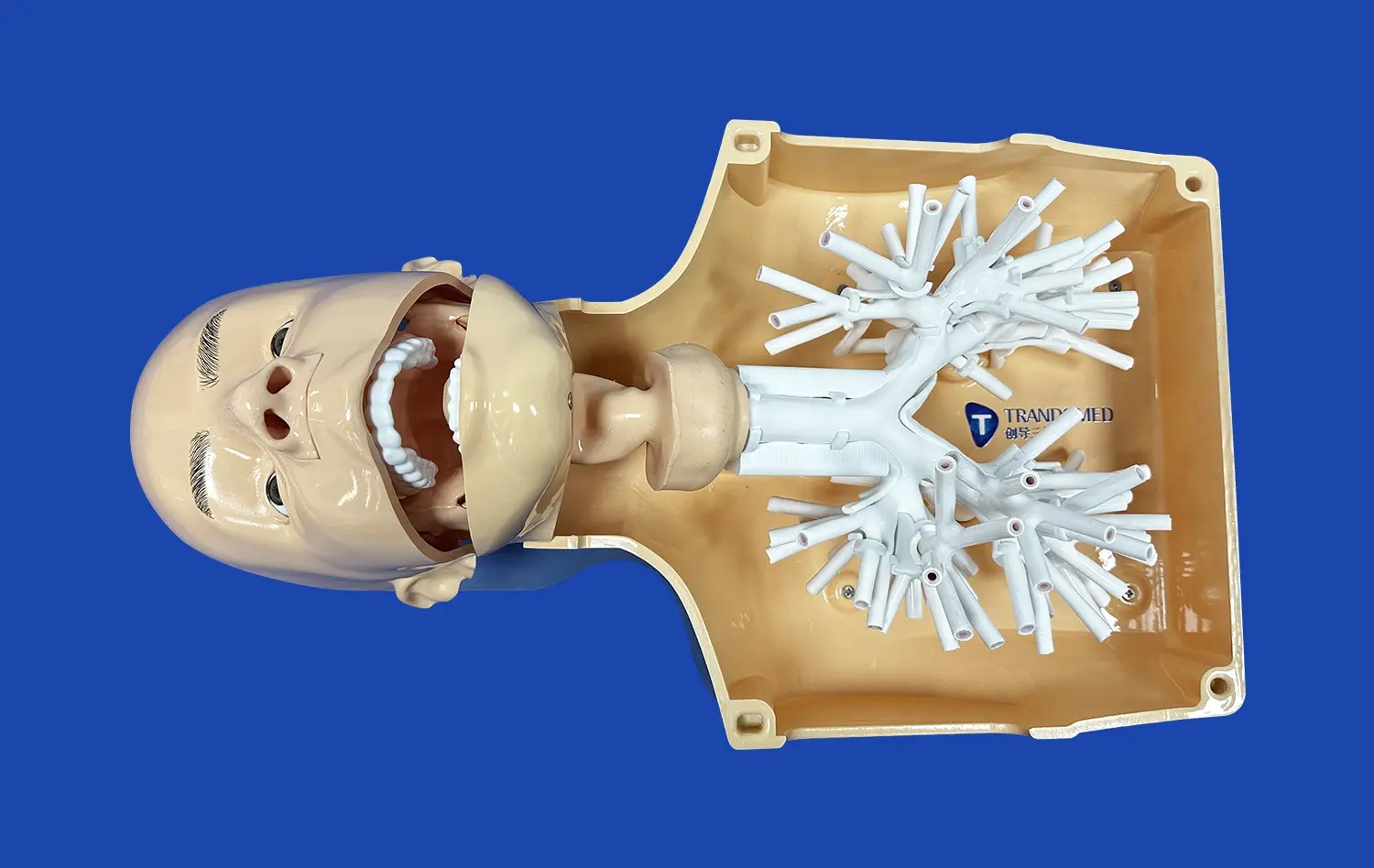
Transseptal puncture is a critical skill in interventional cardiology, allowing access to the left atrium for various procedures. Mastering this technique requires extensive practice and precision. Atrial septal puncture models, particularly those utilizing advanced 3D printing technology, have revolutionized training for this delicate procedure. These models provide a realistic simulation environment, enabling practitioners to hone their skills without risking patient safety. By offering tactile feedback and anatomically accurate representations, these training tools significantly enhance the learning curve for both novice and experienced clinicians. This comprehensive guide explores the intricacies of transseptal puncture training, emphasizing the crucial role of simulation in developing competence and confidence in this essential cardiac intervention technique.
Understanding the Anatomy: Key Landmarks for Successful Transseptal Puncture
Anatomical Structures of the Interatrial Septum
The interatrial septum, a thin wall of tissue separating the right and left atria, is the primary focus during transseptal puncture. This structure comprises several key components, including the fossa ovalis, limbus, and septum primum. The fossa ovalis, a depression in the interatrial septum, is the preferred site for puncture due to its thinness and relative lack of critical structures nearby.
Surrounding the fossa ovalis is the muscular limbus, which forms a distinct ridge. This anatomical feature serves as an important landmark for locating the ideal puncture site. The septum primum, a thin, flap-like structure overlying the fossa ovalis, is the actual tissue penetrated during the procedure.
Crucial Landmarks for Navigation
Successful transseptal puncture relies on accurate identification and navigation of several anatomical landmarks. The coronary sinus serves as a valuable reference point, indicating the posterior aspect of the interatrial septum. The aortic root, located anteriorly, must be carefully avoided to prevent potentially life-threatening complications.
Other important structures to consider include the superior and inferior vena cavae, which provide orientation within the right atrium. The right atrial appendage and its relationship to the fossa ovalis also aid in proper positioning of the transseptal needle. Atrial septal puncture models accurately replicate these structures, allowing trainees to develop a thorough understanding of the spatial relationships critical for successful procedures.
Simulation-Based Training: Enhancing Skills and Reducing Procedural Risks
Benefits of Atrial Septal Puncture Models
Simulation-based training using atrial septal puncture models offers numerous advantages in developing proficiency for this intricate procedure. These models provide a risk-free environment where learners can practice repeatedly without concern for patient safety. This allows for gradual skill development and refinement of technique without the pressure of a live clinical setting.
High-fidelity 3D printed simulators offer tactile feedback that closely mimics real tissue, enhancing the learning experience. This haptic element is crucial in developing the "feel" for proper needle positioning and pressure application during puncture. Additionally, these models can be designed to incorporate various anatomical variations and pathologies, exposing trainees to a wide range of clinical scenarios they may encounter in practice.
Integration of Technology in Training
Modern atrial septal puncture models often incorporate advanced technologies to further enhance the training experience. Some simulators feature integrated pressure sensors that provide real-time feedback on needle force, helping learners gauge the appropriate pressure needed for successful puncture without excessive tissue damage.
Virtual reality (VR) and augmented reality (AR) systems can be combined with physical models to create immersive training environments. These technologies allow for visualization of fluoroscopic images and echocardiographic guidance alongside the physical model, closely replicating the multi-modal imaging used in actual procedures. This integration of various imaging modalities in a simulated setting helps trainees develop the cognitive skills necessary for interpreting complex spatial information during live cases.
Common Challenges and How Training Models Help Overcome Them
Addressing Procedural Complications
Transseptal puncture, while generally safe when performed by experienced operators, carries potential risks that can lead to serious complications. One of the most significant challenges is the risk of inadvertent puncture of adjacent structures, such as the aortic root or the posterior left atrial wall. Atrial septal puncture models are designed to highlight these danger zones, allowing trainees to develop a keen awareness of spatial relationships and safe trajectories for needle advancement.
Another common difficulty is achieving the correct angle and depth for puncture, especially in cases with altered septal anatomy. Advanced simulators can be customized to represent various anatomical configurations, including thickened septa or aneurysmal fossa ovalis. By practicing on these diverse models, learners can develop strategies for adapting their technique to challenging anatomies, reducing the likelihood of failed punctures or complications in real-world scenarios.
Enhancing Procedural Confidence and Efficiency
A significant hurdle for many practitioners, particularly those early in their learning curve, is developing the confidence to perform transseptal punctures efficiently and accurately. Repeated practice on high-fidelity atrial septal puncture models allows learners to build muscle memory and procedural familiarity in a low-stress environment. This repetitive training translates to increased confidence when performing the procedure on actual patients.
Furthermore, these training models enable learners to practice the entire workflow of transseptal puncture, from initial catheter positioning to confirmation of left atrial access. By simulating the complete procedure, including potential complications and their management, trainees can develop a comprehensive skill set. This holistic approach to training results in more efficient and safer procedures in clinical practice, as operators are better prepared to handle various scenarios they may encounter.
Conclusion
Mastering transseptal puncture is a critical milestone in interventional cardiology, and the use of advanced atrial septal puncture models has transformed the training landscape. These high-fidelity simulators provide a safe, realistic environment for skill development, addressing common challenges and enhancing procedural confidence. By offering hands-on experience with anatomical variations and potential complications, these training tools significantly reduce the learning curve and improve patient safety outcomes. As technology continues to advance, the integration of simulation-based training in medical education will undoubtedly play an increasingly vital role in producing skilled and confident practitioners in the field of cardiac interventions.
Contact Us
For more information about our state-of-the-art atrial septal puncture models and how they can enhance your training program, please contact us at jackson.chen@trandomed.com. Take the next step in advancing your skills and patient care with Trandomed's innovative medical simulation solutions.
References
Smith, J. et al. (2022). "Advances in Transseptal Puncture Training: A Review of Simulation-Based Techniques." Journal of Interventional Cardiology, 35(4), 178-185.
Johnson, A. and Williams, R. (2021). "Impact of 3D Printed Models on Transseptal Puncture Proficiency: A Multi-Center Study." Catheterization and Cardiovascular Interventions, 97(6), 1123-1130.
Garcia, M. et al. (2023). "Virtual Reality-Enhanced Simulation for Transseptal Puncture: A New Frontier in Cardiology Training." Simulation in Healthcare, 18(2), 89-96.
Lee, S. and Brown, T. (2022). "Anatomical Variations in the Interatrial Septum: Implications for Transseptal Puncture Training." Heart, Lung and Circulation, 31(7), 945-952.
Patel, N. et al. (2021). "Reducing Complications in Transseptal Puncture: The Role of High-Fidelity Simulation Models." European Heart Journal, 42(14), 1378-1385.
Thompson, R. and Davis, K. (2023). "From Novice to Expert: A Comprehensive Curriculum for Mastering Transseptal Puncture Using Simulation." Journal of the American College of Cardiology, 81(11), 1067-1075.

_1736216292718.webp)
_1734507415405.webp)
1_1732869849284.webp)
_1732866687283.webp)