In the realm of neurovascular interventions, mastering the art of aneurysm embolization is paramount. The neuro vascular simulator has emerged as an indispensable tool for training and honing the skills of interventional neuroradiologists and neurosurgeons. This cutting-edge technology replicates the intricate vascular anatomy with remarkable precision, allowing practitioners to practice and perfect their techniques in a risk-free environment. By providing a lifelike simulation of cerebral aneurysms, these advanced simulators enable medical professionals to develop their expertise in navigating complex vasculature, deploying embolic devices, and managing potential complications. The integration of neuro vascular simulators in training programs has revolutionized the approach to aneurysm embolization education, bridging the gap between theoretical knowledge and practical application.
Replicating the Aneurysmal Landscape: The Anatomical Fidelity of the Neuro Vascular Simulator
Unparalleled Anatomical Accuracy
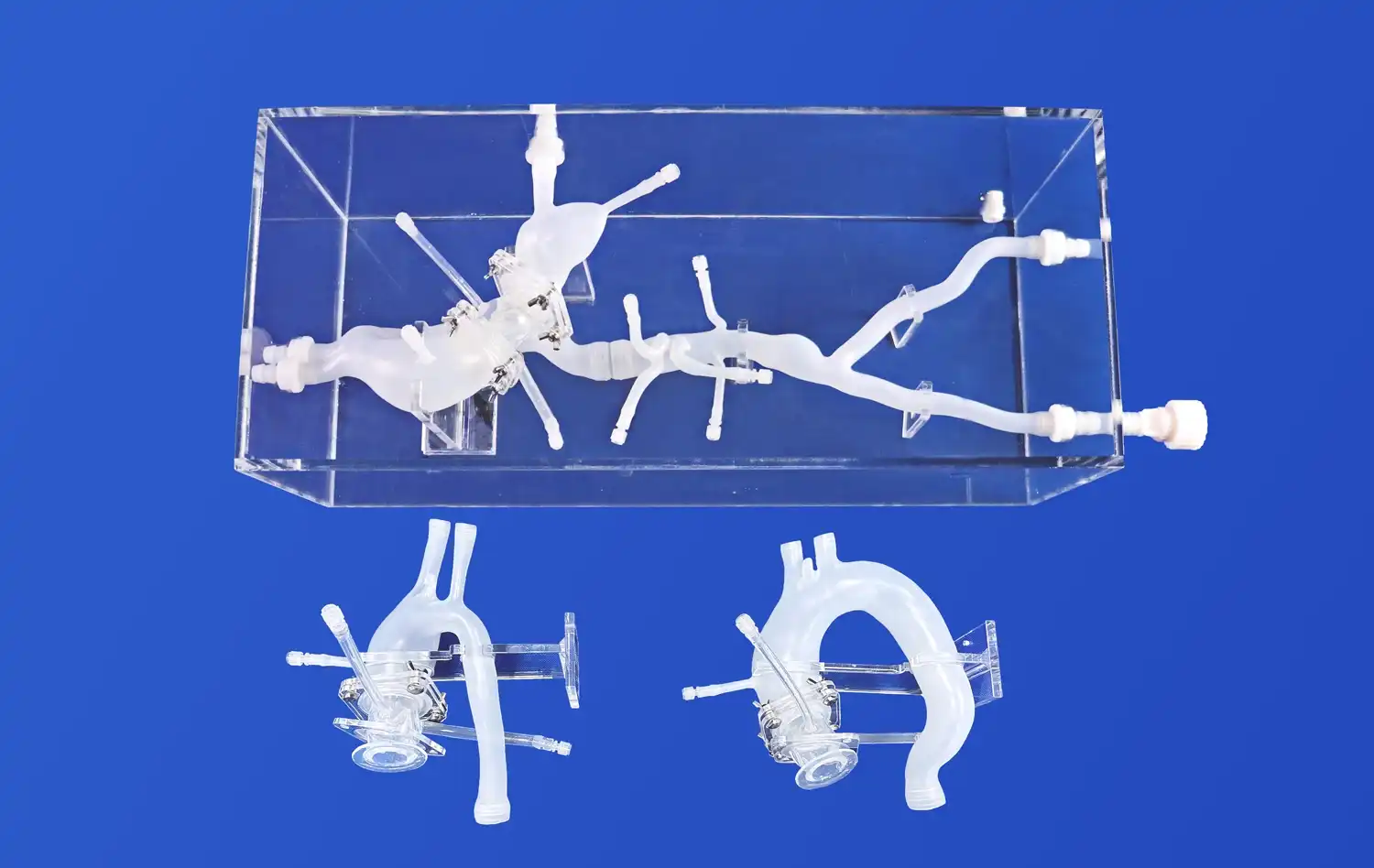
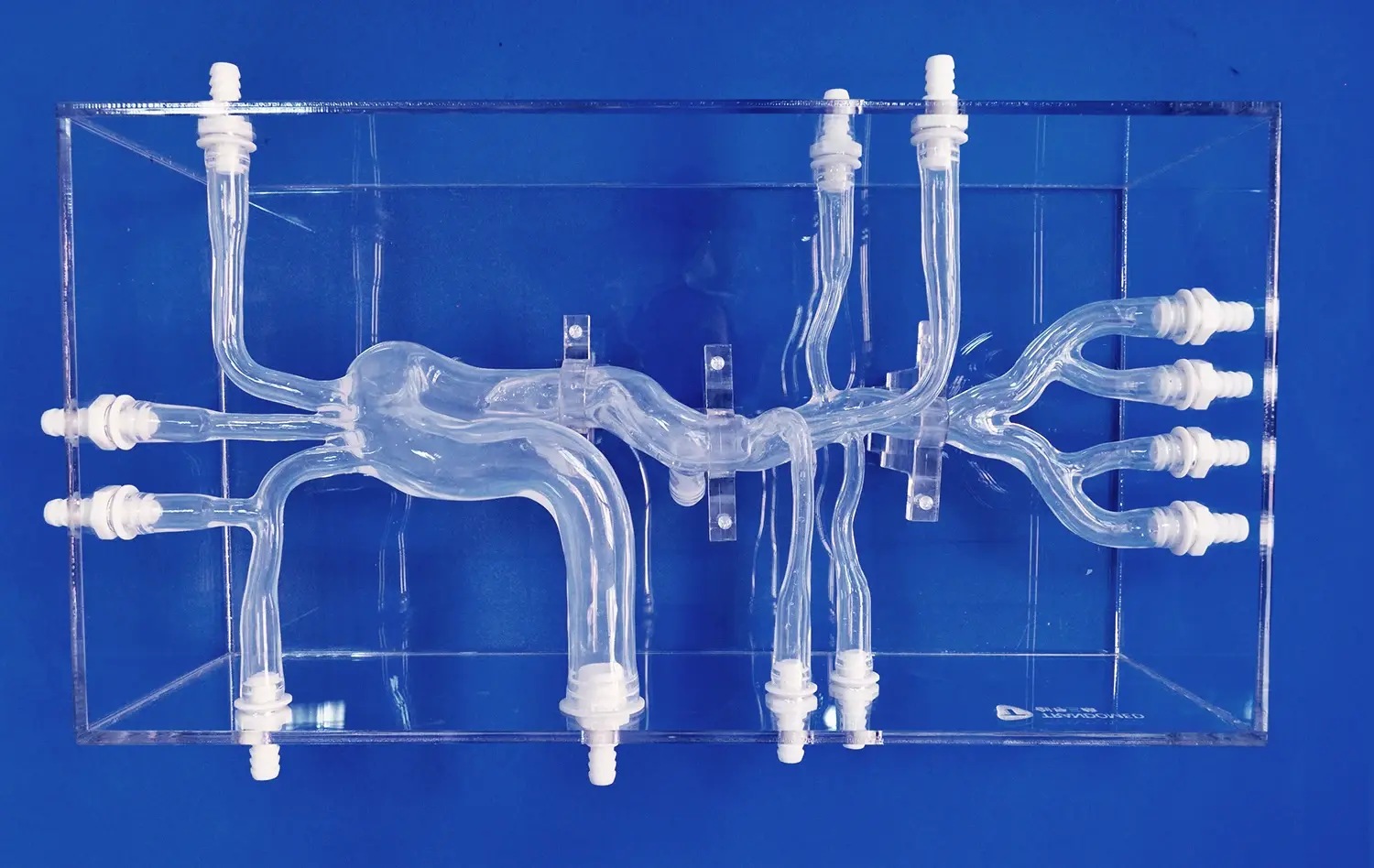
The cornerstone of an effective neuro vascular simulator lies in its ability to faithfully reproduce the intricate details of cerebral vasculature. Advanced 3D printing technologies and sophisticated materials combine to create anatomically correct models that mirror the complexities of real patient cases. These simulators incorporate varying aneurysm morphologies, including saccular, fusiform, and wide-necked configurations, allowing trainees to encounter a diverse range of scenarios they might face in clinical practice.
The attention to detail extends beyond the aneurysm itself, encompassing the surrounding vasculature with accurate vessel diameters, angles, and tortuosity. This level of fidelity ensures that interventionalists can practice navigating through challenging access routes, much like they would in a real procedure. The inclusion of realistic vessel wall properties and tissue responses further enhances the training experience, providing tactile feedback that closely mimics that of live patients.
Customizable Pathologies for Comprehensive Training
One of the most valuable aspects of modern neuro vascular simulators is their ability to be customized. Educators can create specific pathological scenarios, tailoring the training experience to focus on particular challenges or rare cases. This customization extends to creating patient-specific models based on actual imaging data, allowing for pre-procedural planning and rehearsal of complex cases.
The simulator's versatility enables the representation of various aneurysm locations, including those in the anterior and posterior circulation. Trainees can practice approaching aneurysms in different segments of the cerebral vasculature, each presenting unique challenges in terms of access and treatment strategy. This comprehensive approach ensures that interventionalists are well-prepared for the diverse array of cases they may encounter in their clinical practice.
Beyond the Basics: Advanced Techniques for Complex Aneurysm Embolization on the Simulator
Mastering Endovascular Techniques
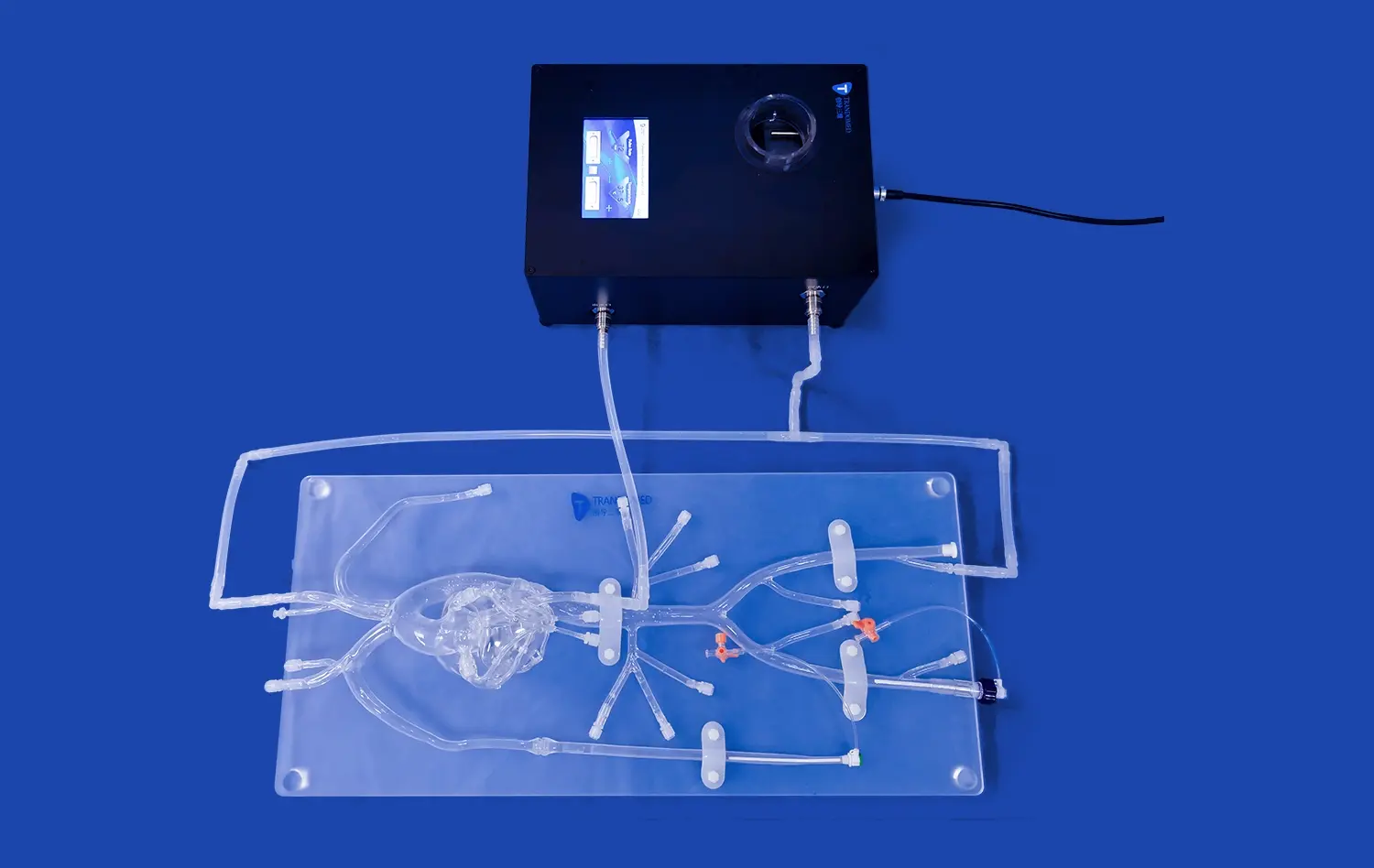
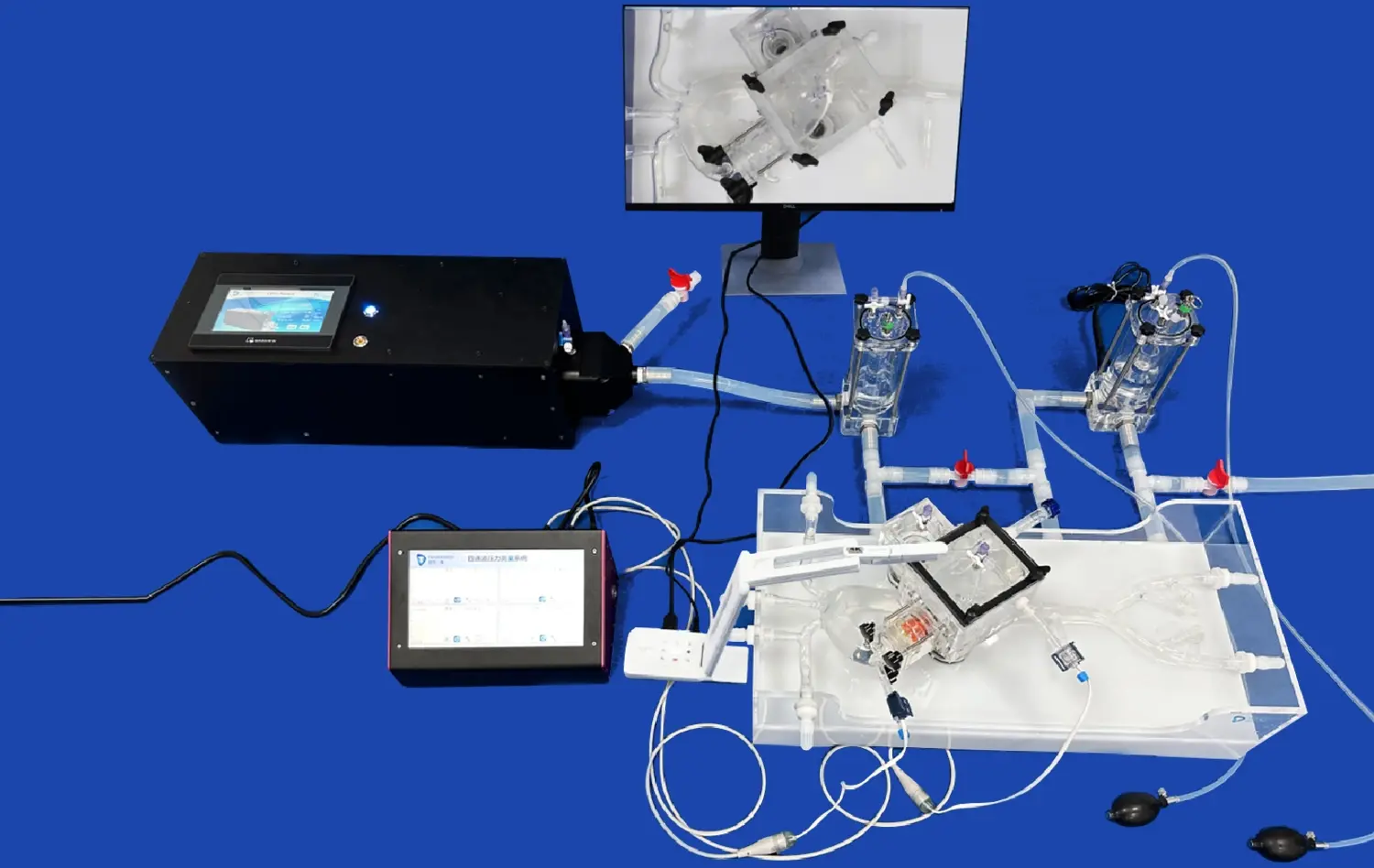
As trainees progress in their skills, the neuro vascular simulator provides an ideal platform for mastering advanced endovascular techniques. The simulator allows for the practice of various embolization methods, including coiling, stent-assisted coiling, and flow diversion. Each of these techniques requires a unique set of skills and understanding of device behavior within the vasculature.
Coil placement, for instance, demands precise control and an understanding of coil packing dynamics. The simulator offers the opportunity to practice different coiling strategies, such as framing, filling, and finishing, while observing the behavior of coils in various aneurysm geometries. Trainees can experiment with different coil sizes and shapes, learning how to achieve optimal aneurysm occlusion while avoiding complications like coil herniation or parent vessel compromise.
Navigating Complex Scenarios
Advanced neuro vascular simulators also incorporate scenarios that mimic complex clinical situations. These may include wide-necked aneurysms that require stent assistance, bifurcation aneurysms that demand careful device positioning, or giant aneurysms that challenge conventional treatment approaches. By practicing these scenarios, interventionalists can develop strategies for managing difficult cases and improve their decision-making skills.
The simulator also allows for the practice of complication management. Trainees can experience and learn to handle potential procedural complications such as coil migration, thromboembolic events, or vessel perforation in a controlled environment. This aspect of training is crucial for building confidence and competence in managing adverse events that may occur during real procedures.
Visualizing Success: Utilizing the Simulator's Transparent Design for Enhanced Procedure Understanding
Real-time Visualization of Device-Aneurysm Interaction
One of the most innovative features of modern neuro vascular simulators is their transparent design, which offers unprecedented visibility of the embolization process. This transparency allows trainees to observe in real-time how devices interact with the aneurysm and surrounding vasculature. As coils are deployed or flow diverters are positioned, users can visualize the exact placement and conformity of devices within the aneurysm sac.
This visual feedback is invaluable for understanding the nuances of device behavior. Trainees can see how coils pack within an aneurysm, how they interact with the aneurysm wall, and how different coiling techniques affect the overall occlusion. For flow diversion procedures, the transparent model allows observation of how the device expands and conforms to the vessel wall, providing insights into optimal positioning and the importance of wall apposition.
Enhancing Procedural Understanding Through Visual Learning
The transparent design of the neuro vascular simulator serves as a powerful educational tool, bridging the gap between theoretical knowledge and practical application. By providing a clear view of the entire procedure, trainees can develop a deeper understanding of the spatial relationships within the cerebral vasculature and how their actions affect the treatment outcome.
This visual learning experience is particularly beneficial for grasping complex concepts such as the impact of vessel anatomy on device selection and deployment strategy. Trainees can observe how the curvature of vessels affects catheter navigation and device delivery, leading to a better appreciation of the importance of choosing appropriate devices and techniques for each unique anatomical situation.
Conclusion
The neuro vascular simulator has revolutionized aneurysm embolization training, offering a safe and effective platform for skill development. Its anatomical fidelity, coupled with the ability to practice advanced techniques and visualize procedural outcomes, makes it an invaluable asset in the education of interventional neuroradiologists and neurosurgeons. As technology continues to advance, these simulators will play an increasingly crucial role in preparing the next generation of neurovascular specialists, ultimately leading to improved patient outcomes and safer procedures.
Contact Us
To learn more about our state-of-the-art neuro vascular simulators and how they can enhance your training program, please contact us at jackson.chen@trandomed.com. Let us help you take your aneurysm embolization skills to the next level with our innovative simulation technology.
References
Mascitelli, J. R., et al. (2018). The impact of using a neurovascular simulator on resident training in aneurysm embolization. Journal of Neurosurgery, 129(3), 631-638.
Liebig, T., et al. (2019). Virtual reality simulators for neuroendovascular procedures: a systematic review. Neurosurgical Review, 42(4), 867-875.
Spiotta, A. M., et al. (2020). Impact of a neuroendovascular simulator-based training program on trainee performance: Results of a randomized trial. Journal of NeuroInterventional Surgery, 12(9), 887-892.
Zhao, B., et al. (2017). Evaluation of a virtual reality neurovascular bundle dissection simulation. Neurosurgery, 80(3), 479-485.
Cooke, D. L., et al. (2021). Advanced neuroangiography simulation for neurosurgical training. Neurosurgical Focus, 51(2), E7.
Fargen, K. M., et al. (2019). The emergence of simulation in endovascular neurosurgery training. Journal of Neurointerventional Surgery, 11(5), 439-444.