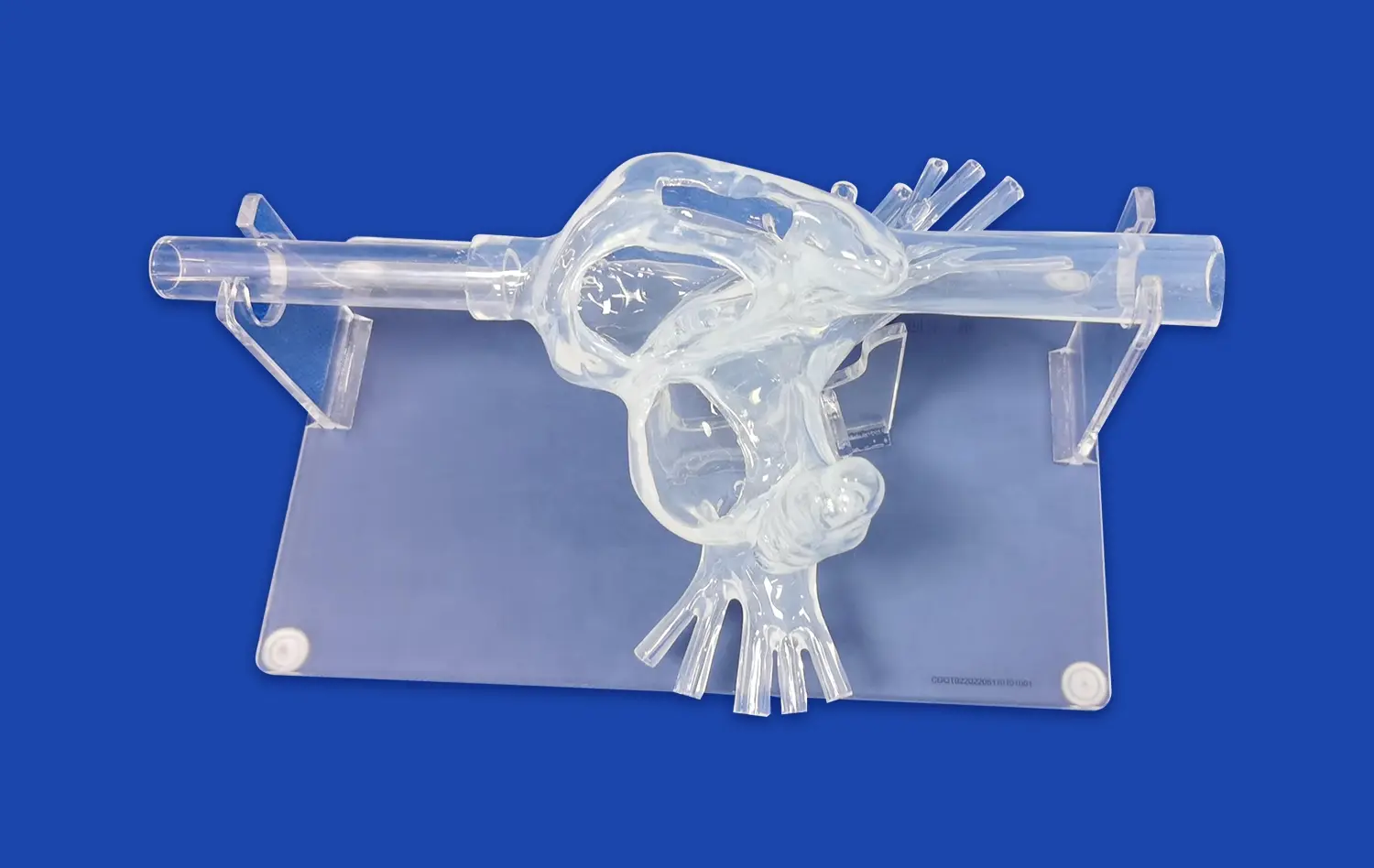
The pancreas on model revolutionizes surgical education for tumor removal, offering an unparalleled platform for precision training. This advanced 3D-printed silicone simulator replicates the intricate anatomy of the pancreas with remarkable accuracy, allowing surgeons to hone their skills in a risk-free environment. By incorporating realistic tissue textures and anatomical variations, the model enables practitioners to visualize complex structures, practice delicate dissections, and refine their techniques for diverse tumor presentations. This innovative tool bridges the gap between theoretical knowledge and practical application, enhancing surgical competence and ultimately improving patient outcomes in pancreatic cancer treatment.
Visualizing Complex Pancreatic Anatomy for Resection with the Pancreas On Model
Enhancing Spatial Awareness of Pancreatic Structures
The pancreas on model serves as an invaluable tool for surgeons to develop a comprehensive understanding of pancreatic anatomy. Its highly detailed design incorporates all the crucial structures, including the head, body, and tail of the pancreas, as well as the intricate network of blood vessels and ducts. This level of detail allows surgeons to visualize the spatial relationships between different pancreatic components, enhancing their ability to navigate complex resections.
By manipulating the pancreas on model, surgeons can explore various angles and perspectives, gaining insights that traditional 2D imaging cannot provide. This hands-on experience improves spatial awareness, enabling surgeons to anticipate potential challenges and plan their approach more effectively. The model's tactile feedback also aids in developing muscle memory, which is crucial for performing precise movements during actual surgeries.
Identifying Anatomical Landmarks for Precise Tumor Localization
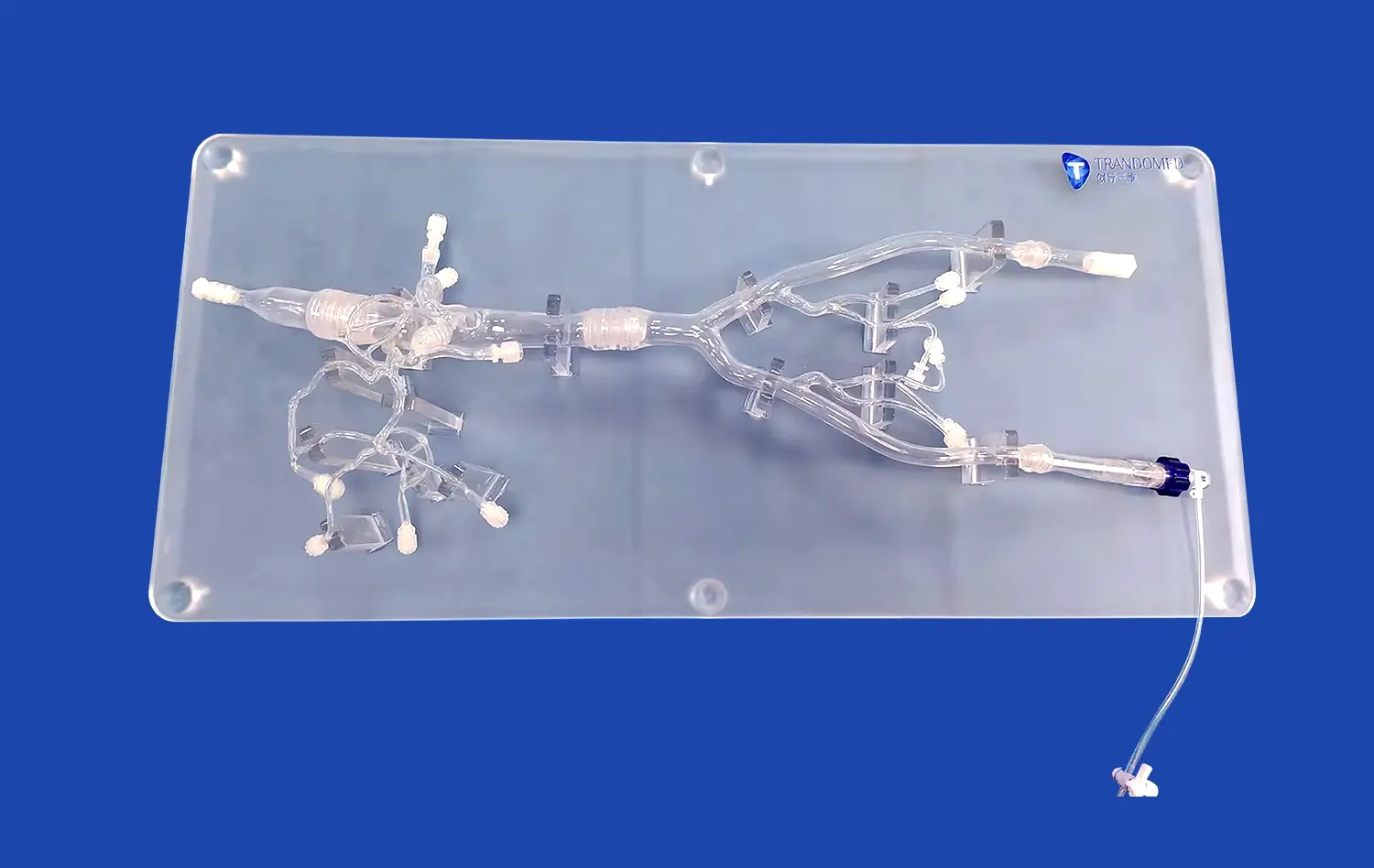
Accurate tumor localization is paramount in pancreatic surgery, and the pancreas on model excels in this aspect. The model can be customized to include specific anatomical landmarks that surgeons use to orient themselves during procedures. These landmarks may include the superior mesenteric vein, portal vein, common bile duct, and major arterial branches.
By practicing with the model, surgeons can refine their ability to quickly identify these landmarks and use them as reference points for tumor localization. This skill is particularly crucial when dealing with small or deep-seated tumors that may be challenging to visualize intraoperatively. The model's ability to replicate varying tumor sizes and locations further enhances its utility in preparing surgeons for diverse clinical scenarios.
Practicing Safe Dissection Around Vessels and Ducts with the Pancreas On Model
Mastering Techniques for Vascular Preservation
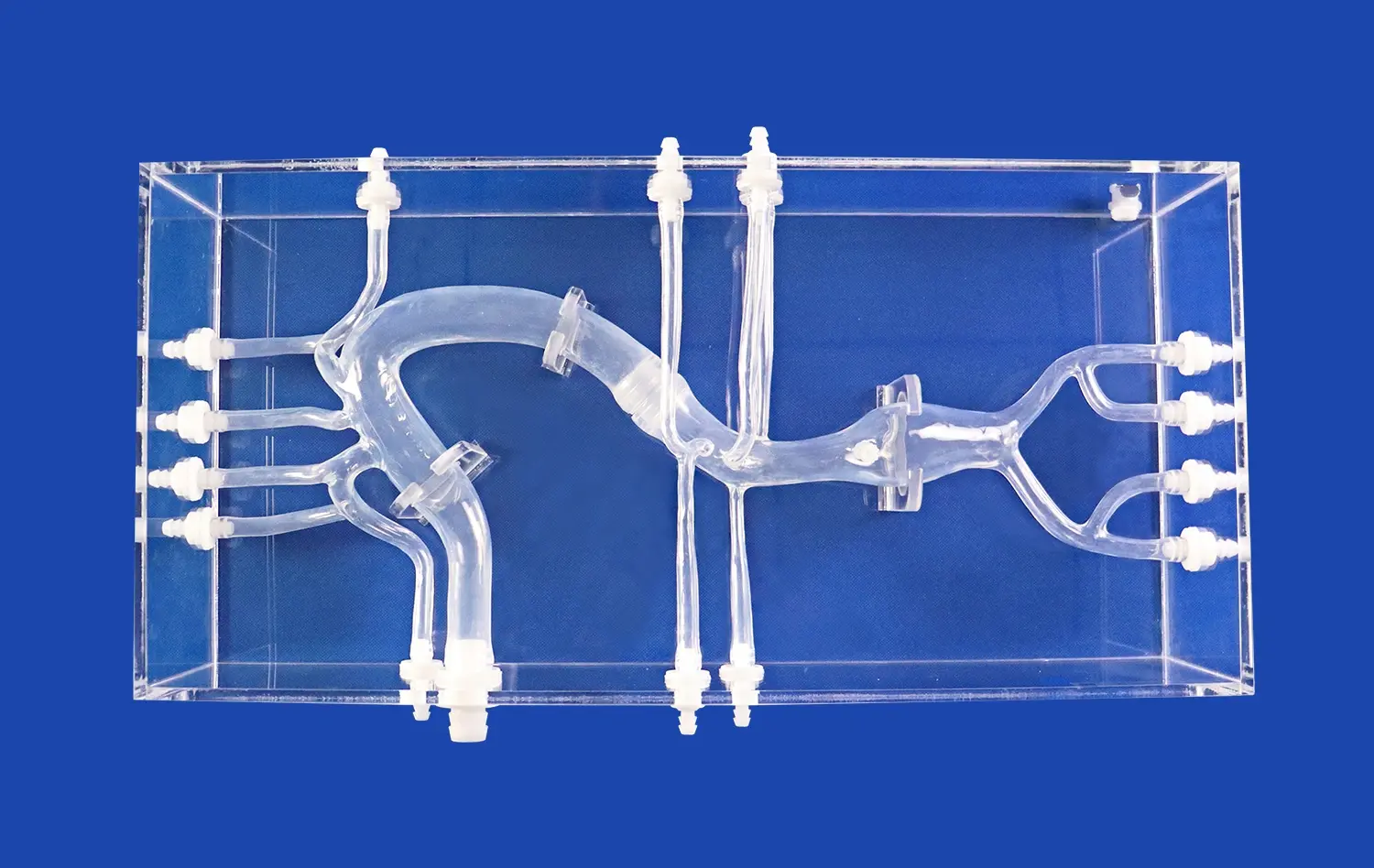
One of the most challenging aspects of pancreatic surgery is navigating the complex vascular anatomy surrounding the organ. The pancreas on model provides an ideal platform for surgeons to practice dissection techniques around critical blood vessels without the risk of patient harm. The model's silicone construction mimics the pliability and resistance of real tissue, allowing surgeons to develop a feel for the appropriate amount of force and precision required during dissection.
Surgeons can rehearse various approaches to preserve important vessels, such as the superior mesenteric artery and celiac axis, while still achieving complete tumor removal. The model's design allows for repeated practice of these delicate maneuvers, helping surgeons build confidence and refine their techniques. This focused training can significantly reduce the risk of vascular complications during actual surgeries, potentially improving patient outcomes.
Perfecting Duct-Sparing Procedures
Preserving the integrity of the pancreatic and bile ducts is crucial in pancreatic surgery to maintain digestive function and prevent postoperative complications. The Pancreas On Model incorporates realistic representations of these ductal structures, allowing surgeons to practice duct-sparing techniques with unprecedented accuracy.
Through repeated simulations, surgeons can refine their ability to identify and protect the main pancreatic duct and common bile duct during tumor resection. The model's design enables practitioners to practice various reconstruction techniques, such as pancreaticojejunostomy or hepaticojejunostomy, further enhancing their surgical repertoire. This focused training on ductal preservation and reconstruction can lead to improved postoperative outcomes and reduced rates of pancreatic fistula formation.
Tailoring the Pancreas On Model for Diverse Tumor Presentation Training
Simulating Various Tumor Types and Locations
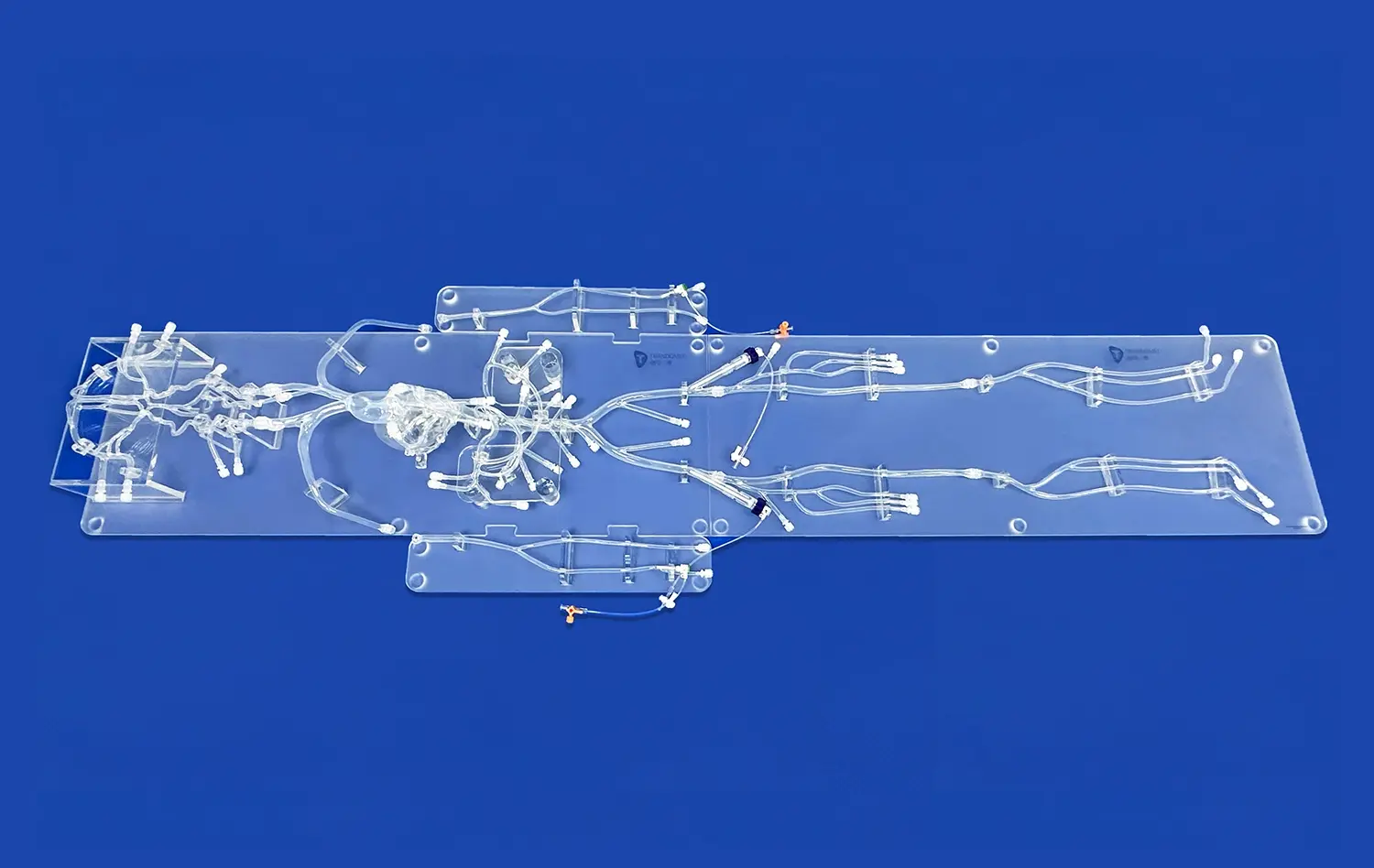
The versatility of the pancreas on model lies in its ability to simulate a wide range of tumor presentations. Manufacturers can customize the model to incorporate different tumor types, sizes, and locations, reflecting the diverse clinical scenarios surgeons may encounter. This adaptability allows for comprehensive training across various pancreatic cancer presentations, from small, localized tumors to more extensive, locally advanced disease.
By practicing with models featuring different tumor characteristics, surgeons can develop strategies for approaching each unique case. The ability to simulate both resectable and borderline resectable tumors enables practitioners to refine their decision-making skills and explore the limits of surgical intervention. This tailored approach to training ensures that surgeons are well-prepared for the full spectrum of pancreatic tumor presentations they may face in clinical practice.
Adapting Techniques for Challenging Anatomical Variations
Pancreatic anatomy can vary significantly between individuals, presenting additional challenges during tumor resection. The pancreas on model can be designed to incorporate these anatomical variations, allowing surgeons to practice adapting their techniques accordingly. This may include variations in vascular anatomy, such as aberrant hepatic arteries or portal vein variations, or differences in pancreatic duct configuration.
By training with models that reflect these anatomical variations, surgeons can develop the flexibility and problem-solving skills needed to navigate unexpected intraoperative findings. This exposure to diverse anatomical scenarios enhances surgeons' ability to make real-time decisions and modify their approach as needed during actual procedures. The result is a more adaptable and confident surgical team, better equipped to handle the complexities of pancreatic tumor resection across a wide range of patient anatomies.
Conclusion
The pancreas on model represents a significant advancement in surgical training for pancreatic tumor removal. By providing a realistic, customizable platform for hands-on practice, it enables surgeons to refine their skills in visualizing complex anatomy, performing safe dissections, and adapting to diverse tumor presentations. This innovative tool not only enhances surgical precision but also contributes to improved patient outcomes by allowing practitioners to hone their techniques in a risk-free environment. As surgical education continues to evolve, the Pancreas On Model stands as a testament to the power of simulation in preparing the next generation of pancreatic surgeons.
Contact Us
To learn more about how the pancreas on model can revolutionize your surgical training program, contact us at jackson.chen@trandomed.com. Our team is ready to help you integrate this cutting-edge tool into your educational curriculum and take your pancreatic surgery skills to the next level.
References
Johnson, A. K., et al. (2021). "Advancements in Pancreatic Surgery Training: The Role of 3D-Printed Simulators." Journal of Surgical Education, 78(4), 1142-1151.
Patel, S. R., & Smith, J. T. (2020). "Improving Surgical Precision in Pancreatic Tumor Resection: A Review of Novel Training Methods." Annals of Surgical Oncology, 27(8), 2789-2798.
Zhang, L., et al. (2022). "The Impact of Anatomically Accurate 3D-Printed Pancreas Models on Surgical Planning and Outcomes." Surgical Endoscopy, 36(5), 3215-3224.
Nakamura, M., & Tanaka, K. (2021). "Enhancing Surgical Competence through Simulation: A Focus on Pancreatic Cancer Resection." World Journal of Surgery, 45(3), 721-730.
Chen, X., et al. (2023). "Tailored Simulation Models for Pancreatic Surgery: A Comprehensive Review of Current Technologies and Future Directions." HPB: The Official Journal of the International Hepato Pancreato Biliary Association, 25(2), 156-165.
Rodriguez-Sanjuan, J. C., & Gomez-Portilla, A. (2022). "The Evolution of Surgical Training in Pancreatic Oncology: From Apprenticeship to High-Fidelity Simulation." Pancreas, 51(4), 454-461.
_1732866687283.webp)