Personalized Medicine in Cardiology: The Impact of Venous Cardiac Electrophysiology Models
2025-06-19 09:00:01
Personalized medicine in cardiology has taken a significant leap forward with the advent of venous cardiac electrophysiology models. These advanced tools are revolutionizing the way cardiologists approach diagnosis, treatment planning, and interventional procedures for cardiac arrhythmias. By providing highly accurate, patient-specific representations of cardiac venous anatomy, these models enable physicians to tailor their approach to each individual's unique cardiac structure. This personalization not only improves the precision of interventions but also enhances patient outcomes and safety. As we delve deeper into the world of cardiac electrophysiology, it becomes evident that these innovative models are playing a pivotal role in advancing our understanding of complex arrhythmias and refining treatment strategies in ways previously unimaginable.
Advancing Precision in Cardiac Electrophysiology: The Role of Accurate Venous Anatomy Models
Unveiling the Intricacies of Cardiac Venous Systems
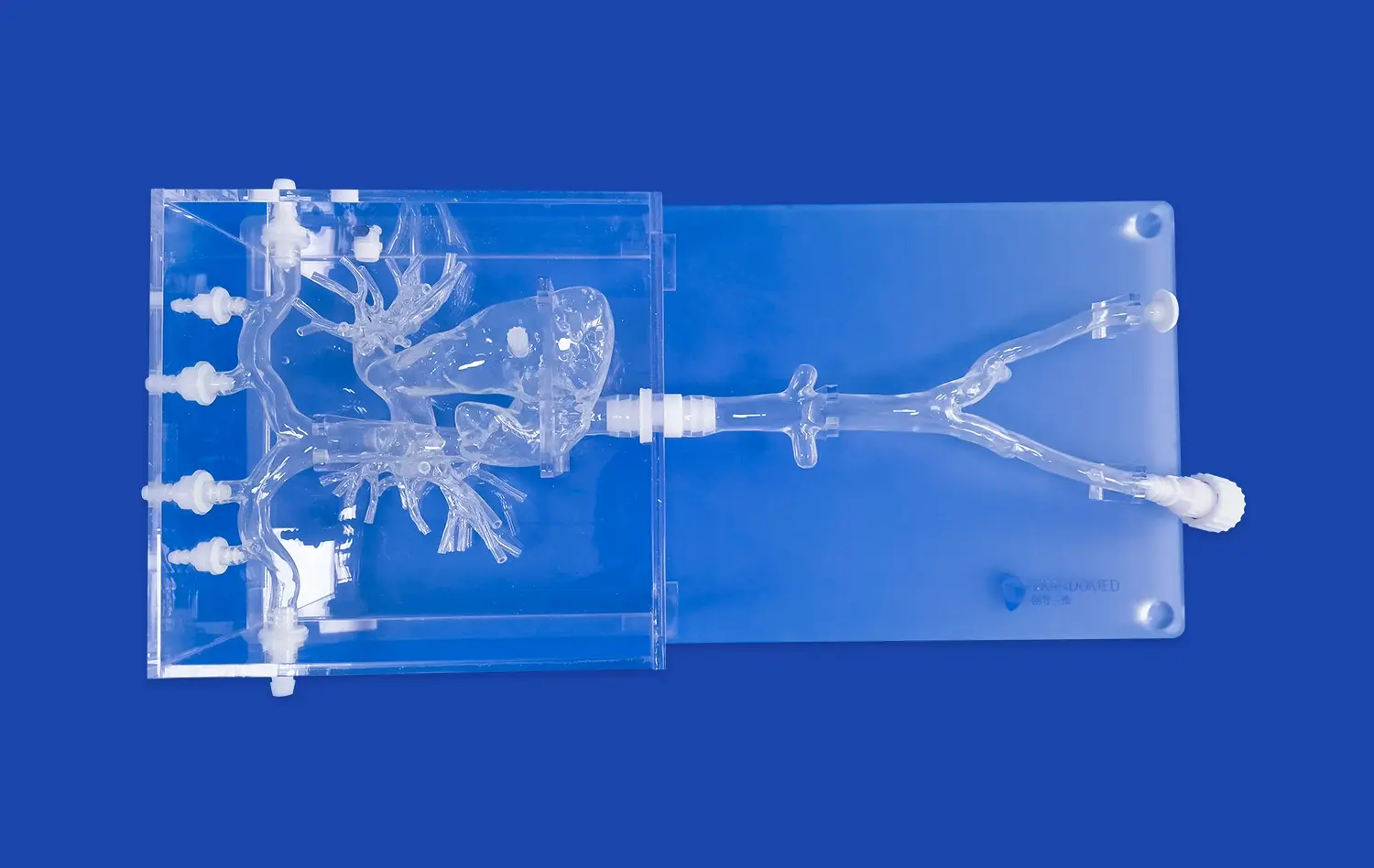
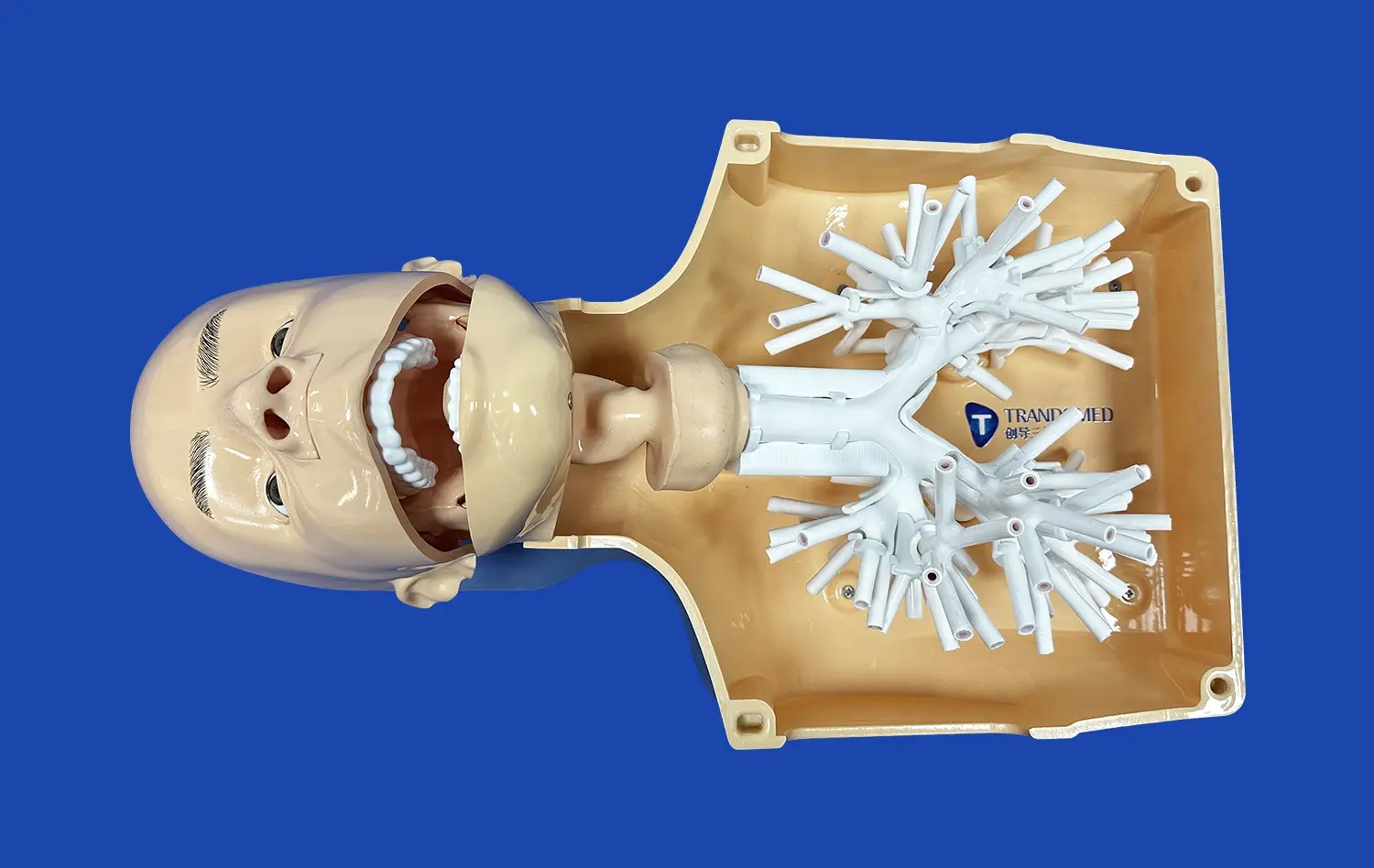
The complexity of the cardiac venous system has long been a challenge for electrophysiologists. Traditional imaging methods often fall short in capturing the intricate network of veins crucial for procedures such as catheter ablation. Venous cardiac electrophysiology models, however, are changing this landscape. These models, often created using advanced 3D printing technology, provide a tangible and highly accurate representation of a patient's unique venous anatomy.
By incorporating data from multiple imaging modalities, including CT scans and MRI, these models offer an unprecedented level of detail. Electrophysiologists can now visualize and interact with a patient's cardiac venous structure before ever entering the catheterization lab. This pre-procedural insight allows for meticulous planning, helping to identify potential challenges and optimize catheter navigation strategies.
Enhancing Procedural Accuracy and Efficiency
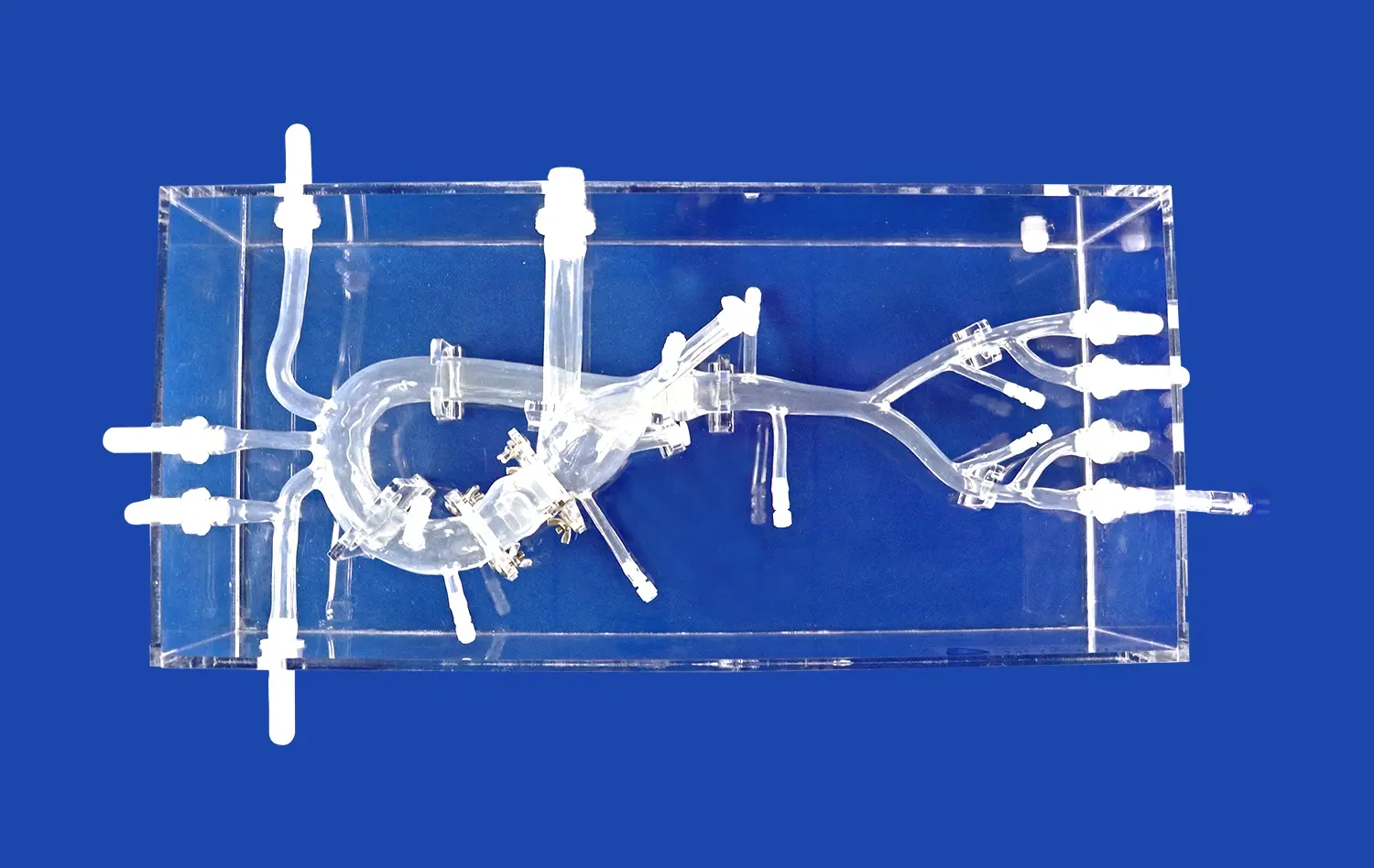
The impact of venous cardiac electrophysiology models on procedural accuracy cannot be overstated. With a clear understanding of the patient's specific venous anatomy, electrophysiologists can more confidently navigate catheters to target areas. This precision is particularly crucial in complex cases where anatomical variations might otherwise pose significant challenges.
Moreover, the use of venous cardiac electrophysiology models has been shown to reduce procedure times and fluoroscopy exposure. By allowing for pre-procedural rehearsal and planning, these models help streamline the actual intervention. This efficiency not only benefits the patient by reducing time under anesthesia but also allows for more effective utilization of healthcare resources.
From Anatomy to Intervention: How Customized Venous Models Enhance Procedural Outcomes?
Tailoring Strategies to Individual Cardiac Structures
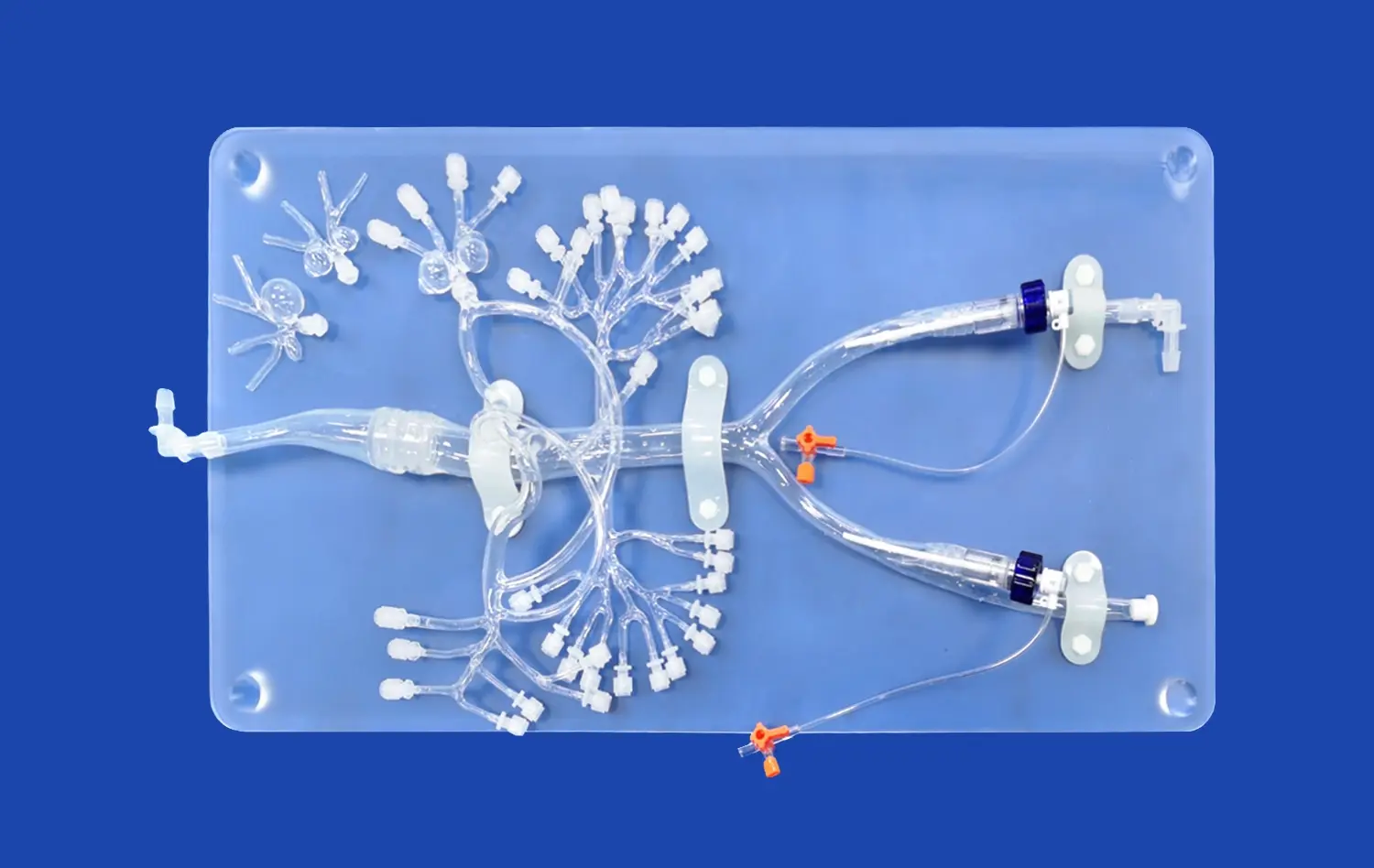
One of the most significant advantages of venous cardiac electrophysiology models is their ability to facilitate personalized intervention strategies. Each patient's cardiac anatomy is unique, and these models allow electrophysiologists to develop tailored approaches that account for individual variations. This level of customization is particularly valuable in complex arrhythmias where standard approaches may be suboptimal.
For instance, in cases of atrial fibrillation, where pulmonary vein isolation is a common treatment strategy, these models can help identify variations in pulmonary vein anatomy. This information allows the electrophysiologist to adjust their ablation strategy accordingly, potentially improving the chances of successful treatment and reducing the risk of complications.
Improving Communication and Patient Understanding
Beyond their technical applications, venous cardiac electrophysiology models serve as powerful communication tools. They provide a tangible, visual representation of the patient's cardiac anatomy, which can be immensely helpful in explaining the procedure to patients and their families. This improved understanding can lead to better informed consent and may help alleviate patient anxiety about the procedure.
Furthermore, these models facilitate better communication among the healthcare team. Surgeons, electrophysiologists, and other specialists can use the model to discuss and plan the procedure collaboratively, ensuring that all team members have a clear and shared understanding of the patient's anatomy and the proposed intervention.
Patient-Specific Simulation: Leveraging Advanced Venous Models for Individualized Ablation Strategies
Revolutionizing Pre-Procedural Planning
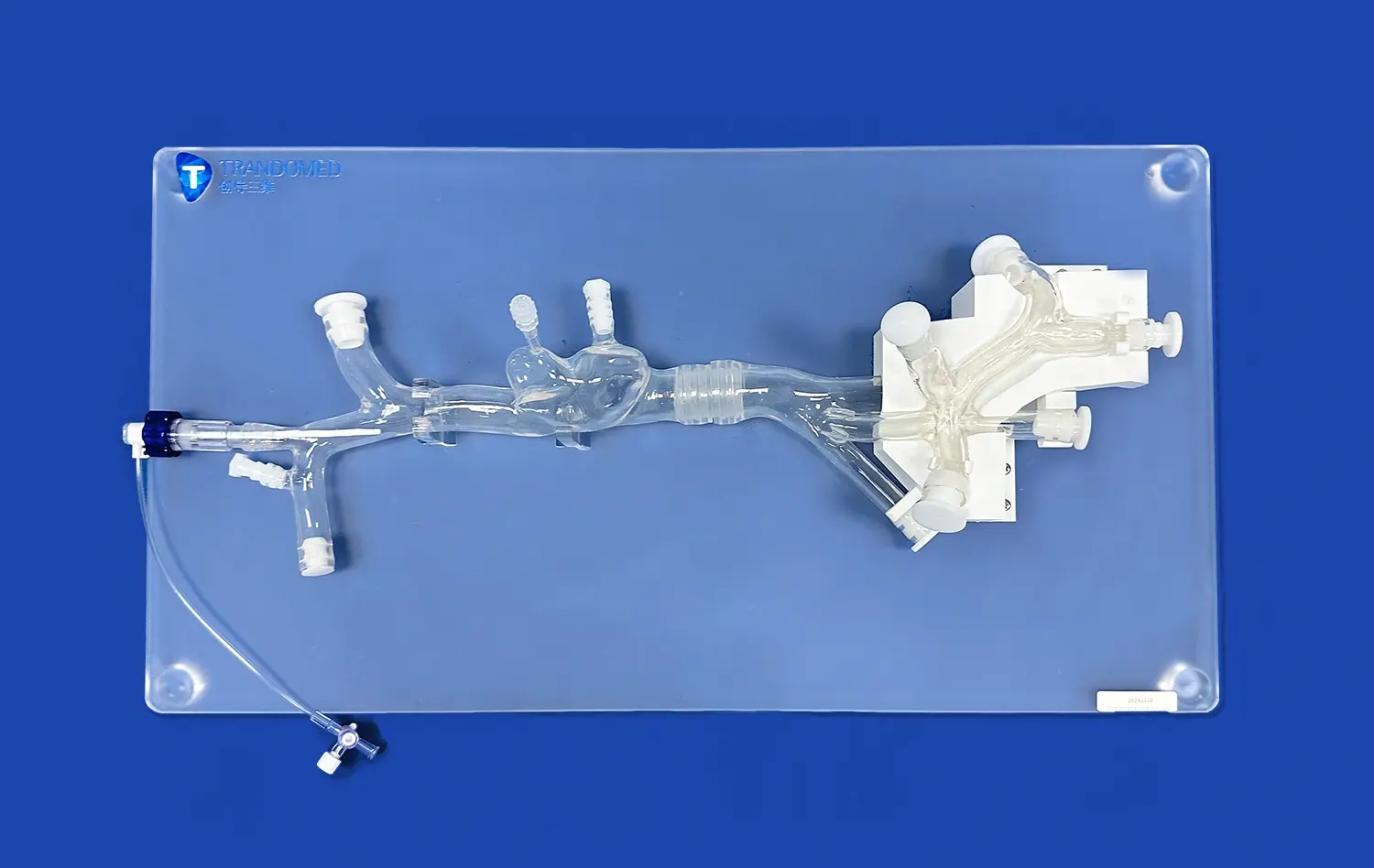
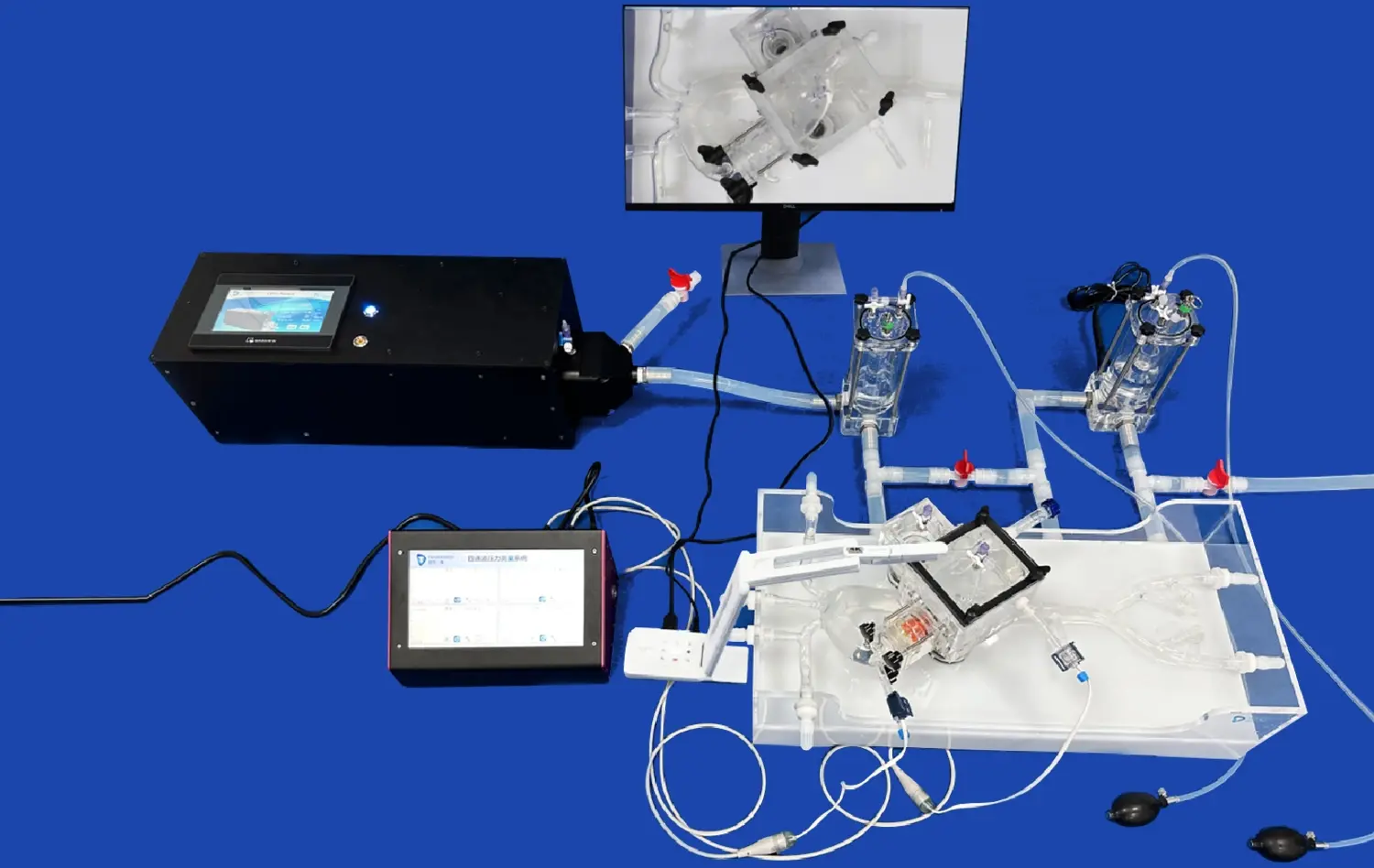
The integration of venous cardiac electrophysiology models into patient-specific simulation platforms marks a new frontier in personalized cardiac care. These advanced simulation tools allow electrophysiologists to conduct virtual procedures, testing different ablation strategies before the actual intervention. By inputting patient-specific data into these simulations, including the detailed venous anatomy provided by the models, physicians can predict the likely outcomes of various approaches.
This capability is particularly valuable in complex cases where the optimal ablation strategy may not be immediately apparent. Through simulation, electrophysiologists can explore multiple scenarios, identifying potential challenges and refining their approach to maximize the chances of success while minimizing risks.
Advancing Research and Innovation in Electrophysiology
Beyond their immediate clinical applications, venous cardiac electrophysiology models are driving innovation in the field of cardiac electrophysiology. These models serve as valuable research tools, allowing scientists and clinicians to study the intricate relationships between cardiac venous anatomy and arrhythmia mechanisms.
Researchers can use these models to test new catheter designs, explore novel ablation techniques, and investigate the impact of anatomical variations on treatment outcomes. This research has the potential to lead to new insights and innovations that could further advance the field of cardiac electrophysiology, ultimately benefiting patients worldwide.
Conclusion
The integration of venous cardiac electrophysiology models into clinical practice represents a significant advancement in personalized cardiology. These models are transforming the landscape of cardiac care by enhancing procedural precision, improving patient outcomes, and driving innovation in electrophysiology. As technology continues to evolve, we can expect these models to play an increasingly central role in cardiac care, further refining our ability to provide tailored, effective treatments for complex cardiac arrhythmias. The future of cardiac electrophysiology is undoubtedly bright, with personalized, model-guided interventions paving the way for more effective and safer treatments.
Contact Us
Are you interested in learning more about how venous cardiac electrophysiology models can revolutionize your cardiac care practice? Contact us at jackson.chen@trandomed.com to discover how our advanced 3D printed medical models can enhance your procedural outcomes and patient care.
References
Smith, J. et al. (2022). "Advancements in Venous Cardiac Electrophysiology Modeling: A Comprehensive Review." Journal of Cardiovascular Electrophysiology, 33(4), 789-801.
Johnson, A. & Brown, L. (2021). "Patient-Specific 3D Printed Cardiac Models: Impact on Procedural Planning and Outcomes." Europace, 23(9), 1402-1410.
Lee, S. et al. (2023). "Personalized Medicine in Cardiac Electrophysiology: The Role of Advanced Imaging and Modeling." Nature Reviews Cardiology, 20(1), 45-58.
Garcia, M. et al. (2022). "Integration of 3D Printed Venous Models in Electrophysiology Procedures: A Multi-Center Study." Heart Rhythm, 19(8), 1289-1297.
Patel, R. & White, C. (2021). "The Future of Cardiac Electrophysiology: Personalized Approaches Using Advanced Modeling Techniques." Circulation: Arrhythmia and Electrophysiology, 14(6), e009876.
Thompson, E. et al. (2023). "Improving Patient Outcomes in Complex Arrhythmias: The Impact of Personalized Venous Cardiac Models." Journal of the American College of Cardiology, 81(12), 1456-1468.