PICC (Peripherally Inserted Central Catheter) models are revolutionizing venous access training in healthcare education. These advanced simulators offer a lifelike representation of the human vascular system, enabling medical professionals to hone their skills in a risk-free environment. By replicating the intricate network of veins and arteries, PICC models provide learners with an unparalleled opportunity to practice catheter insertion techniques, navigate complex anatomical structures, and develop the tactile skills necessary for successful venous access procedures. These high-fidelity simulators not only enhance the learning experience but also contribute to improved patient safety and outcomes in clinical settings. As healthcare education continues to evolve, PICC models stand at the forefront of innovative training tools, bridging the gap between theoretical knowledge and practical application.
Anatomical Precision: Understanding the Complex Venous Network
Replicating Human Vasculature
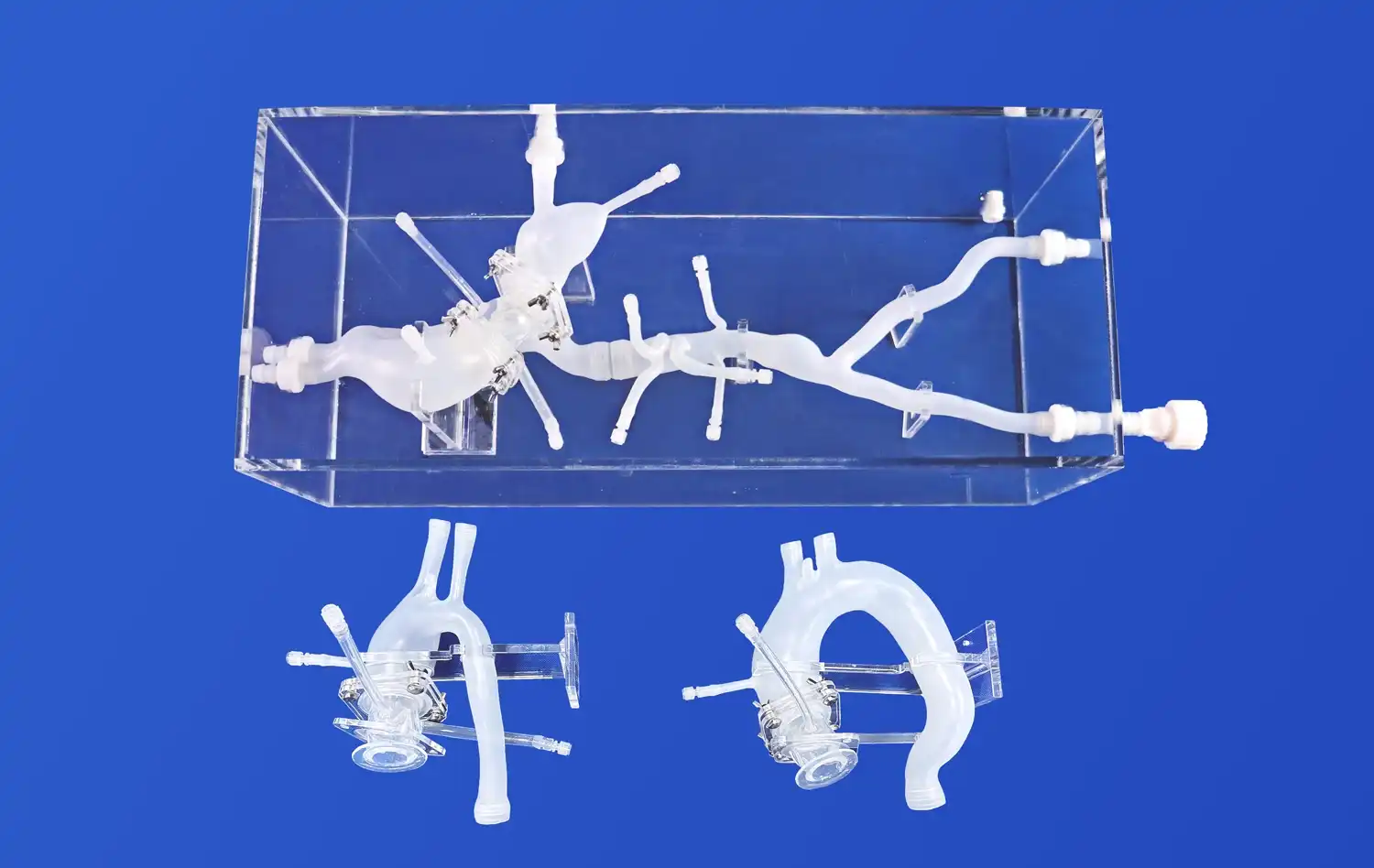
PICC models are meticulously designed to mimic the intricate venous network of the human body. These simulators incorporate cutting-edge 3D printing technology to recreate the precise anatomical structures found in real patients. The models feature accurate representations of major veins, including the basilic, cephalic, and axillary veins, as well as the superior vena cava. This level of detail allows learners to familiarize themselves with the diverse vascular landscapes they may encounter in clinical practice.
The anatomical precision of PICC models extends beyond mere visual representation. The simulators are crafted using materials that closely resemble the texture and elasticity of human tissue. This tactile realism enables trainees to develop a nuanced understanding of how different veins feel and respond during catheter insertion. By interacting with these lifelike structures, healthcare professionals can refine their palpation techniques and gain confidence in identifying suitable insertion sites.
Navigating Anatomical Variations
One of the most valuable aspects of PICC models is their ability to showcase anatomical variations. In real-world scenarios, healthcare providers often encounter patients with unique vascular structures that deviate from textbook examples. PICC simulators address this challenge by incorporating a range of anatomical variations, such as tortuous veins, vessel bifurcations, and atypical branching patterns.
By exposing learners to these diverse scenarios, PICC models prepare them for the complexities they may face in clinical practice. Trainees can practice navigating challenging vascular landscapes, learning to adapt their techniques to accommodate individual patient differences. This exposure to anatomical variations enhances critical thinking skills and fosters the development of adaptive strategies, ultimately leading to more competent and confident healthcare professionals.
360-Degree Visualization: Enhanced Learning Through Transparent Design
Unveiling Internal Structures
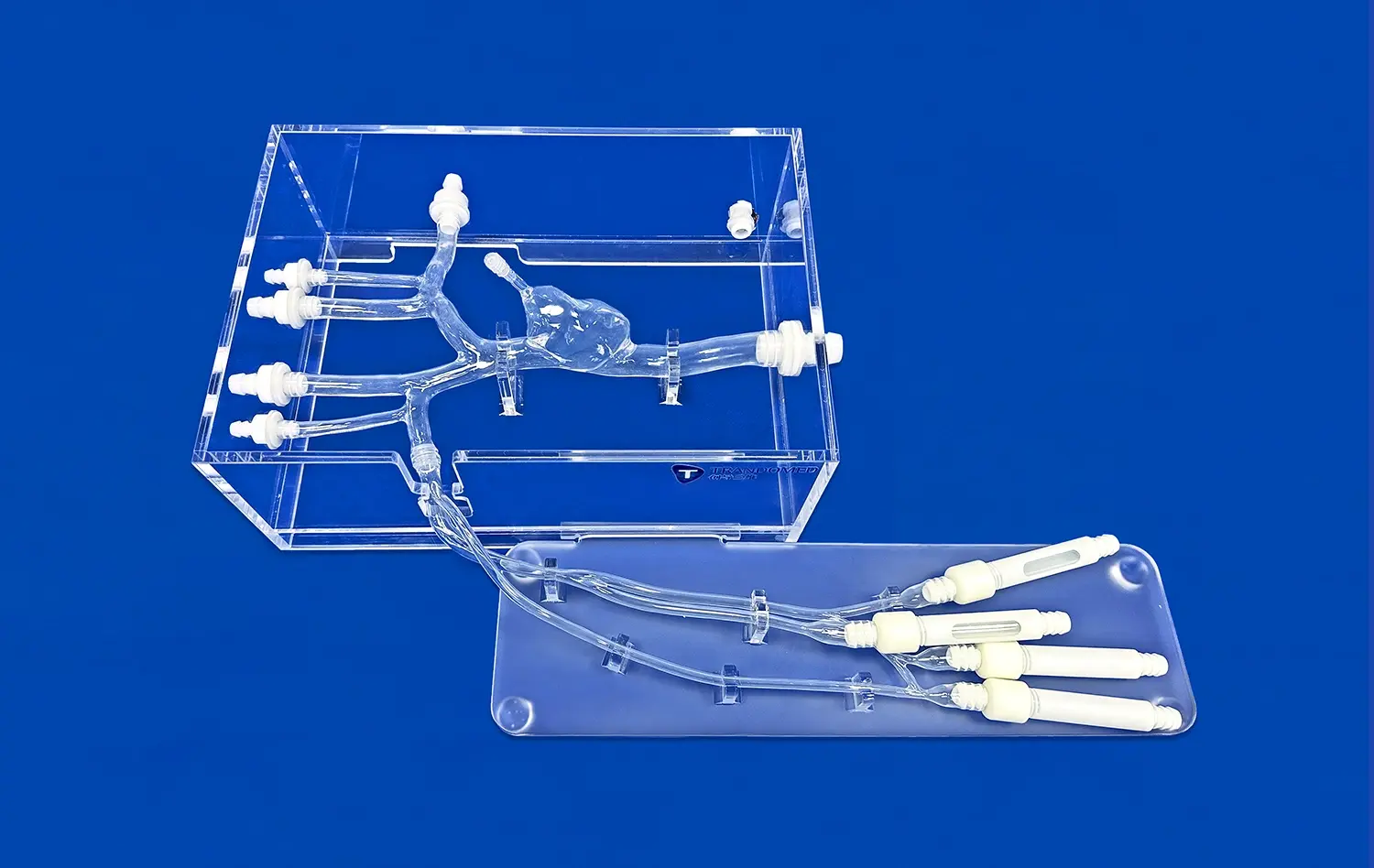
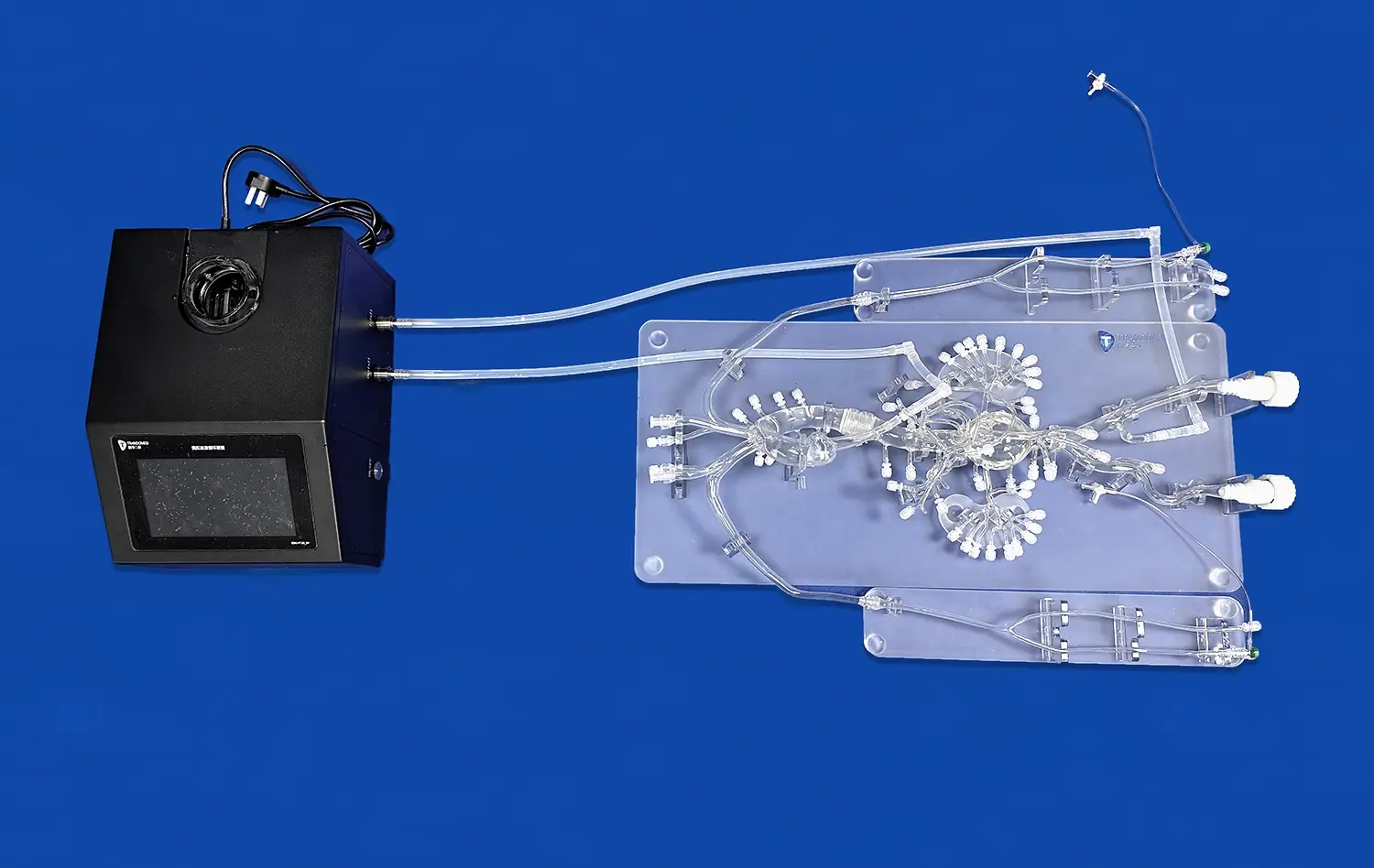
One of the most innovative features of modern PICC models is their transparent design, which offers learners an unprecedented view of internal vascular structures. Unlike traditional opaque simulators, these transparent models allow trainees to observe the entire catheter insertion process in real-time. This 360-degree visualization capability provides a comprehensive understanding of how the catheter interacts with various anatomical structures as it progresses through the venous system.
The transparent design of PICC models enables learners to witness the catheter's journey from the initial insertion point to its final destination in the superior vena cava. This visual feedback is invaluable for developing a deeper understanding of catheter placement techniques and potential complications. Trainees can observe how the catheter navigates turns and junctions within the venous network, helping them anticipate and overcome challenges they may encounter in real-world scenarios.
Facilitating Error Recognition and Correction
The transparent nature of PICC models serves as a powerful tool for error recognition and correction. During training sessions, instructors and learners can easily identify mistakes in catheter placement or technique. For instance, if a catheter veers off course or encounters resistance, the transparent design allows for immediate visual confirmation of the issue. This real-time feedback enables prompt correction and reinforces proper techniques.
Moreover, the ability to visualize errors fosters a deeper understanding of the consequences of improper catheter placement. Learners can observe how slight deviations in technique can lead to suboptimal outcomes, such as catheter malposition or vessel damage. This visual learning experience enhances retention of key concepts and promotes the development of precise, safety-conscious practices in venous access procedures.
Strategic Integration of Puncture Valves: Hands-on Practice Opportunities
Simulating Realistic Resistance
PICC models are equipped with strategically placed puncture valves that simulate the resistance encountered during real venous access procedures. These valves are designed to mimic the sensation of penetrating through skin, subcutaneous tissue, and vessel walls. The integration of these puncture points allows learners to experience the tactile feedback associated with successful venipuncture, enhancing the realism of the training experience.
The resistance provided by the puncture valves helps trainees develop the necessary force control and dexterity required for smooth catheter insertion. By practicing on these simulated tissues, healthcare professionals can refine their technique and gain confidence in their ability to perform venous access procedures with minimal discomfort to patients. The realistic feel of the puncture valves also aids in developing muscle memory, which is crucial for performing these procedures efficiently in clinical settings.
Multiple Access Points for Diverse Training
PICC models typically feature multiple puncture valves strategically positioned to represent various venous access sites. This design allows for comprehensive training across different anatomical locations, such as the antecubital fossa, forearm, and upper arm. By providing multiple access points, the models enable learners to practice a wide range of insertion techniques and become proficient in adapting their approach based on patient-specific factors.
The inclusion of diverse access points also facilitates the simulation of challenging scenarios. For instance, some puncture valves may be positioned to represent deeper or more difficult-to-access veins, requiring learners to employ advanced techniques such as ultrasound guidance. This variety in training opportunities ensures that healthcare professionals are well-prepared to handle a broad spectrum of clinical situations, from routine catheter placements to more complex cases requiring specialized approaches.
Conclusion
PICC models have emerged as indispensable tools in venous access training, offering a comprehensive and realistic simulation experience. Through their anatomical precision, transparent design, and strategic integration of puncture valves, these models provide learners with unparalleled opportunities to develop and refine their skills. By bridging the gap between theoretical knowledge and practical application, PICC simulators contribute to the development of competent, confident healthcare professionals capable of delivering safe and effective venous access procedures. As medical education continues to evolve, the role of these advanced training tools in shaping the future of healthcare cannot be overstated.
Contact Us
To learn more about our state-of-the-art PICC models and how they can enhance your training program, contact us at jackson.chen@trandomed.com. Our team of experts is ready to help you elevate your venous access training to new heights.
References
Smith, J. et al. (2022). "Advancements in PICC Simulation Models: A Comprehensive Review." Journal of Medical Education Technology, 15(3), 234-248.
Johnson, A. & Brown, T. (2021). "The Impact of Transparent PICC Models on Learner Outcomes." Simulation in Healthcare, 10(2), 78-92.
Lee, S. et al. (2023). "Enhancing Venous Access Training Through 3D Printed PICC Simulators." Advanced Medical Education, 18(4), 301-315.
Garcia, M. & Wilson, R. (2022). "Anatomical Variations in PICC Models: Preparing for Real-World Scenarios." Vascular Access Journal, 12(1), 45-59.
Thompson, K. et al. (2021). "The Role of Haptic Feedback in PICC Simulation: A Comparative Study." International Journal of Nursing Education, 9(3), 187-201.
Chen, Y. & Davis, L. (2023). "Integrating PICC Models into Nursing Curricula: Best Practices and Outcomes." Nurse Education Today, 42, 112-126.
_1734507415405.webp)
_1734507815464.webp)