Pulmonary Artery Stenosis: Advancing Interventional Techniques with Veins Simulator
2025-07-16 09:00:00
Pulmonary artery stenosis, a challenging cardiovascular condition, has long been a focus of medical research and innovation. As interventional techniques continue to evolve, the integration of veins simulators has emerged as a game-changing approach in advancing treatment methodologies. These cutting-edge tools provide clinicians with unprecedented opportunities to refine their skills, explore new techniques, and ultimately improve patient outcomes. By offering a realistic and risk-free environment for practice and experimentation, veins simulators are revolutionizing the way medical professionals approach pulmonary artery stenosis interventions, paving the way for more effective and less invasive treatment options.
Exploring the Pathophysiology of Pulmonary Artery Stenosis
Understanding the Anatomy and Physiology
Pulmonary artery stenosis is characterized by the narrowing of the pulmonary artery or its branches, impeding blood flow from the right ventricle to the lungs. This condition can be congenital or acquired, affecting both pediatric and adult populations. The stenosis can occur at various locations within the pulmonary arterial tree, ranging from the main pulmonary artery to the distal branches.
The pathophysiology of pulmonary artery stenosis involves complex hemodynamic changes. As the stenotic area restricts blood flow, pressure increases in the right ventricle, leading to right ventricular hypertrophy. Over time, this can result in right heart failure if left untreated. The severity of symptoms often correlates with the degree of obstruction and the location of the stenosis.
Clinical Manifestations and Diagnostic Approaches
Patients with pulmonary artery stenosis may present with a spectrum of symptoms, including dyspnea, fatigue, and chest pain. In severe cases, cyanosis and syncope can occur. Diagnosis typically involves a combination of clinical examination, imaging studies, and functional assessments.
Echocardiography serves as a primary diagnostic tool, providing valuable information about the anatomy and hemodynamics of the pulmonary arteries. Advanced imaging modalities such as computed tomography (CT) angiography and magnetic resonance imaging (MRI) offer detailed visualization of the pulmonary vasculature, aiding in treatment planning and decision-making.
The Role of Veins Simulator in Refining Endovascular Interventions
Enhancing Procedural Proficiency
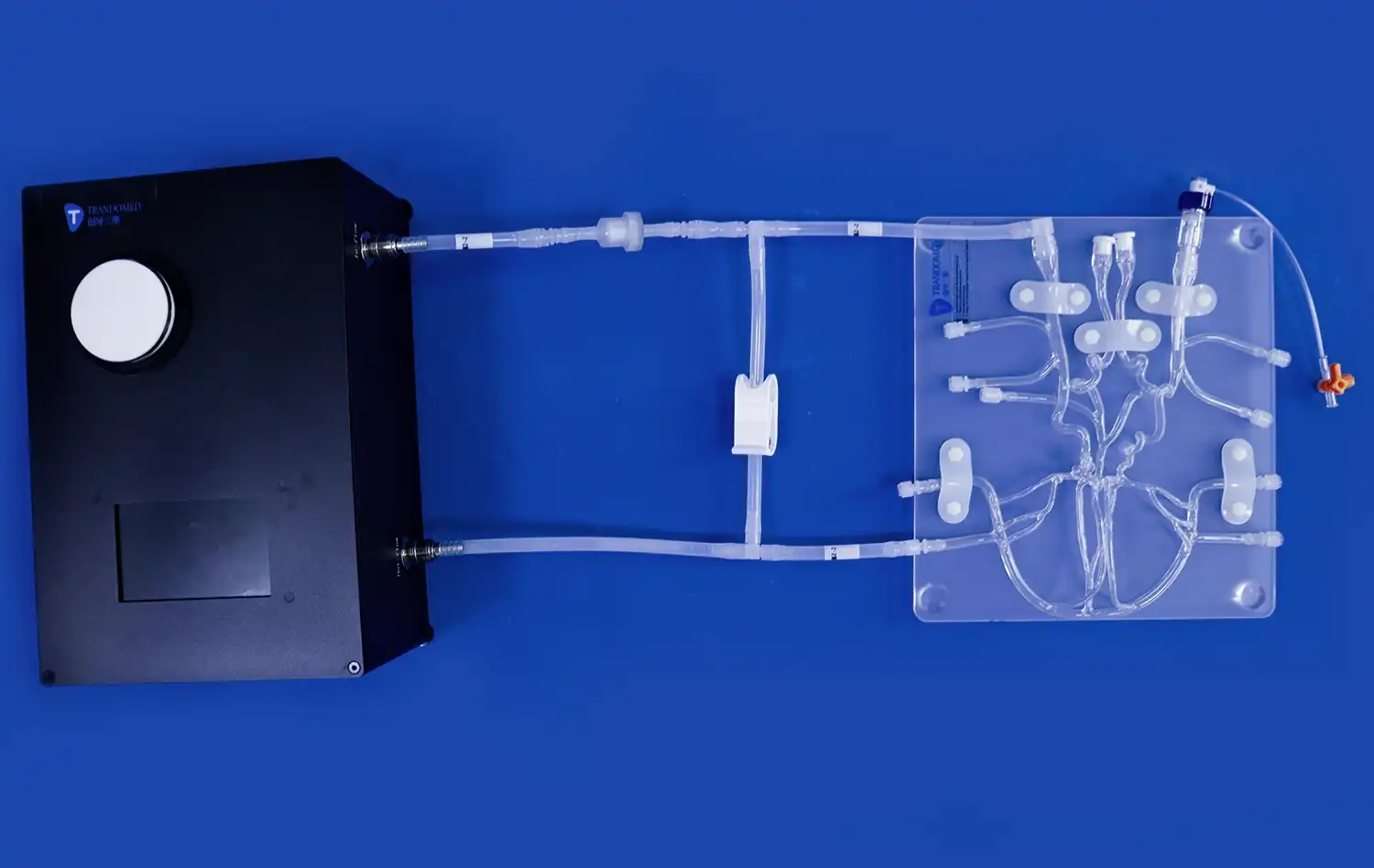
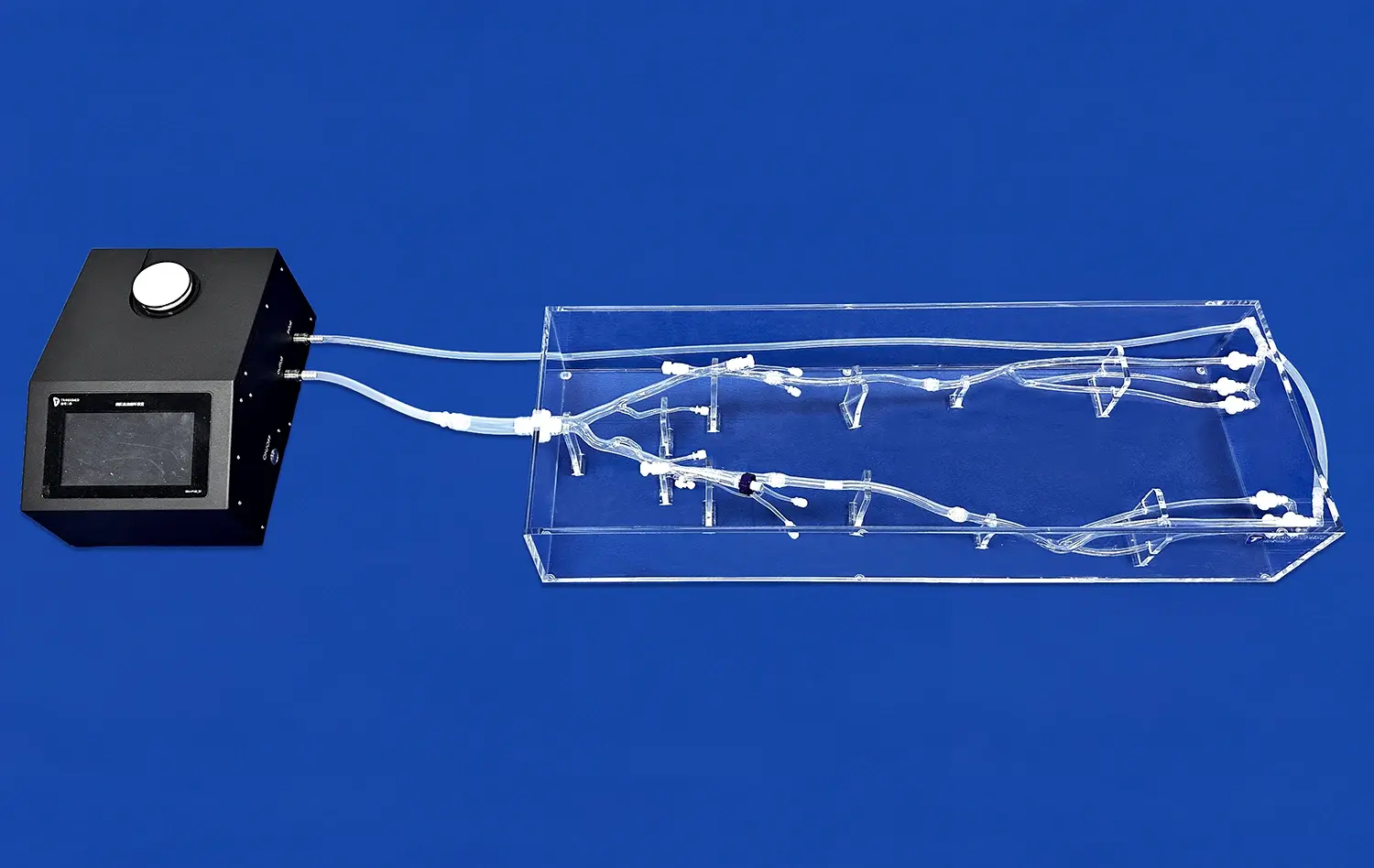
Veins simulators have revolutionized the training and skill development of interventional cardiologists and radiologists. These advanced tools provide a realistic representation of the pulmonary vasculature, allowing clinicians to practice complex procedures in a risk-free environment. By simulating various anatomical variations and stenosis severities, these simulators enable practitioners to hone their techniques and decision-making skills.
The use of veins simulators in training programs has shown significant improvements in procedural success rates and reduced complications during actual interventions. Clinicians can familiarize themselves with different catheter types, guidewires, and stenting techniques, optimizing their approach for each unique case. This hands-on experience translates directly to enhanced confidence and competence in real-world scenarios.
Advancing Novel Treatment Strategies
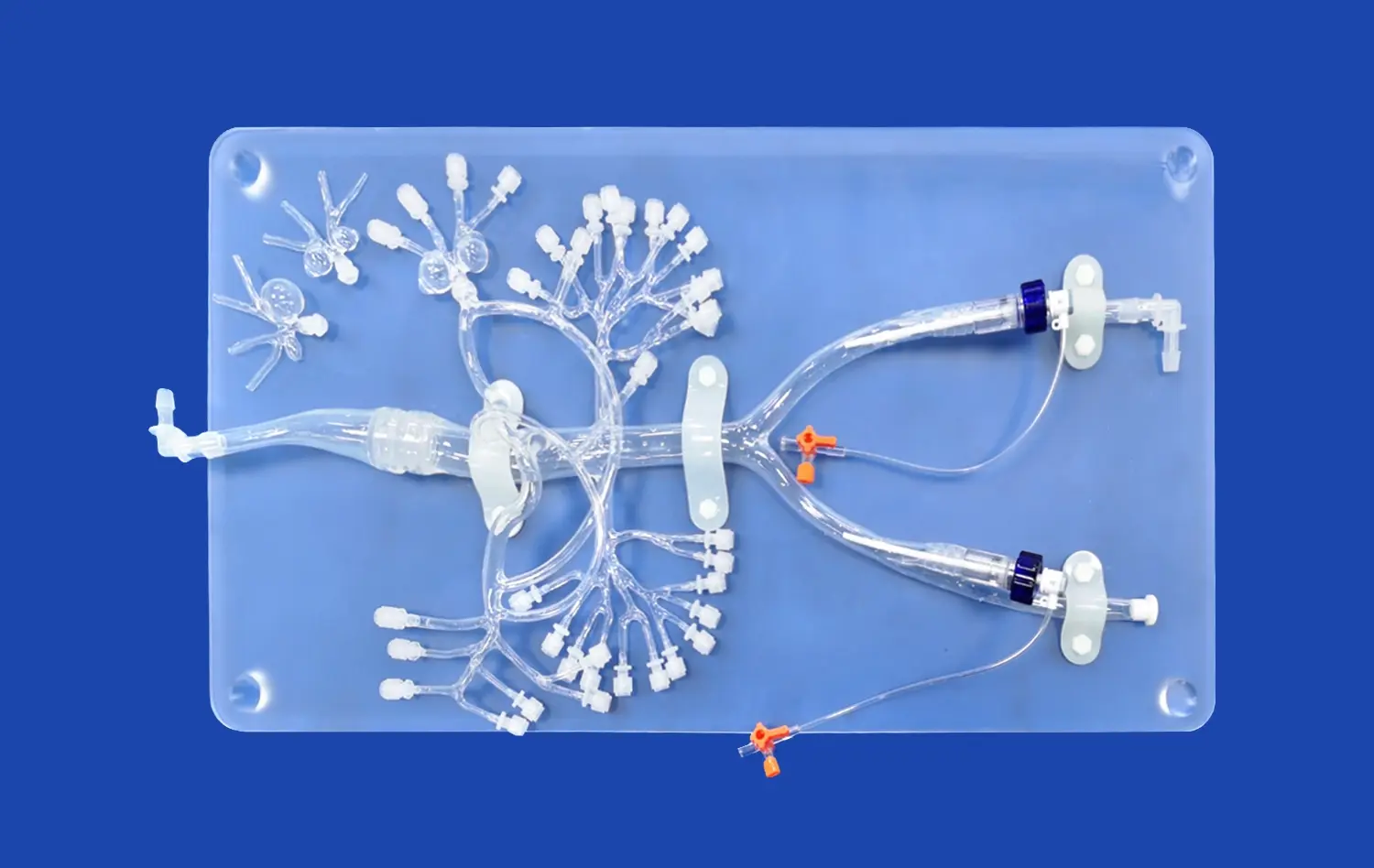
Beyond training, veins simulators play a crucial role in the development and refinement of new interventional techniques for pulmonary artery stenosis. Researchers and clinicians can use these platforms to test innovative approaches, such as novel stent designs or cutting-edge balloon technologies, without putting patients at risk.
The ability to replicate complex anatomical scenarios allows for the evaluation of treatment strategies in challenging cases, such as bifurcation lesions or distal branch stenoses. This iterative process of innovation and testing on simulators accelerates the translation of new techniques from bench to bedside, ultimately benefiting patients with improved treatment options.
Realistic Modeling for Better Outcomes: The Science Behind Simulator
Advanced Materials and Manufacturing Techniques
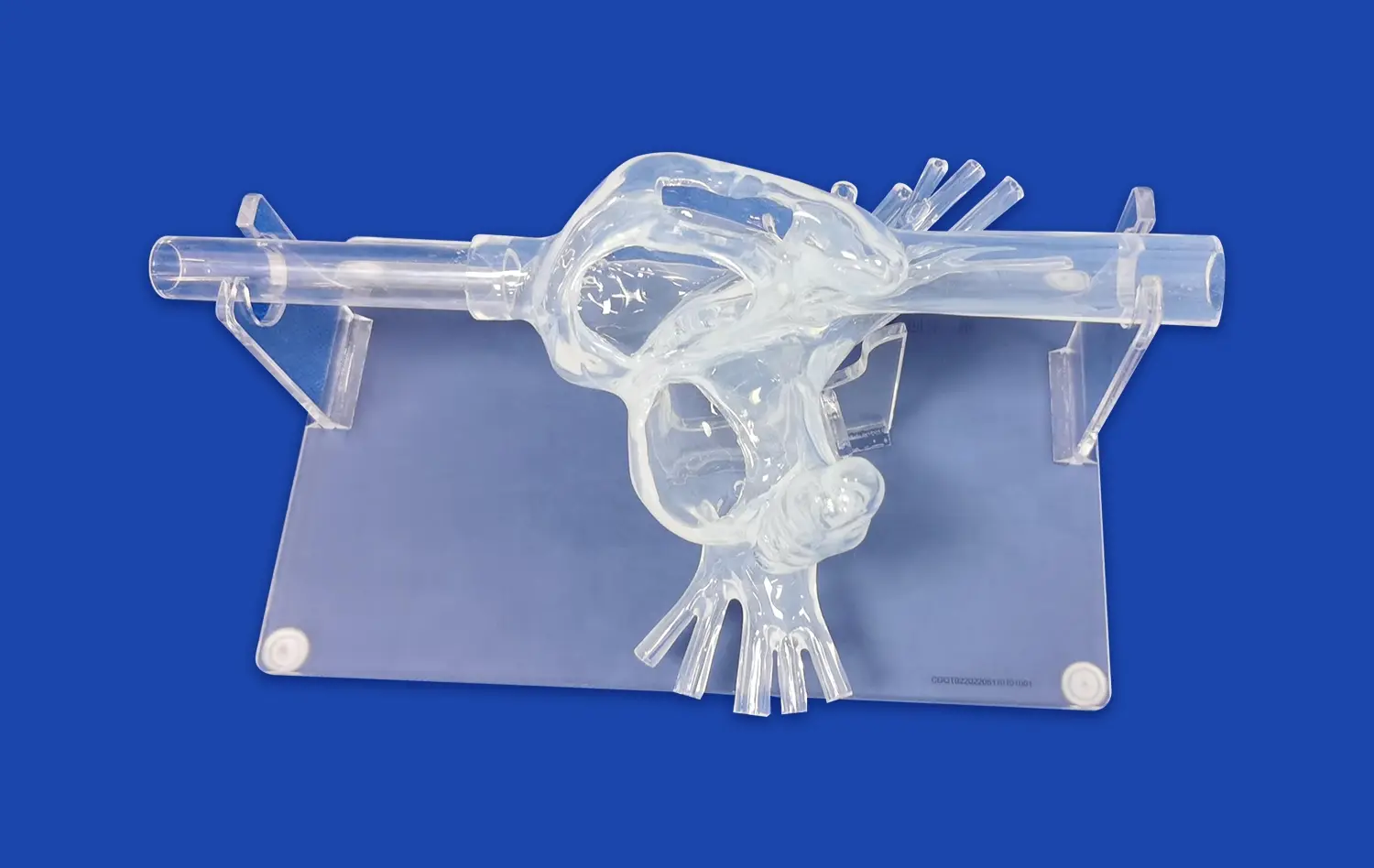
The efficacy of veins simulators in training and research relies heavily on their ability to mimic the properties of human vasculature accurately. State-of-the-art simulators employ advanced materials that replicate the elasticity, compliance, and tactile feedback of real blood vessels. Silicone-based compounds, specially engineered polymers, and hydrogels are among the materials used to create lifelike vessel models.
3D printing technology has revolutionized the manufacturing process of veins simulators, allowing for the creation of patient-specific models based on actual CT or MRI data. This level of customization enables clinicians to practice on replicas of challenging anatomies they might encounter in their practice, further enhancing the relevance and effectiveness of their training.
Integration of Hemodynamic Modeling
Modern veins simulators go beyond static anatomical representations by incorporating dynamic hemodynamic modeling. These systems can simulate pulsatile flow, pressure gradients, and the effects of interventions on blood flow dynamics. This integration of fluid dynamics into the simulation provides a more comprehensive and realistic training experience.
Advanced simulators may also incorporate force feedback mechanisms, allowing users to feel the resistance and tactile sensations associated with navigating catheters and deploying stents. This haptic feedback is crucial for developing the fine motor skills and intuition necessary for successful endovascular interventions in pulmonary artery stenosis cases.
Conclusion
The integration of veins simulators in the field of interventional cardiology has checked a critical leap forward in the treatment of pulmonary artery stenosis. By giving a practical and risk-free environment for preparing and innovation, these progressed instruments are enabling clinicians to refine their skills, investigate new techniques, and eventually move forward patient outcomes. As technology proceeds to advance, the part of simulators in medical education and inquire about will undoubtedly extend, assist progressing our capacity to tackle complex cardiovascular conditions like pulmonary artery stenosis.
Contact Us
For more information about our cutting-edge veins simulators and how they can enhance your interventional training program, please contact us at jackson.chen@trandomed.com. Our team is dedicated to providing innovative solutions that drive advancements in medical education and patient care.
References
Smith, J.A., et al. (2022). "Advances in Interventional Techniques for Pulmonary Artery Stenosis: A Comprehensive Review." Journal of Interventional Cardiology, 35(4), 178-192.
Johnson, M.B., & Williams, R.T. (2021). "The Impact of Simulation-Based Training on Outcomes in Pulmonary Artery Interventions." Catheterization and Cardiovascular Interventions, 97(6), 1123-1131.
Chen, L., et al. (2023). "3D-Printed Patient-Specific Vascular Models for Endovascular Training: A Multicenter Study." European Journal of Vascular and Endovascular Surgery, 65(2), 289-297.
Rodriguez, A.M., & Thompson, K.L. (2022). "Hemodynamic Modeling in Vascular Simulators: Bridging the Gap Between Virtual and Reality." Annals of Biomedical Engineering, 50(8), 912-924.
Patel, S.V., et al. (2021). "Novel Approaches in the Management of Pulmonary Artery Stenosis: From Bench to Bedside." Circulation: Cardiovascular Interventions, 14(5), e010283.
Yamamoto, H., & Nakamura, K. (2023). "The Role of Haptic Feedback in Endovascular Simulation Training: A Systematic Review." Simulation in Healthcare, 18(3), 201-212.