A realistic 3D artery model, which provides anatomically accurate representations of the vascular systems that educators and medical professionals depend on on a daily basis, is a significant advancement in medical simulation. Medical students, interventional specialists, and device manufacturers can practice techniques, validate products, and convey difficult conditions with remarkable clarity thanks to these sophisticated neurovascular simulators that mimic the complex geometry of cerebral arteries. These models alter how institutions approach vascular education and procedural training by bridging the gap between theoretical knowledge and practical clinical competence through the use of state-of-the-art 3D printing technology in conjunction with medical-grade silicone materials.
Understanding Realistic 3D Artery Models: Technology and Applications
Sophisticated fabrication techniques that replicate every anatomical aspect of the human artery system are the foundation of modern vascular simulation. We've seen how these developments have transformed medical education, providing students with something considerably better than stiff plastic prototypes or conventional textbook diagrams. Examining the underlying technology as well as the various applications these models support in various healthcare contexts is necessary to comprehend what makes them effective.
Advanced Materials and Manufacturing Techniques
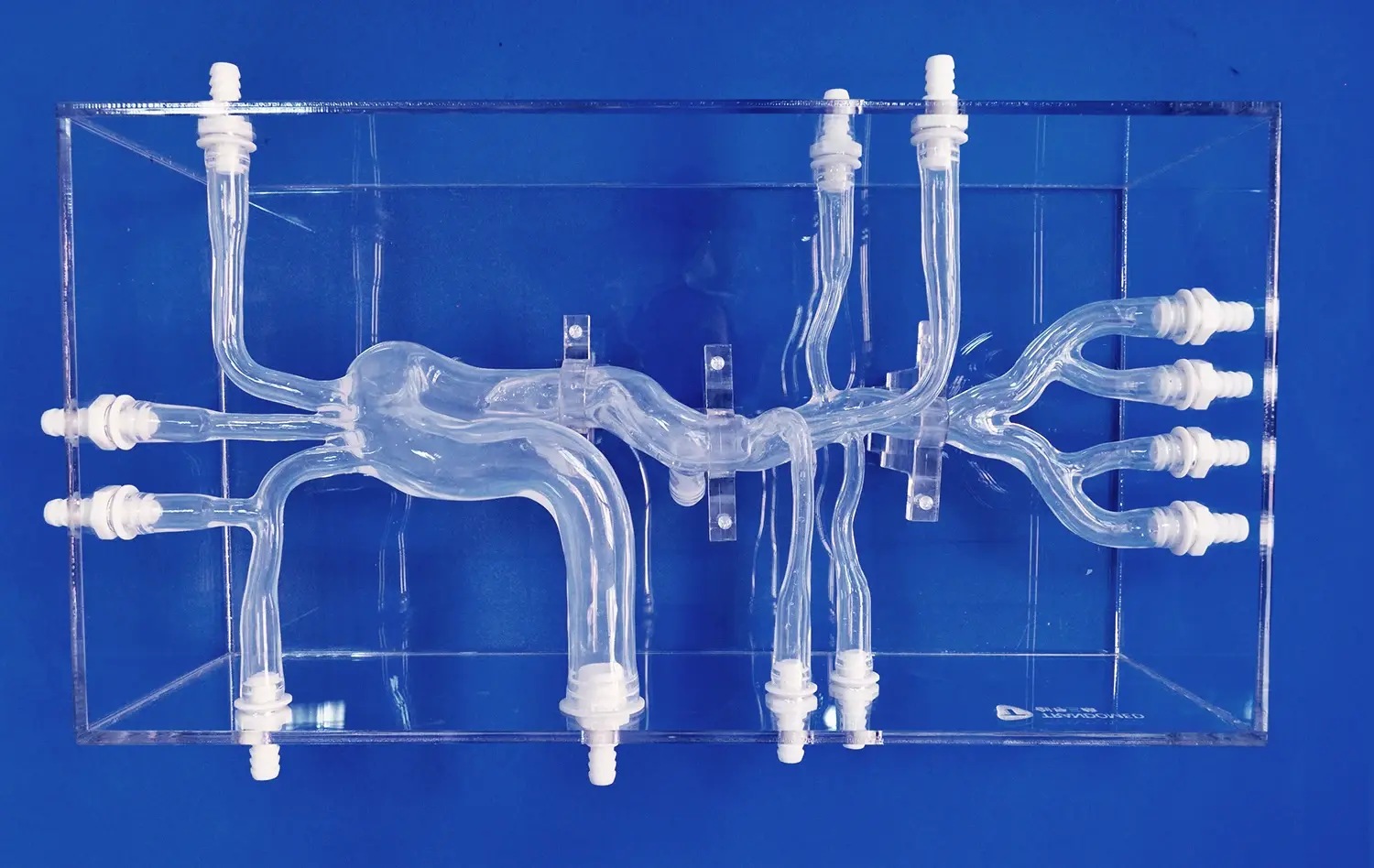
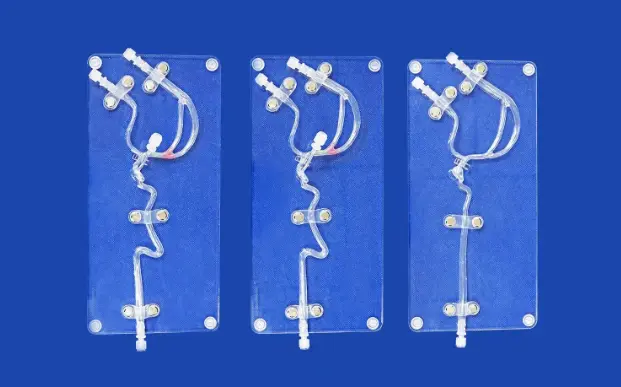
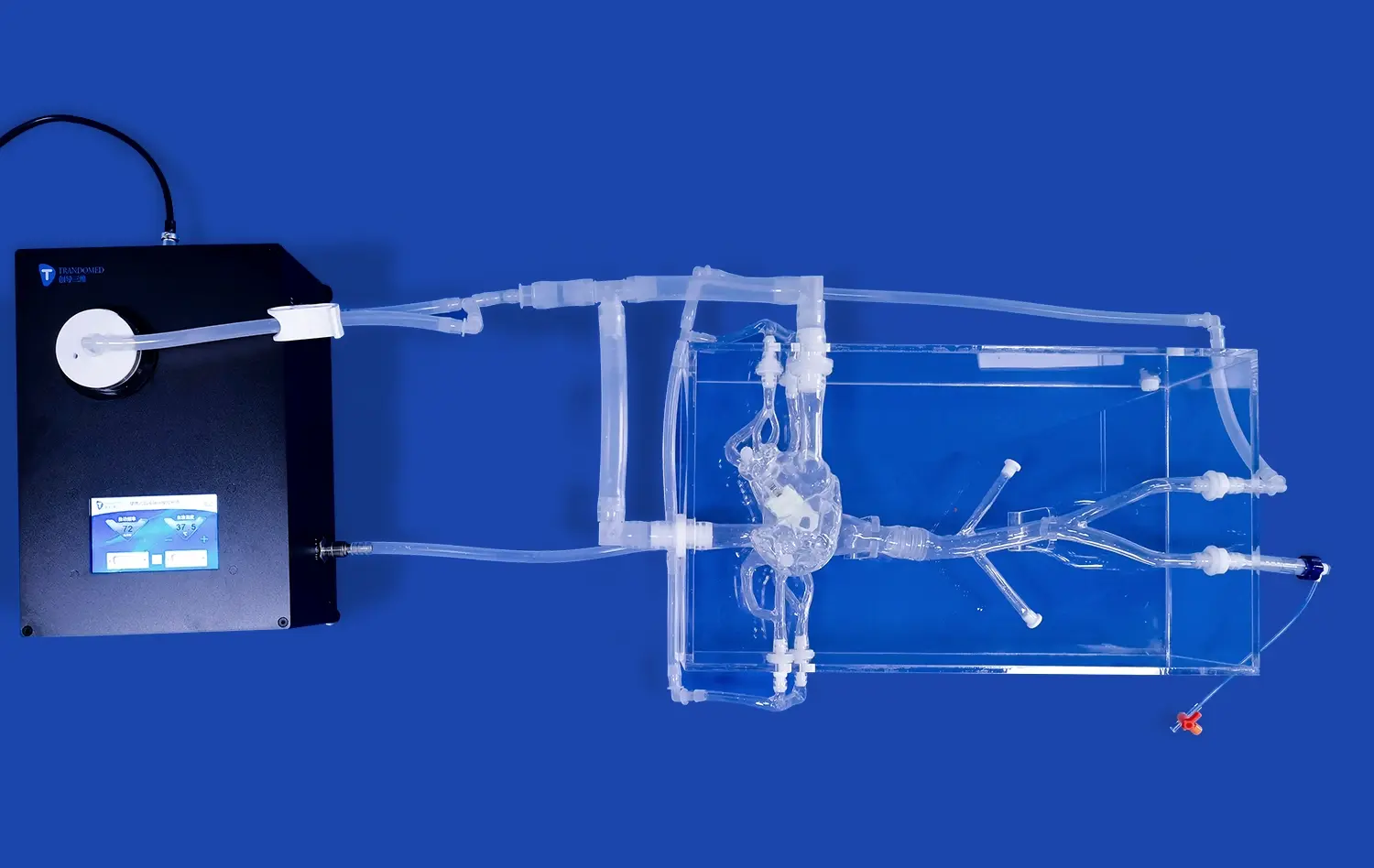
The choice of materials is the first step in building any high-quality cerebral artery simulator. Since Silicone Shore 40A closely resembles the tactile characteristics of human blood arteries, it has become the industry standard for neurovascular models. Catheters and guidewires may pass through the model precisely as they would in a living patient thanks to this particular durometer rating, which strikes the ideal balance between flexibility and structural integrity. Precision 3D printing is used in the production process to replicate the intricate bifurcations, curves, and variances present in real brain circulation.
The ability of modern models to replicate patient-specific anatomy distinguishes them from previous generations. Manufacturers can now produce personalized replicas that represent individual differences in artery tortuosity, aneurysm morphology, and stenotic lesions using medical imaging data from CT scans, MRI studies, or angiography. Surgeons can now physically rehearse their technique before entering the operating room thanks to this customisation feature, which turns surgical planning from an abstract activity into a real rehearsal opportunity.
Clinical Applications in Preoperative Planning
Vascular models have been adopted by hospitals and surgical training labs as vital resources for complex case preparation. A tangible model of the patient's distinct anatomy offers insights that digital imaging alone cannot provide when a neurosurgeon is faced with a difficult aneurysm repair or a delicate carotid endarterectomy. Clinical teams can foresee problems and improve their tactics by manipulating the model, testing various catheter angles, and seeing the spatial correlations between vessels.
These methods support larger quality improvement activities in addition to individual case planning. Standardized vascular replicas are used in simulation-based training programs to evaluate staff proficiency, guarantee uniform procedure across departments, and lessen procedural outcome variability. When compared to observation-only training techniques, research published in medical education publications repeatedly shows that practical experience with accurate anatomical models enhances retention, boosts confidence, and reduces learning curves.
Educational Impact in Medical Schools and Training Centers
Neurovascular simulators such as the 3D artery model have been incorporated into the main curricula of medical schools, nursing schools, and clinical skills centers because they solve a basic problem in healthcare education: giving students enough practice before they interact with real patients. Students can practice recognizing anatomical landmarks, comprehend the three-dimensional interactions between brain vessels, and hone the spatial thinking abilities necessary for interventional treatments by using a middle cerebral artery model.
The educational benefit goes beyond teaching fundamental anatomy. These models are incorporated into simulation exercises in advanced training scenarios that mimic emergency events, such as traumatic vascular injuries, acute stroke interventions, or problems during endovascular treatments. In a safe setting where errors are viewed as teaching opportunities rather than threats to patient safety, residents and fellows develop the muscle memory and reflexes for making decisions that they will need in real clinical situations.
Comparing 3D Artery Models: Traditional vs. Modern Solutions
The transition from traditional teaching aids to modern vascular simulations is indicative of larger technological developments in the medical device industry. Procurement professionals can better understand why investing in contemporary solutions yields quantifiable benefits in clinical outcomes and training efficacy by being aware of these distinctions. When it comes to training healthcare personnel for complicated treatments, the comparison shows not only small but significant advances.
Limitations of Traditional Anatomical Models
Rigid plastic constructs or two-dimensional images that could only roughly depict the intricacy of human anatomy were the mainstay of earlier generations of vascular teaching materials. These conventional models' teaching value was constrained by a number of serious flaws. There was no accurate tactile feedback during catheter manipulation exercises because the materials, which were usually hard plastics or resins, bore no resemblance to actual vascular tissue. Although they studied anatomy in abstract terms, students didn't really understand how vessels react to instruments in real life.
Standardization was another major drawback. The general anatomy shown by traditional models hardly ever represented the anatomical variances that physicians see in their daily work. Although the vascular architecture of each patient varies slightly, students who were only taught on standardized reproductions formed expectations that were difficult to meet in clinical settings. When practitioners started dealing with real cases, the learning curves grew longer due to the mismatch between training models and actual patient anatomy.
Advantages of Contemporary Silicone-Based Simulators
These historical constraints are addressed in contemporary neurovascular models by careful engineering and cutting-edge materials research. The switch to medical-grade silicone produces an experience that is quite similar to working with human tissue. The resistance, flexibility, and feedback that an interventional cardiologist experiences when passing a catheter through a silicone carotid artery replica are similar to those they will experience during real treatments. Practice sessions become real skill-building experiences instead of just abstract exercises because to this genuineness.
Another significant advancement is the ability to customize. These days, we may create models that are suited to particular learning goals or medical situations. Exact aneurysm sizes, locations, and neck geometries may be specified in an aneurysm coiling training program. Vessel widths and curvature angles that correspond to their study protocols can be requested by a research lab investigating novel stent designs. Instead of requiring courses to adjust to model limits, this flexibility guarantees that the training environment properly matches learning objectives.
Value evaluations for a 3D artery model also heavily weigh durability issues. Superior silicone endures frequent use without deteriorating or losing its realistic qualities. Before a model needs to be replaced, training facilities can perform hundreds of practice operations on it, distributing the cost over many students and sessions. These models had a longer lifespan than more conventional options, which frequently displayed wear or damage after only a small amount of use.
Key Selection Criteria for Procurement Decisions
A number of elements should be carefully taken into account while assessing possible providers and particular model offerings. The model must accurately replicate the vascular structures pertinent to your training goals or clinical applications; anatomical accuracy is crucial. Ask for validation data that compares the model's measurements, geometry, and physical characteristics to patient imaging investigations or published anatomical references.
Equal attention should be paid to material attributes. Examine the silicone's performance under several circumstances in addition to its fundamental durometer grade. Does it remain constant as the temperature changes? What is its reaction to various coatings and materials for catheters? If sterilization is required by your protocols, can it survive? Being aware of these features helps you avoid unpleasant surprises after buying.
Reputation and support skills of suppliers are frequently just as crucial as the actual goods. The subtleties of educational and clinical applications are understood by a company with a great deal of experience in medical simulation. They can help you choose a model, customize it to fit your needs, and offer prompt customer support all the way through the product lifecycle. These intangible elements often dictate whether a procurement choice results in long-term benefits or continues to cause aggravation.
Procurement Guide for Realistic 3D Artery Models
It's important to comprehend both the technical requirements that determine quality and the business factors that affect total cost of ownership when navigating the procurement process for specialist medical simulation equipment. Procurement experts that are successful take a strategic approach to these acquisitions, striking a balance between short-term financial restrictions and long-term performance standards and institutional objectives. Compared to regular medical supply purchases, the intricacy of vascular models necessitates a more advanced evaluation procedure.
Identifying Reputable Suppliers and Manufacturers
Although there are many providers in the medical simulation sector, very few have the specific knowledge needed to create high-fidelity neurovascular models. Manufacturers with specialized R&D skills in 3D printing and anatomical modeling should be given preference while looking for possible providers. Businesses with decades of experience in this field are aware of the minute distinctions between good imitations and training aids that are genuinely outstanding.
Credentials for certification and quality control offer impartial proof of manufacturing standards. Seek out vendors who can record their quality control procedures and hold ISO certifications pertinent to the production of medical devices. When feasible, ask for samples so that your educators and clinical staff can test the models out in person before placing bigger orders. This due diligence guarantees that product capabilities and institutional needs are aligned and helps to avoid costly errors.
Geographic considerations for a 3D artery model also influence supplier selection. Global sourcing increases alternatives, but it can also create issues with customs clearance, shipping logistics, and cross-time zone communication. Manufacturers who have set up effective global distribution networks can allay these worries by partnering with reputable couriers and providing prompt assistance to customers wherever they may be.
Customization Options and Bulk Order Considerations
While standard catalog models are useful for many purposes, personalization allows 3D printing technology to reach its full potential for specific needs. You can better express your expectations and determine whether a supplier can meet them if you know what customized implies. Customization requests for neurovascular models sometimes entail changing the number, size, position, or form of aneurysms to reflect particular diseases or training settings.
Another common area of customisation is modifications to vessel geometry. Models that correspond to specific patient cases or educational goals can be created by altering the degree of tortuosity in the internal carotid artery, the branching angles of cerebral arteries, or the presence of atherosclerotic plaques. Medical imaging can be easily converted into physical replicas by manufacturers who accept data files in formats like CT DICOM, CAD, STL, or STEP. This allows for the creation of genuinely patient-specific models for surgery planning.
Beyond only unit cost issues, bulk purchase merits serious examination. Volume discounts can drastically lower per-model costs, increasing the financial viability of implementing extensive training programs. Bulk orders, however, necessitate assurances on the quality of the goods and the dependability of the supplier. Clear terms pertaining to manufacturing schedules, quality requirements, acceptance standards, and replacements for faulty units should be negotiated. By defining these guidelines up front, disagreements are avoided and transactions run smoothly.
Logistics, Lead Times, and After-Sales Support
The intricacy of the model and the need for customisation determine the production schedule. While highly personalized replicas may take several weeks from order confirmation to delivery, standard models often ship in a matter of days. Planning training courses, conferences, or surgery dates that rely on model availability requires an understanding of these schedules. Reputable vendors keep in touch during the production process and give accurate lead time estimates.
Medical simulation equipment shipping logistics necessitate specific treatment to avoid damage during transportation. Although silicone versions are robust when in use, they may be susceptible to compression or extremely high or low temperatures when being transported. Make that your supplier employs reputable courier services like FedEx, DHL, UPS, or TNT that provide monitoring and insurance for foreign shipments, as well as acceptable packaging techniques. Make it clear who is responsible for import taxes, customs charges, and any shipping damage.
Beyond the scope of a simple warranty, after-sales service takes several forms. By offering advice on upkeep, care, and the best practices for usage, technical support enables users to optimize the instructional or therapeutic value of their models. In order to assist institutions in incorporating the models into their current workflows or curriculum, several providers provide training sessions or documentation. This continuous assistance turns a transactional purchase into a cooperative relationship that adapts to your changing demands.
Conclusion
The way that healthcare organizations approach clinical training, surgical preparation, and medical device development has been completely changed by realistic vascular simulators such as the 3D artery model. The transition from conventional teaching aids to advanced silicone-based models is a reflection of both a greater understanding of effective medical education and broader advancements in manufacturing technology. These anatomically accurate models offer practical learning opportunities that enhance theoretical education, foster procedural confidence, and ultimately raise the standard of patient care. Your investment will have a long-lasting educational and clinical impact if you choose the right models and collaborate with knowledgeable producers. The use of high-fidelity simulation in healthcare training will only increase as patient safety standards rise and medical procedures become more sophisticated.
FAQs
What standards determine a neurovascular model's correctness and realism?
The degree of clinical-grade realism attained by a vascular simulator is determined by a number of objective metrics. Comparing the model's measurements to published anatomical references or patient imaging data is known as dimensional accuracy, and it usually calls for tolerances of less than one millimeter for important features. The Shore hardness number, which controls how vessels react to catheter manipulation, is one of the material qualities that must mimic the behavior of human tissue. Smoother internal lumens provide more realistic navigation, and surface finish influences how devices move through the model. Anatomical completeness guarantees that all pertinent structures—such as branch vessels, bifurcations, and pathological features like aneurysms or stenoses—appear in the appropriate spatial connections.
In what ways do these approaches enhance the efficacy of medical education and training?
When compared to traditional didactic instruction or observation-based learning, educational research consistently shows that practical experience with realistic simulators speeds up the acquisition of skills. Through repetition, learners cultivate procedural intuition and muscle memory in secure settings where errors are viewed as teaching opportunities rather than threats to patient safety. Physical models' three-dimensionality fosters spatial reasoning skills that two-dimensional imaging cannot match. Students are able to work with the models, see anatomy from many angles, and create the mental maps required for intricate intervention techniques. When transferring to real patient care, trainees who practice using high-fidelity simulators exhibit increased confidence, quicker treatment times, and fewer problems, according to assessment studies.
Which customization choices are available to meet certain educational or clinical needs?
Vascular models can be extensively modified to meet specific needs thanks to modern 3D printing technologies. It is possible to modify the size, position, shape, and neck properties of pathological structures like aneurysms. Changing tortuosity, modifying branch angles, adding stenotic lesions, or reproducing congenital abnormalities are examples of alterations to vessel geometry. By directly converting medical imaging data into physical replicas, patient-specific customization enables surgical teams to train on models that accurately reflect the anatomy of each patient. Creating increasingly challenging courses, mixing several illnesses, or highlighting specific anatomical areas pertinent to particular training goals are some examples of educational personalization.
For large purchases, what are the usual lead times and shipping choices?
Institutions can confidently arrange training schedules because standard models usually ship seven to ten days after order confirmation. Depending on the complexity of the alteration, customized models take longer to produce—usually two to four weeks. Although very large volumes could necessitate phased delivery schedules, bulk orders receive the same priority production treatment. For most international locations, international shipping by major couriers like FedEx, DHL, UPS, and TNT offers dependable travel times of three to seven days. When scheduling allows, expedited delivery options might be used to meet urgent needs. Customers are kept up to date on the progress of their orders thanks to open communication throughout the production and shipping process.
Partner with Trandomed for Advanced Neurovascular Simulation Solutions
Given your institution's dedication to clinical excellence and innovative teaching, you should choose a 3D artery model supplier who shares these values and has the technical know-how to help you achieve your objectives. With more than two decades of specialized experience in medical 3D printing, Trandomed combines a thorough understanding of clinical applications with manufacturing know-how. Our middle cerebral artery model is the result of decades of material refinement, anatomical correctness, and feedback from medical specialists across the globe. We offer the adaptable, high-fidelity models your applications require, whether you're setting up a hospital simulation center, preparing intricate neurosurgery cases, evaluating novel interventional devices, or outfitting an anatomy lab at a medical school. To discuss your unique needs, obtain comprehensive product specs, or set up a sample evaluation, get in touch with jackson.chen@trandomed.com right now. Procurement managers, clinical educators, research directors, and medical device development teams looking for dependable manufacturing partners that provide outstanding quality and prompt service at every step of the procurement process are welcome to contact us.
References
Anderson, J.R., Thompson, W.L., Alkattan, A.K., Diaz, O., Klucznik, R., Zhang, Y.J., Britz, G.W., Grossman, R.G., and Karmonik, C. (2017). "Three-dimensional printing of anatomically accurate, patient specific intracranial aneurysm models." Journal of NeuroInterventional Surgery, 8(5), 517-520.
Mashiko, T., Otani, K., Kawano, R., Konno, T., Kaneko, N., Ito, Y., and Watanabe, E. (2015). "Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping." World Neurosurgery, 83(3), 351-361.
Kimura, T., Morita, A., Nishimura, K., Aiyama, H., Itoh, H., Fukaya, S., Sora, S., and Ochiai, C. (2009). "Simulation of and training for cerebral aneurysm clipping with three-dimensional models." Neurosurgery, 65(4), 719-726.
_1734504221178.webp)
 (SJ001D)_1734504338727.webp)
_1734507815464.webp)
_1732843184544.webp)