Simulating Aneurysm Clipping: The Role of Aneurysm Models in Surgical Planning
2025-07-09 09:00:53
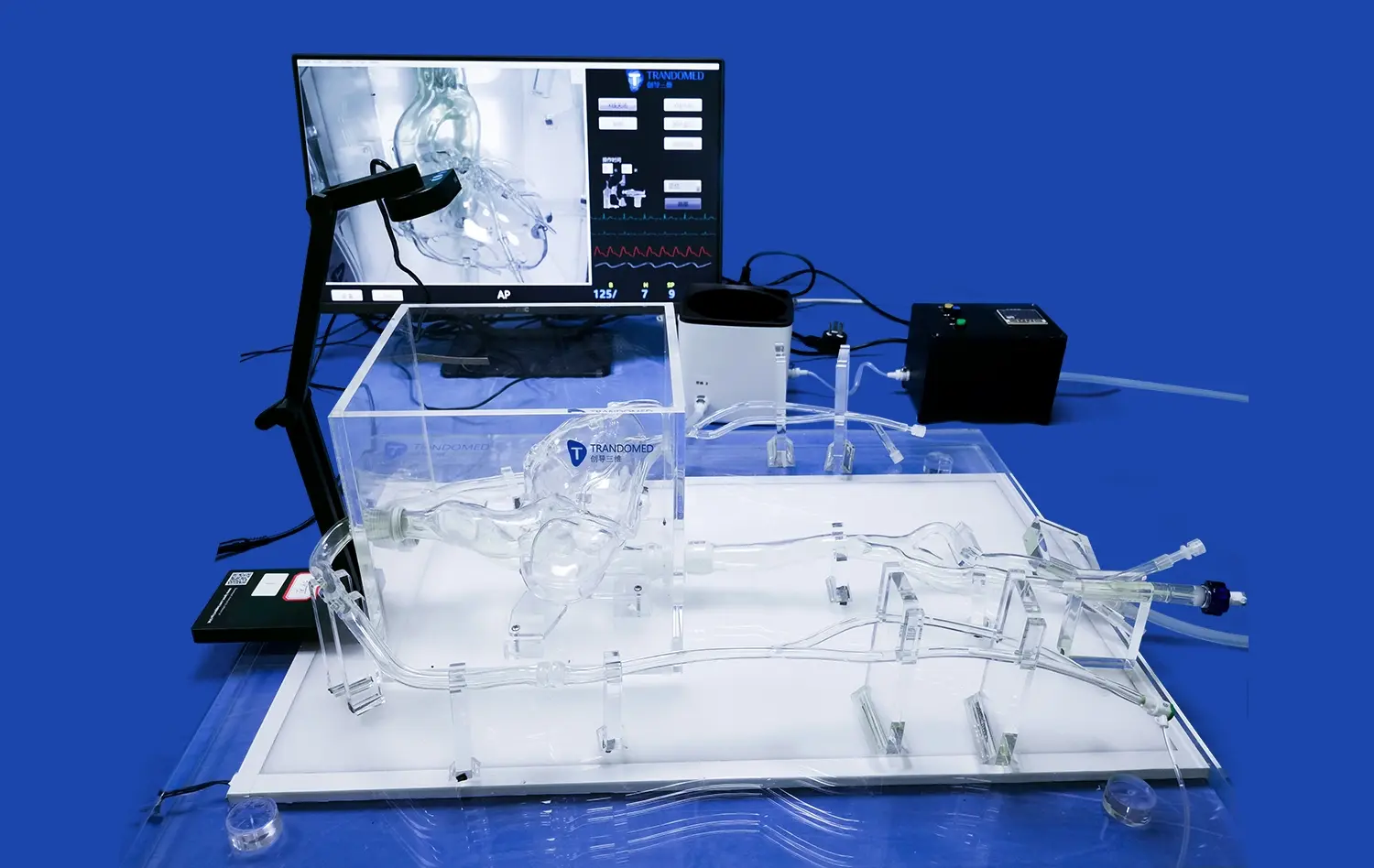
Aneurysm clipping is a complex neurosurgical procedure that requires meticulous planning and precision. The role of aneurysm models in surgical planning has become increasingly significant, offering neurosurgeons valuable insights into the unique anatomical challenges of each case. These 3D-printed replicas provide a tangible representation of the patient's vascular anatomy, allowing surgeons to visualize, strategize, and practice complex clipping techniques before entering the operating room. By integrating aneurysm simulation into preoperative planning, surgeons can enhance their decision-making processes, optimize clip placement, and ultimately improve patient outcomes. This article explores the multifaceted benefits of using aneurysm models in surgical simulation, from understanding anatomical intricacies to preventing potential complications during the actual procedure.
Anatomy of Aneurysm Clipping: Understanding the Challenges of Surgical Simulation
Complexities of Cerebral Vasculature
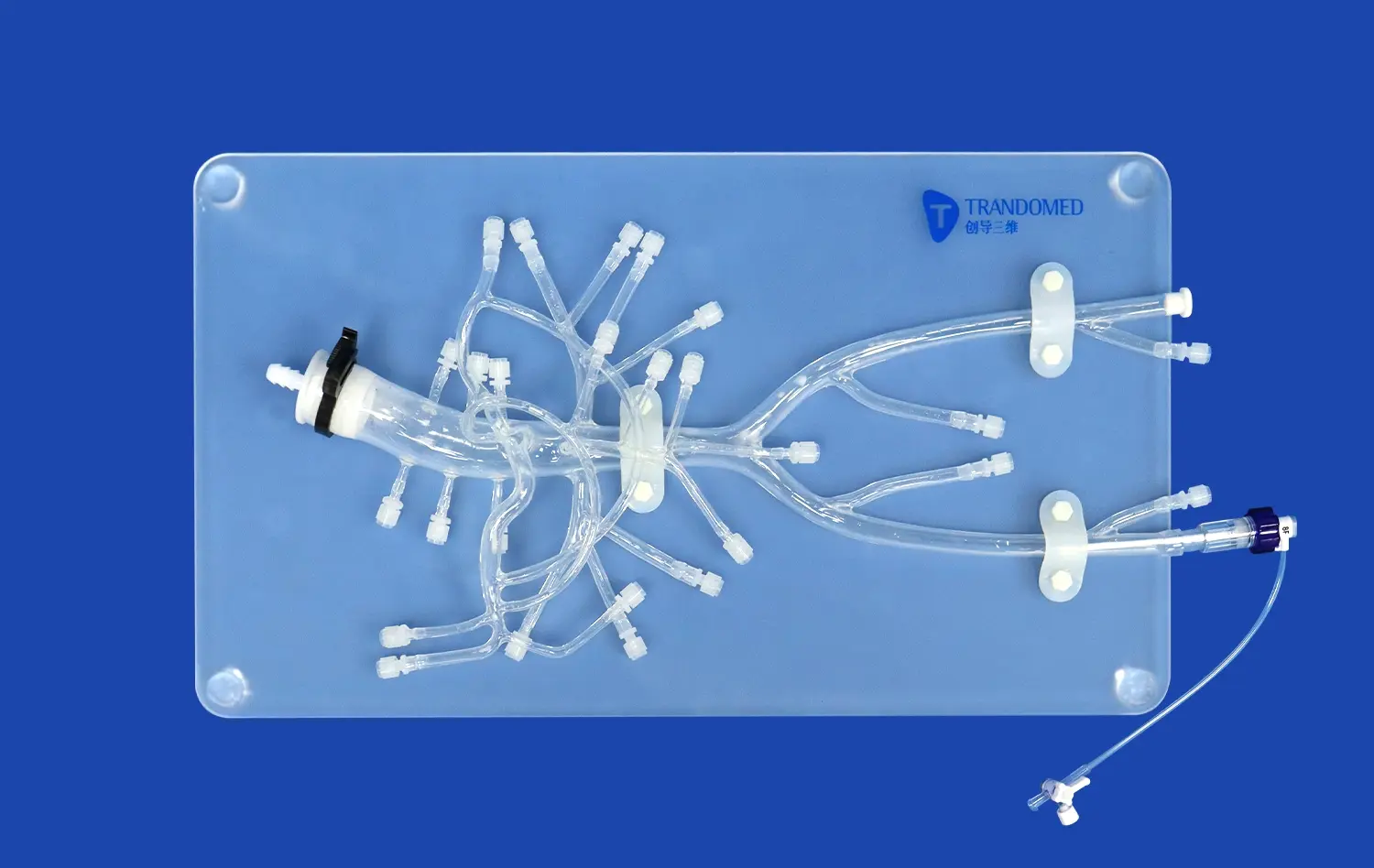
The human brain's vascular system is a labyrinth of intricately connected arteries and veins. Aneurysms, which are abnormal bulges in blood vessel walls, can form in various locations and configurations. Each aneurysm presents a unique set of challenges, influenced by factors such as size, shape, location, and surrounding anatomical structures. Neurosurgeons must navigate this complex landscape with utmost precision to successfully clip the aneurysm without compromising blood flow to critical brain regions.
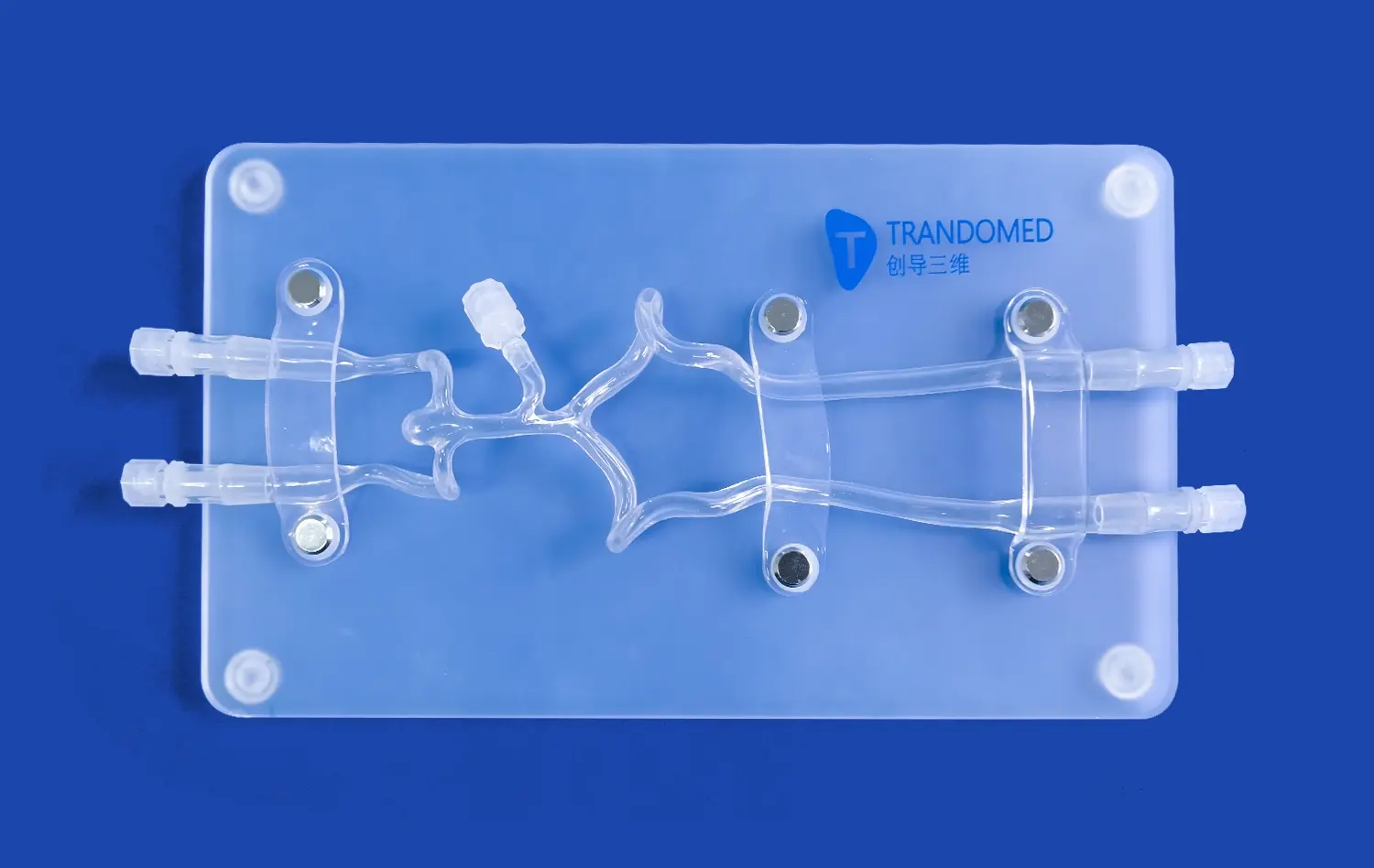
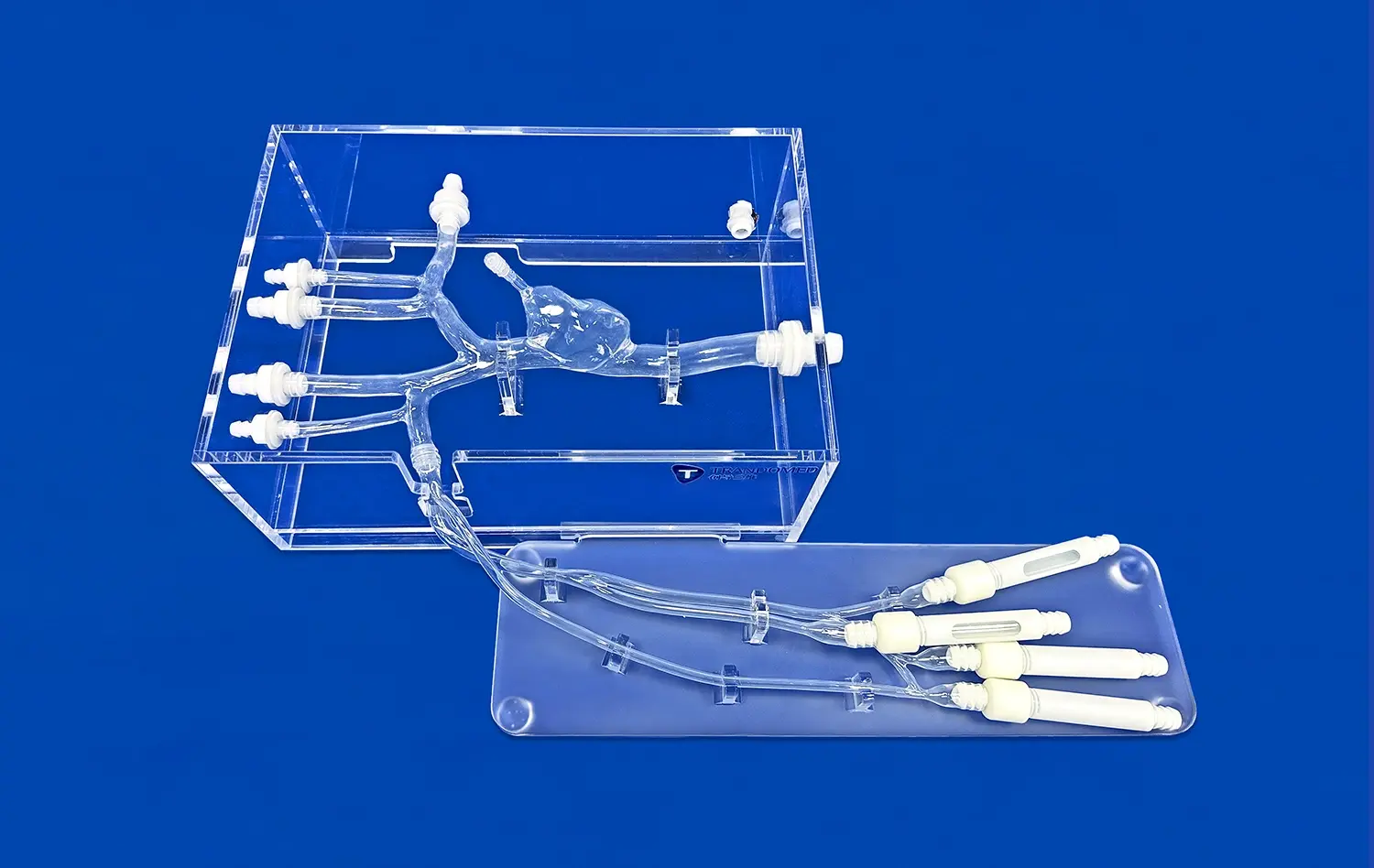
Aneurysm models play a crucial role in helping surgeons comprehend these complexities. By providing a three-dimensional representation of the patient's specific vascular anatomy, these models allow for a more intuitive understanding of spatial relationships and potential obstacles. Surgeons can examine the aneurysm from multiple angles, assess its relationship to nearby blood vessels, and identify critical perforating arteries that must be preserved during the clipping procedure.
Variability in Aneurysm Morphology
Aneurysms come in various shapes and sizes, each presenting its own set of challenges for surgical intervention. Saccular aneurysms, the most common type, resemble a berry-like outpouching from the artery wall. Fusiform aneurysms, on the other hand, involve a widening of the entire circumference of the blood vessel. Additionally, some aneurysms may have complex configurations, such as bilobed or multilobed structures, which further complicate the clipping process.
Aneurysm simulation using 3D-printed models allows surgeons to appreciate these morphological nuances in a tangible format. By handling and manipulating the model, surgeons can gain insights into the optimal approach for clip placement, taking into account the aneurysm's neck width, dome orientation, and any irregularities in its shape. This hands-on experience with a patient-specific model can significantly enhance the surgeon's mental preparation and strategy formulation before the actual procedure.
Using Aneurysm Models to Assess Aneurysm Morphology and Optimize Clipping Strategies
Preoperative Planning and Clip Selection
One of the most valuable aspects of using aneurysm models in surgical planning is the ability to conduct detailed preoperative assessments. Surgeons can use these models to meticulously evaluate the aneurysm's morphology, including its size, shape, and orientation relative to the parent vessel. This in-depth analysis allows for more informed decision-making regarding the optimal surgical approach and clip selection.
By manipulating the aneurysm model, surgeons can experiment with different clip configurations and placements. They can assess how various clip sizes and shapes interact with the aneurysm neck and surrounding vasculature. This process helps in determining the most suitable clip or combination of clips to achieve complete aneurysm occlusion while preserving blood flow in adjacent vessels. The ability to "test" different clipping strategies on a patient-specific model can lead to more confident and efficient intraoperative decision-making.
Simulating Complex Clipping Techniques
Certain aneurysms, due to their location or configuration, may require advanced clipping techniques. These can include tandem clipping, where multiple clips are used in a linear fashion, or fenestrated clips that allow for the preservation of perforating arteries. Aneurysm models provide an invaluable platform for surgeons to practice and refine these complex techniques before attempting them in the operating room.
Using the model, surgeons can simulate various clipping scenarios, assessing the feasibility and potential risks of each approach. They can practice clip application, repositioning, and removal, gaining a tactile sense of how the clips interact with the aneurysm and surrounding structures. This hands-on simulation not only enhances the surgeon's technical skills but also promotes creative problem-solving for challenging cases. By the time the actual surgery takes place, the surgeon has already mentally and physically rehearsed the procedure, potentially leading to smoother execution and reduced operative time.
The Role of Simulation in Preventing Complications During Aneurysm Clipping
Identifying and Mitigating Risks
Aneurysm clipping carries inherent risks, including the potential for clip slippage, incomplete aneurysm occlusion, or inadvertent occlusion of nearby vessels. Aneurysm models serve as powerful tools for identifying and mitigating these risks before they manifest in the operating room. By closely examining the model, surgeons can pinpoint areas of concern, such as a wide aneurysm neck or the presence of calcifications, which may complicate clip placement.
Simulation with aneurysm models allows surgeons to anticipate potential complications and develop strategies to address them. For instance, if the model reveals a high likelihood of clip slippage due to aneurysm geometry, the surgeon might plan to use multiple clips or consider alternative techniques like wrapping or bypass. This proactive approach to risk management can significantly reduce the chances of intraoperative surprises and improve overall surgical outcomes.
Enhancing Surgical Team Communication
Effective communication within the surgical team is crucial for successful aneurysm clipping. Aneurysm models serve as excellent visual aids for facilitating discussions among team members, including surgeons, anesthesiologists, and operating room nurses. By referencing the model during preoperative briefings, the lead surgeon can clearly convey the planned approach, potential challenges, and contingency plans to the entire team.
This shared understanding of the case's complexities ensures that all team members are aligned and prepared for various scenarios that may arise during surgery. The aneurysm model becomes a focal point for collaborative problem-solving, allowing team members to contribute insights and suggestions based on their respective expertise. This enhanced communication and preparation can lead to smoother intraoperative coordination, reduced confusion, and ultimately, improved patient safety.
Conclusion
The integration of aneurysm models in surgical planning represents a significant advancement in the field of neurosurgery. These patient-specific simulations offer surgeons unprecedented opportunities to visualize, strategize, and practice complex clipping procedures before entering the operating room. By providing a tangible representation of the patient's unique vascular anatomy, aneurysm models enhance preoperative decision-making, facilitate the optimization of clipping strategies, and play a crucial role in preventing potential complications. As technology continues to evolve, the role of aneurysm simulation in surgical planning is likely to become even more integral, further improving the safety and efficacy of aneurysm clipping procedures.
Contact Us
To learn more about our advanced 3D-printed aneurysm models and how they can enhance your surgical planning process, please contact us at jackson.chen@trandomed.com. Our team is dedicated to providing cutting-edge solutions that support neurosurgeons in delivering the best possible care to their patients.
References
Lawton, M. T., & Spetzler, R. F. (2010). Surgical management of giant intracranial aneurysms: Experience with 171 patients. Clinical Neurosurgery, 57, 110-115.
Wiebers, D. O., et al. (2003). Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. The Lancet, 362(9378), 103-110.
Sekhar, L. N., & Fessler, R. G. (Eds.). (2006). Atlas of neurosurgical techniques: Brain. Thieme Medical Publishers.
Rhoton, A. L. (2002). Aneurysms. Neurosurgery, 51(suppl_4), S1-121.
Molyneux, A. J., et al. (2005). International subarachnoid aneurysm trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: A randomised comparison of effects on survival, dependency, seizures, rebleeding, subgroups, and aneurysm occlusion. The Lancet, 366(9488), 809-817.
Chowdhury, T., & Cappellani, R. B. (2017). Aneurysm clipping: Techniques and strategies. Journal of Neurosurgical Anesthesiology, 29(3), 275-281.
_1735798438356.webp)