Simulating Aneurysms: How 3D Vascular Models Improve Surgical Outcomes
2025-07-01 09:00:00
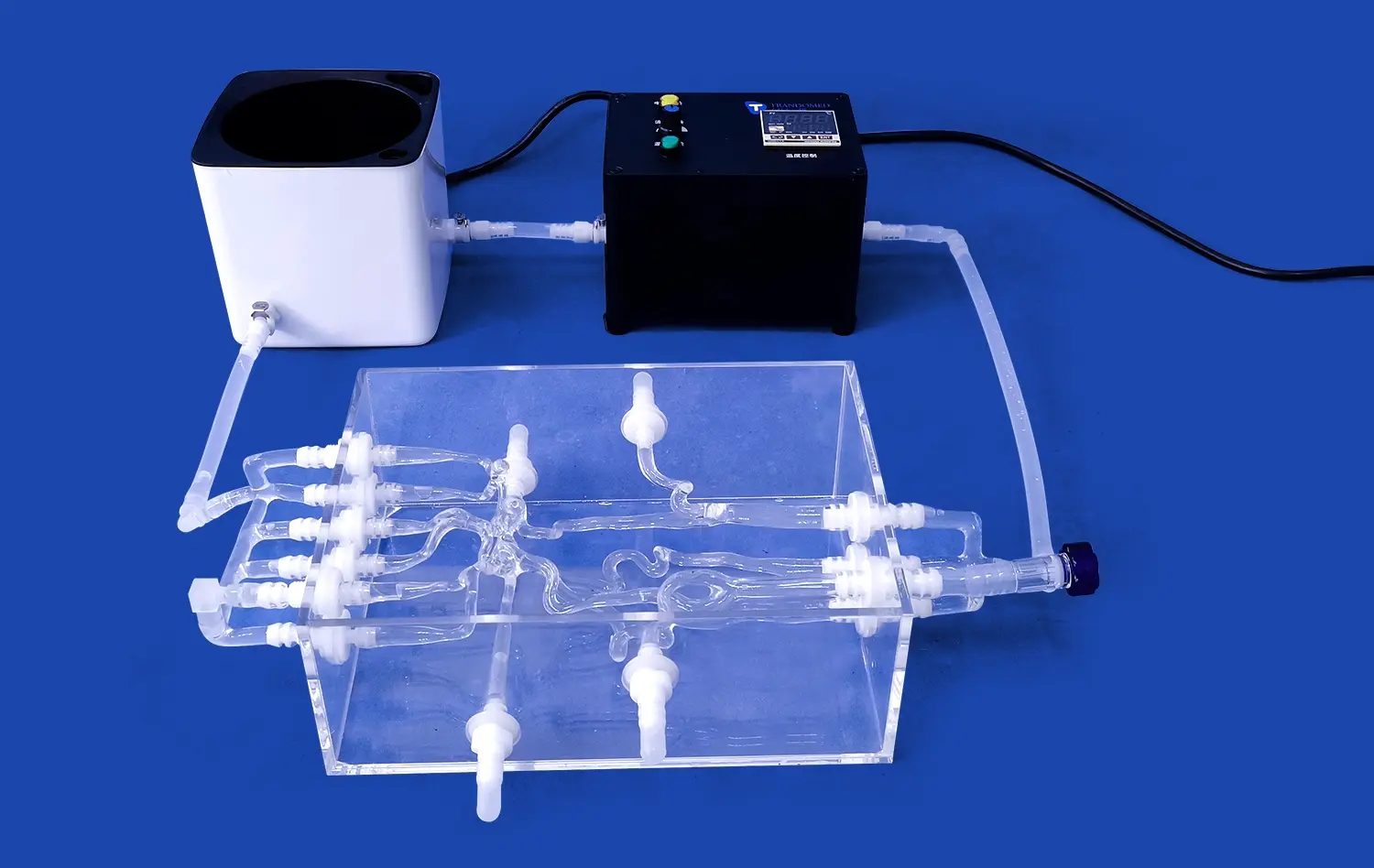
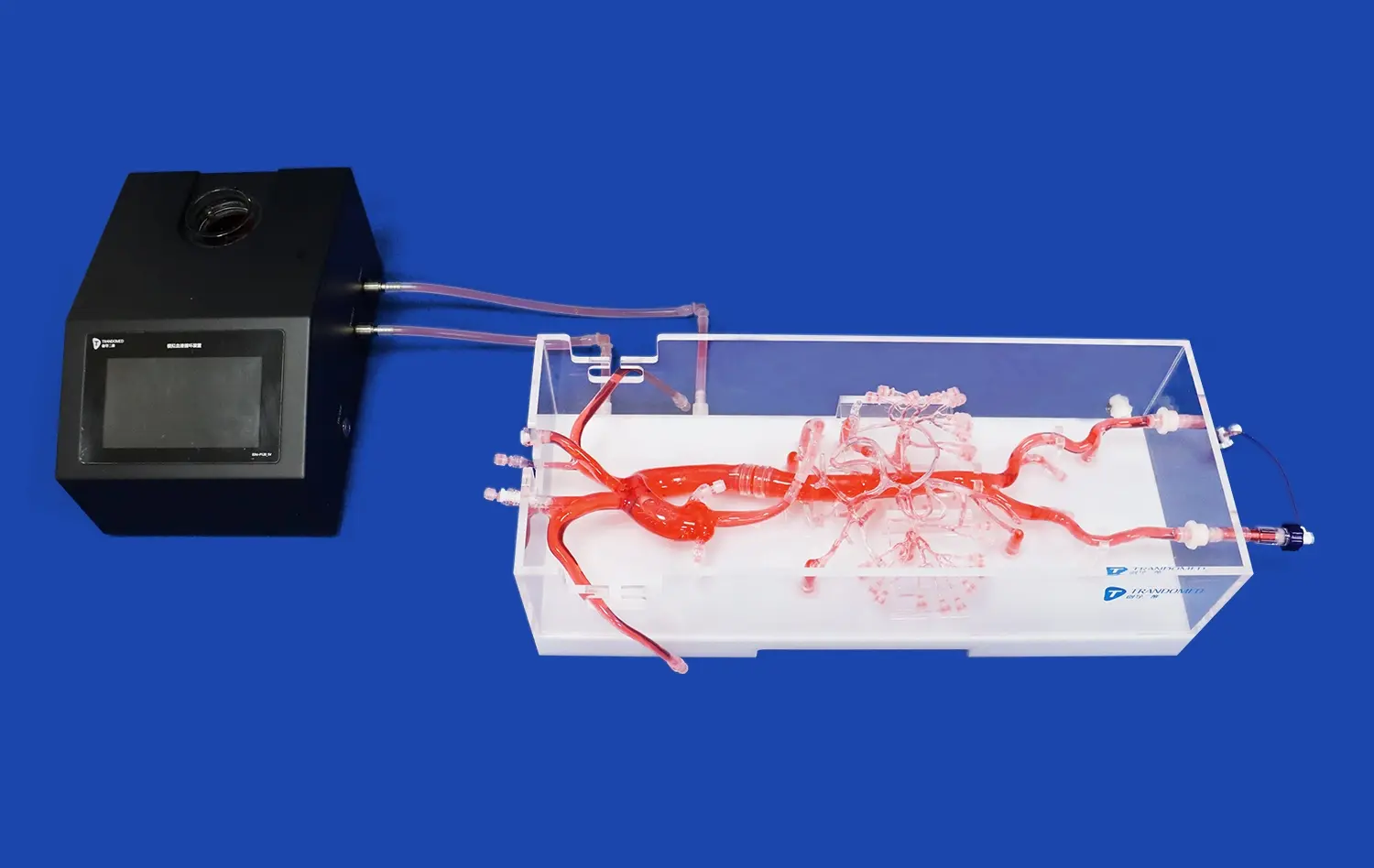
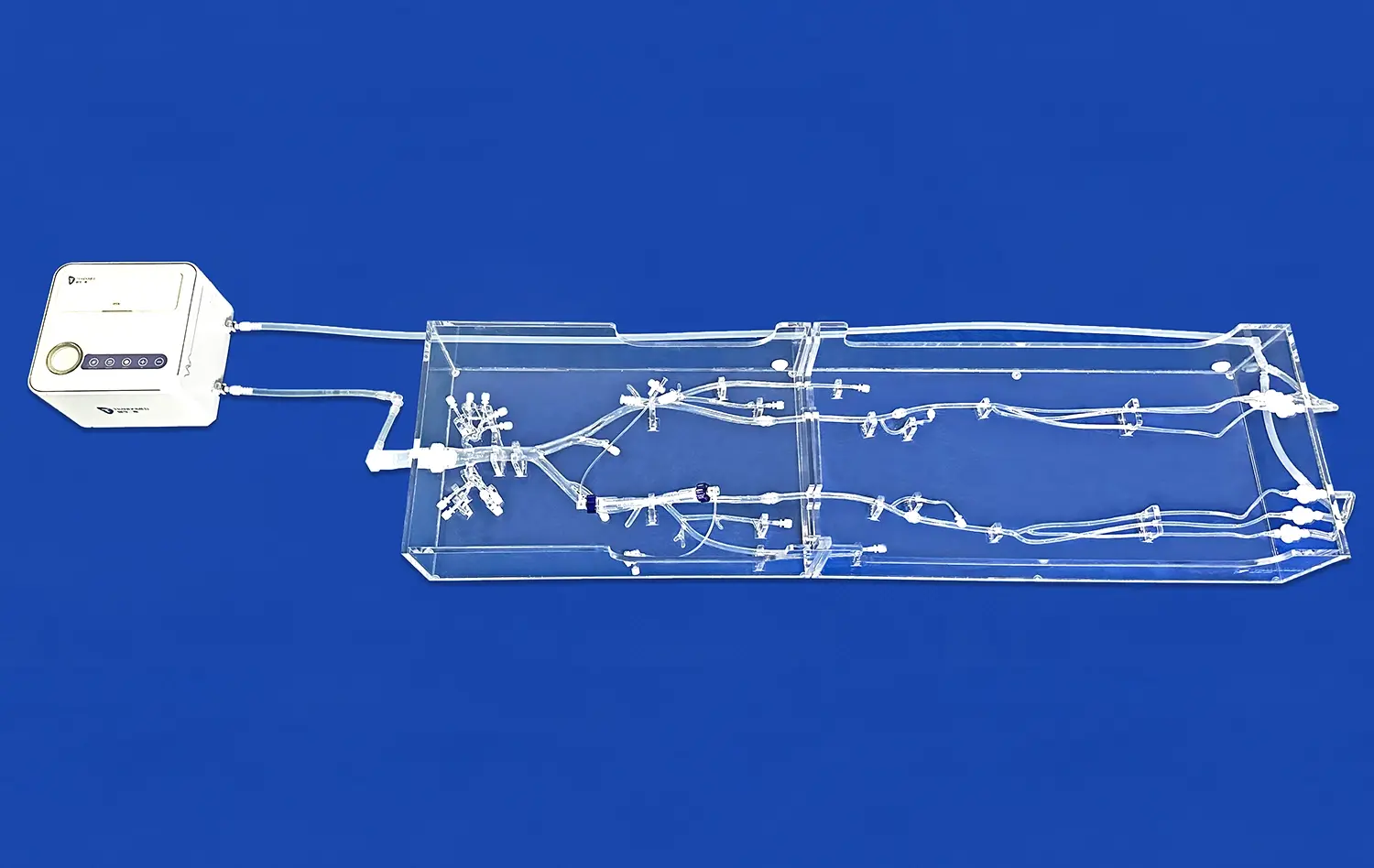
In the realm of neurosurgery and vascular interventions, precision and preparation are paramount. The advent of 3D vascular models has revolutionized the approach to treating complex aneurysms, offering surgeons unprecedented insights and training opportunities. These patient-specific replicas, created through advanced 3D printing technology, allow medical professionals to visualize, plan, and practice intricate procedures before stepping into the operating room. By providing a tangible representation of a patient's unique vascular anatomy, these models enable surgeons to tailor their strategies, reduce potential complications, and ultimately improve patient outcomes. The integration of 3D printed vascular simulators into surgical planning and training protocols marks a significant leap forward in the field of neurovascular surgery, promising enhanced precision, reduced operative times, and increased safety for patients undergoing aneurysm treatment.
Tailoring Surgical Strategies with Patient-Specific 3D Vascular Models
Customized Approach to Complex Aneurysms
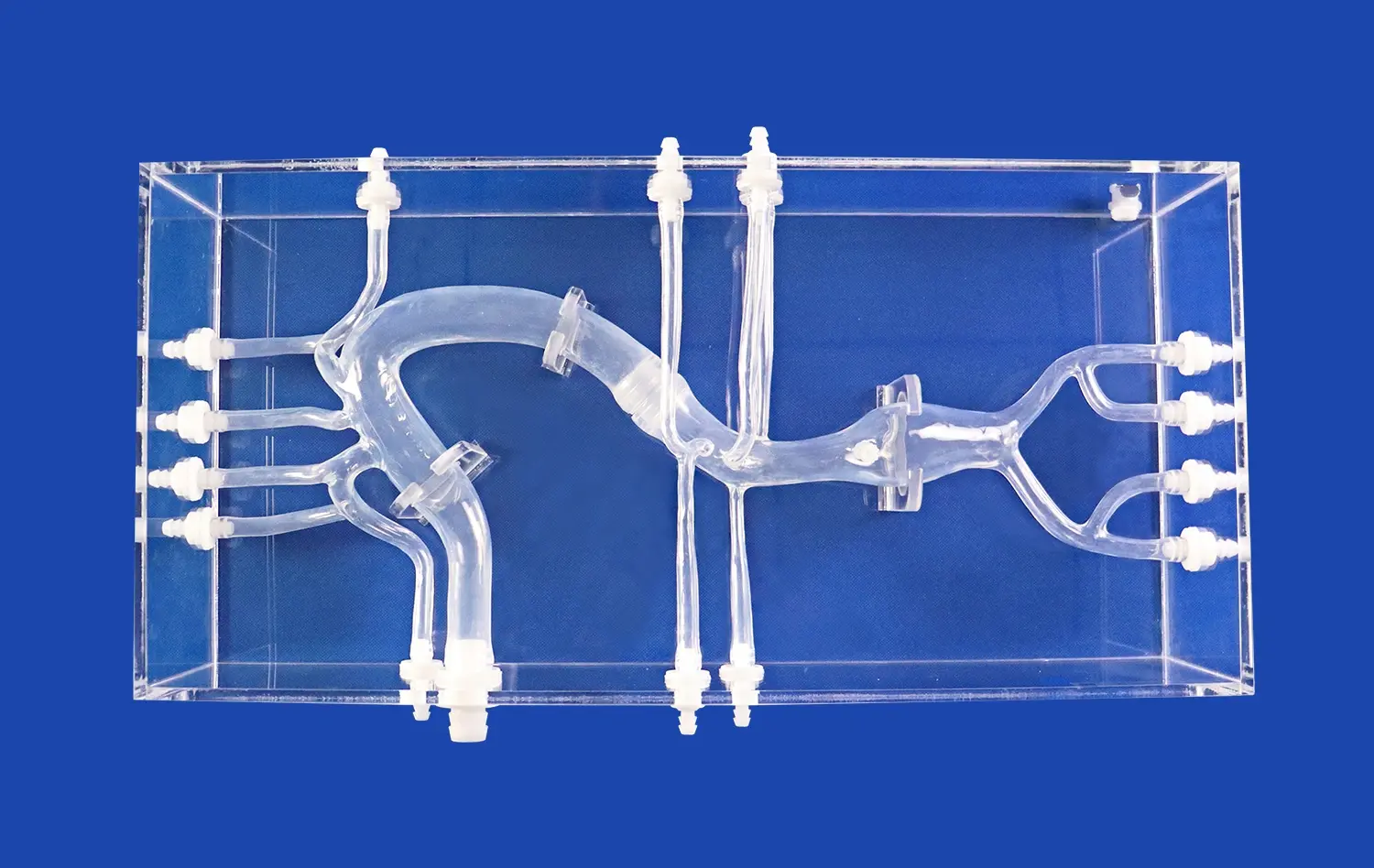
The intricate nature of cerebral aneurysms demands a personalized approach to treatment. 3D vascular models, derived from patient imaging data, offer surgeons a unique opportunity to examine the nuances of each case in detail. These physical representations allow for a comprehensive understanding of the aneurysm's size, shape, and location within the context of surrounding vasculature.
By manipulating these tactile models, neurosurgeons can explore various access routes and intervention techniques. This hands-on experience proves invaluable when dealing with challenging anatomical variations or particularly complex aneurysm configurations. The ability to strategize and refine surgical approaches before the actual procedure significantly enhances the surgeon's confidence and preparedness.
Optimizing Clip Placement and Endovascular Device Selection
One of the critical aspects of aneurysm treatment is the selection and placement of clips or endovascular devices. 3D vascular models excel in this arena, allowing surgeons to test different clip sizes and configurations on an exact replica of the patient's anatomy. This process helps in identifying the optimal clip type and position, ensuring complete aneurysm occlusion while preserving blood flow to vital brain regions.
For endovascular procedures, these models assist in choosing the most suitable stents or coils. Surgeons can simulate the deployment of devices, assessing their fit and effectiveness in the specific aneurysm geometry. This pre-operative planning minimizes the risk of device-related complications and improves the overall success rate of the intervention.
How Simulation Reduces Complication Rates and Improves Patient Safety?
Mitigating Procedural Risks Through Preoperative Planning
The use of 3D vascular models in preoperative planning significantly contributes to risk reduction in aneurysm surgeries. By providing a clear, three-dimensional view of the patient's vascular architecture, these models help surgeons anticipate and prepare for potential challenges. This foresight is crucial in minimizing intraoperative surprises that could lead to complications.
Surgeons can identify critical perforating arteries, assess the relationship between the aneurysm and surrounding structures, and plan their approach to avoid damaging vital tissues. This level of preparation is particularly valuable in cases involving giant or complex aneurysms, where the margin for error is exceedingly small.
Enhancing Surgical Team Communication and Coordination
3D vascular models serve as powerful communication tools within the surgical team. They provide a common reference point for discussing the case, allowing all team members to visualize the planned procedure. This shared understanding enhances coordination during the surgery, leading to smoother operations and reduced operative times.
Moreover, these models facilitate interdisciplinary collaboration. Neurosurgeons can easily consult with radiologists, neurologists, and other specialists, using the 3D model to illustrate specific concerns or strategies. This collaborative approach ensures that all aspects of patient care are considered, further improving safety and outcomes.
Enhanced Hands-On Practice on Realistic Aneurysm Models
Bridging the Gap Between Theory and Practice
The transition from theoretical knowledge to practical application is a critical phase in surgical training. 3D printed vascular models bridge this gap by providing residents and experienced surgeons alike with opportunities for realistic, hands-on practice. These models can be designed to replicate various aneurysm types and complexities, offering a comprehensive training platform.
Trainees can perform simulated procedures repeatedly, honing their skills without risk to patients. This iterative practice leads to improved hand-eye coordination, better spatial awareness, and increased confidence in handling surgical instruments. For experienced surgeons, 3D vascular models offer a chance to refine techniques or prepare for particularly challenging cases.
Simulating Rare and Complex Cases
One of the unique advantages of 3D vascular models is the ability to recreate rare or exceptionally complex aneurysm cases. These scenarios may not be frequently encountered in clinical practice but require specific skills and strategies when they do occur. By creating models based on anonymized patient data, medical institutions can build libraries of complex cases for training purposes.
Surgeons can practice on these rare configurations, developing strategies and skills that would be difficult to acquire through traditional training methods alone. This exposure to a wide range of aneurysm types and locations prepares surgeons to handle even the most challenging cases with greater competence and confidence.
Conclusion
The integration of 3D vascular models in aneurysm treatment represents a significant advancement in neurosurgical practice. By enabling tailored surgical strategies, reducing complication rates, and providing enhanced training opportunities, these models are transforming the landscape of aneurysm management. As technology continues to evolve, the role of 3D printed simulators in improving surgical outcomes and patient safety is likely to expand, heralding a new era of precision and personalization in neurovascular surgery.
Contact Us
For more information on how 3D vascular models can revolutionize your surgical practice and improve patient outcomes, contact us at jackson.chen@trandomed.com. Let's explore how our cutting-edge 3D printing technology can enhance your surgical planning and training programs.
References
Wang, L., et al. (2018). "Three-dimensional printing of cerebral aneurysm models for surgical planning and training." Journal of Neurosurgery, 129(4), 1087-1093.
Ionita, C. N., et al. (2014). "Patient-specific 3D printed models for neurosurgery planning and training." Proceedings of SPIE--the International Society for Optical Engineering, 9036, 90360Z.
Benet, A., et al. (2017). "The use of 3-dimensional printing technology in complex spine surgery." World Neurosurgery, 103, 163-171.
Mashiko, T., et al. (2015). "Development of three-dimensional hollow elastic model for cerebral aneurysm clipping simulation enabling rapid and low cost prototyping." World Neurosurgery, 83(3), 351-361.
Rynio, P., et al. (2019). "The use of 3D printing in planning vascular interventions." Vascular, 27(3), 265-272.
Kang, Y., et al. (2016). "Three-dimensional printing technology for treatment of intracranial aneurysm." Chinese Neurosurgical Journal, 2(1), 1-10.