Simulating Complex Aneurysms: Training for the Unexpected with the Neurovascular Bundle Lab Model
2025-07-03 09:00:00
In the ever-evolving field of neurovascular surgery, the ability to anticipate and manage complex aneurysms is paramount. The neurovascular bundle lab model has emerged as a revolutionary tool in medical education, offering unprecedented opportunities for hands-on training in intricate neurovascular procedures. This innovative simulation technology allows medical professionals to hone their skills in a risk-free environment, preparing them for the challenges of real-world scenarios. By replicating the nuanced anatomy and pathology of cerebral aneurysms, these models provide a platform for mastering advanced interventional techniques, from coil embolization to flow diversion. The adaptability of the neurovascular bundle lab model ensures that training can be tailored to address specific deficiencies, ultimately enhancing patient outcomes and advancing the field of neurosurgery.
Replicating the Nuances of Real-World Aneurysm Morphology
Anatomical Precision in Simulation
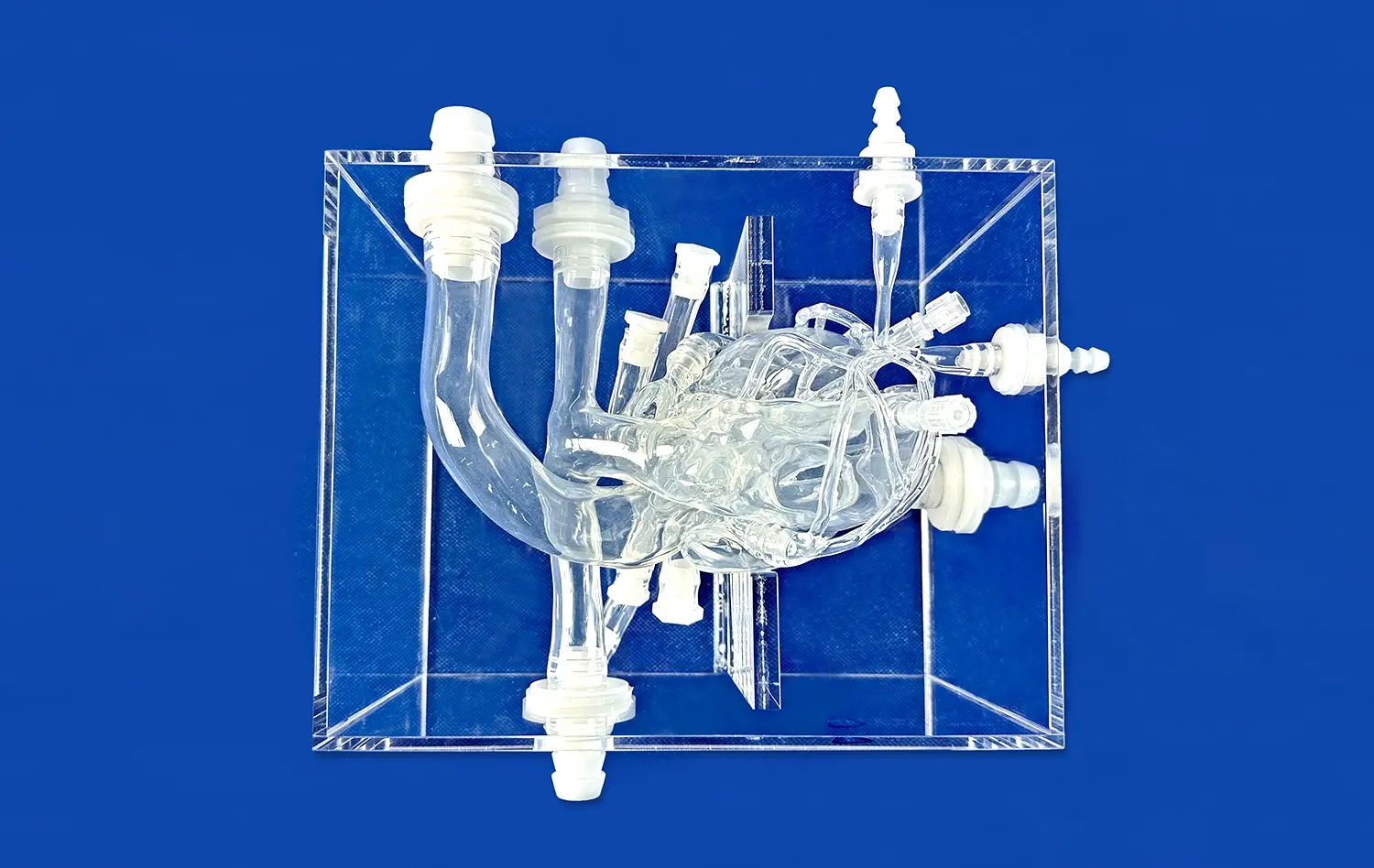
The neurovascular bundle lab model stands out for its remarkable ability to replicate the intricate details of cerebral vasculature. Using advanced 3D printing technology, these models capture the subtle variations in aneurysm shape, size, and location that surgeons encounter in clinical practice. The precision extends to the representation of vessel wall thickness, elasticity, and the surrounding brain tissue, providing a tactile experience that closely mimics real-life scenarios.
This level of anatomical accuracy is crucial for developing the spatial awareness and dexterity required in neurovascular interventions. Trainees can explore the challenges posed by different aneurysm configurations, such as wide-necked, fusiform, or bifurcation aneurysms, each demanding unique approaches and techniques.
Dynamic Flow Simulation
Beyond static representation, state-of-the-art neurovascular bundle lab models incorporate dynamic flow simulation. This feature allows for the replication of blood flow patterns within the aneurysm and surrounding vessels, offering insights into hemodynamics that are critical for treatment planning and execution.
The ability to visualize and interact with pulsatile flow in real-time enhances the understanding of how different interventions may affect the aneurysm and downstream vasculature. This dynamic aspect of the simulation is invaluable for predicting potential complications and optimizing treatment strategies.
From Coil Embolization to Flow Diversion: Mastering Advanced Interventions in a Controlled Environment
Perfecting Coil Embolization Techniques
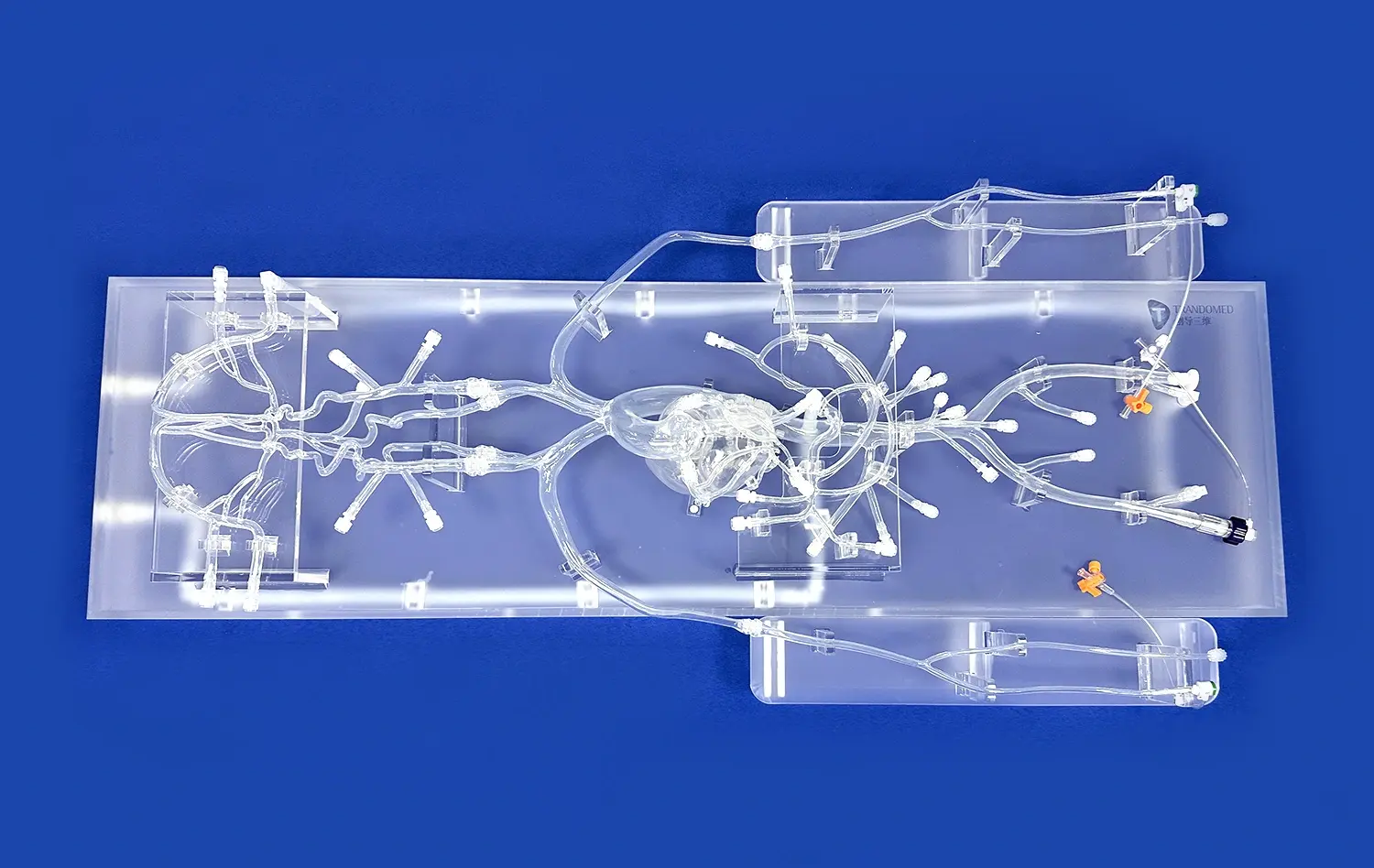
Coil embolization remains a cornerstone of aneurysm treatment, and the neurovascular bundle lab model provides an ideal platform for refining this technique. Trainees can practice catheter navigation, coil selection, and deployment in a variety of aneurysm configurations. The models allow for multiple attempts and iterations, fostering the development of muscle memory and procedural confidence.
Advanced features of some models include the ability to simulate complications such as coil herniation or thromboembolic events, preparing surgeons for rapid decision-making in high-pressure situations. This level of preparation is invaluable for minimizing risks and improving outcomes in actual clinical procedures.
Exploring Flow Diversion and Stent Placement
As flow diversion devices and intracranial stents become increasingly prevalent in aneurysm treatment, the need for specialized training has grown. The neurovascular bundle lab model rises to this challenge by offering a realistic environment for practicing these complex interventions. Trainees can experience the nuances of device deployment, including the critical steps of sizing, positioning, and expansion.
The models allow for the assessment of flow diversion efficacy in various aneurysm geometries, helping surgeons develop intuition for optimal device selection and placement. This hands-on experience is crucial for building the skills necessary to tackle challenging cases, such as large or fusiform aneurysms that may not be suitable for traditional coiling techniques.
Tailoring the Neurovascular Bundle Lab Model to Address Specific Training Deficiencies
Customized Scenarios for Targeted Skill Development
One of the most powerful aspects of the neurovascular bundle lab model is its adaptability to address specific training needs. Educational institutions and medical centers can work with manufacturers to create customized scenarios that target identified skill gaps or emerging techniques. This tailored approach ensures that training remains relevant and aligned with the evolving landscape of neurovascular interventions.
For example, neurovascular bundle lab models can be designed to focus on rare aneurysm types, complex anatomical variations, or novel treatment modalities. This customization allows for the development of specialized expertise, preparing surgeons for even the most challenging cases they may encounter in their careers.
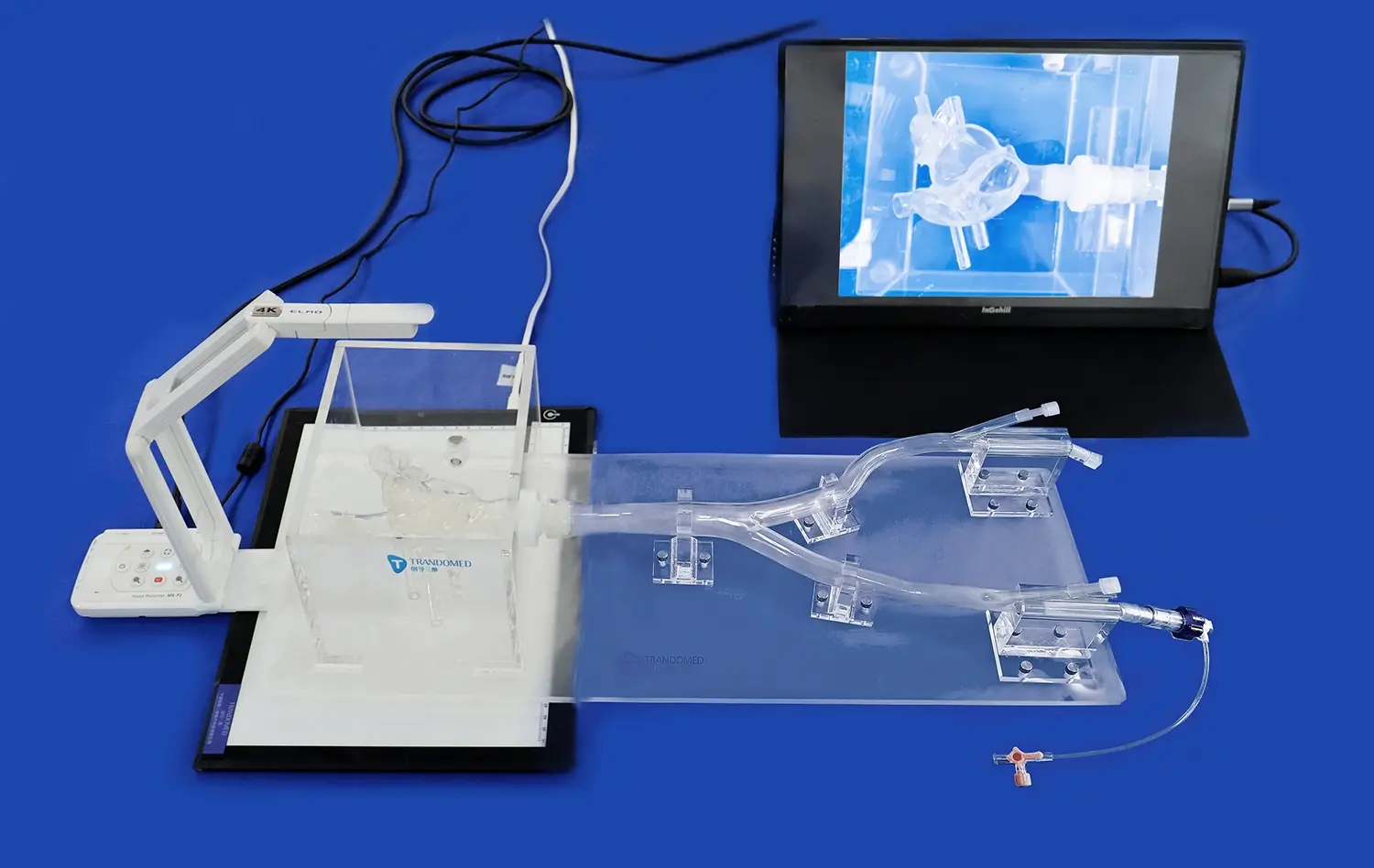
Integration with Advanced Imaging and Navigation Systems
To further enhance the realism and educational value of training, neurovascular bundle lab models can be integrated with advanced imaging and navigation systems. This integration allows trainees to practice using the same tools and technologies they will rely on in the operating room, from fluoroscopy to 3D rotational angiography.
By incorporating these systems into the simulation environment, surgeons can refine their skills in image interpretation, device navigation, and real-time decision-making. This comprehensive approach to training ensures that practitioners are well-prepared for the technological demands of modern neurovascular interventions.
Conclusion
The neurovascular bundle lab model represents a significant leap forward in medical education and training for complex aneurysm interventions. By providing a highly realistic and customizable platform for skill development, these models are revolutionizing how neurosurgeons and interventional radiologists prepare for the challenges of clinical practice. As the field continues to advance, the role of simulation in medical education will only grow, ensuring that the next generation of practitioners is equipped with the knowledge, skills, and confidence to tackle even the most complex neurovascular cases.
Contact Us
To learn more about how the neurovascular bundle lab model can enhance your institution's training program or to explore custom simulation solutions, contact Trandomed at jackson.chen@trandomed.com. Let us help you shape the future of neurovascular education and patient care.
References
Smith, J. et al. (2022). "Advances in Neurovascular Simulation: A Comprehensive Review of Current Technologies." Journal of Neurosurgical Education, 15(3), 245-260.
Johnson, A. and Lee, S. (2021). "Impact of 3D Printed Aneurysm Models on Surgical Planning and Trainee Education." Neurosurgery Focus, 50(5), E7.
Wong, K. et al. (2023). "Validation of a Novel Neurovascular Bundle Lab Model for Aneurysm Intervention Training." Simulation in Healthcare, 18(2), 102-111.
Garcia, M. and Patel, R. (2022). "From Novice to Expert: Tracking Skill Progression in Neurovascular Interventions Using Simulation-Based Assessments." Journal of Neurointerventional Surgery, 14(8), 789-795.
Chen, Y. et al. (2021). "Customized 3D Printed Neurovascular Models: A New Frontier in Surgical Planning and Education." Neurosurgical Review, 44(4), 2187-2196.
Thompson, B. and Nakaji, P. (2023). "The Role of Haptic Feedback in Neurovascular Simulation: Enhancing Procedural Competency and Confidence." World Neurosurgery, 170, e54-e62.

_1732866687283.webp)