How Does Lesion Simulation Enhance PCI Decision-Making?
Replicating Complex Anatomical Variations
Lesion simulation technologies have evolved to replicate intricate anatomical variations with remarkable accuracy. By incorporating patient-specific data from CT scans and MRI imaging, these simulators create highly realistic models of coronary arteries. This level of detail allows trainees to encounter a wide spectrum of lesion types, from simple stenosis to complex bifurcation lesions and chronic total occlusions (CTOs). The ability to practice on such diverse scenarios enhances a practitioner's capacity to make informed decisions when faced with challenging cases in clinical settings.
Dynamic Flow Visualization
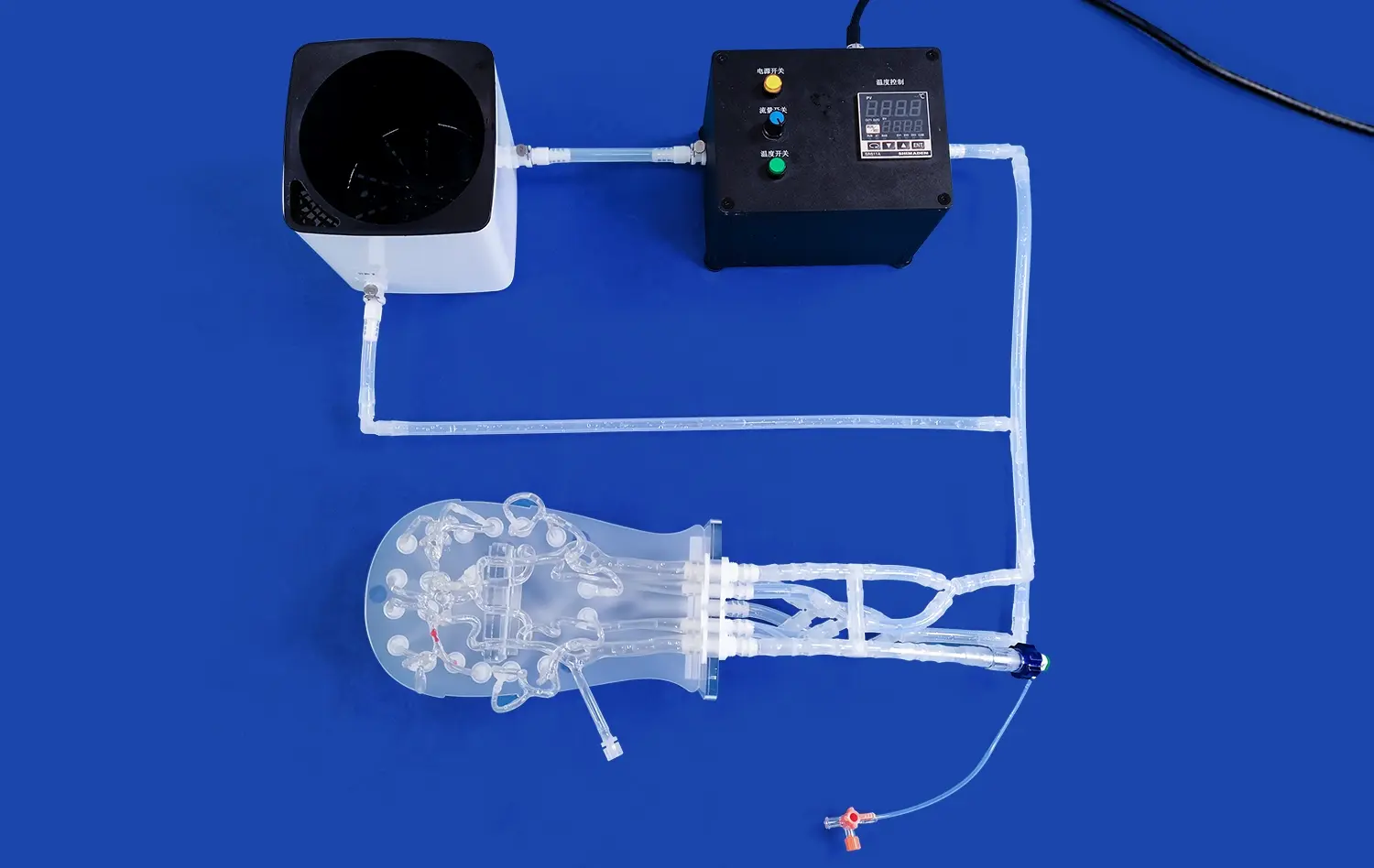
Neuro vascular simulator now integrate dynamic flow visualization capabilities, enabling trainees to observe how blood flow is affected by various lesion characteristics. This feature is particularly valuable in understanding the hemodynamic impact of different stenosis severities and locations. By visualizing flow patterns in real-time, interventionists can better assess the functional significance of lesions and make more informed decisions about when and how to intervene.
Interactive Pressure Wire Simulation
Modern lesion simulation platforms often include interactive pressure wire functionality, allowing trainees to perform virtual Fractional Flow Reserve (FFR) measurements. This capability is crucial in developing the skills necessary to accurately assess the physiological significance of coronary stenoses. By practicing FFR-guided decision-making in a simulated environment, interventionists can refine their ability to distinguish between lesions that require intervention and those that can be managed medically, thereby optimizing patient care and resource utilization.
Realistic Plaque Morphology and Stent Deployment Practice
Diverse Plaque Compositions
Cutting-edge simulators now offer the ability to replicate various plaque compositions, including soft, fibrotic, and calcified lesions. This diversity is essential for trainees to develop a tactile sense of how different plaque types respond to intervention. For instance, practicing on simulated calcified lesions helps interventionists understand the challenges associated with stent delivery and expansion in these complex scenarios, preparing them for similar situations in real patients.
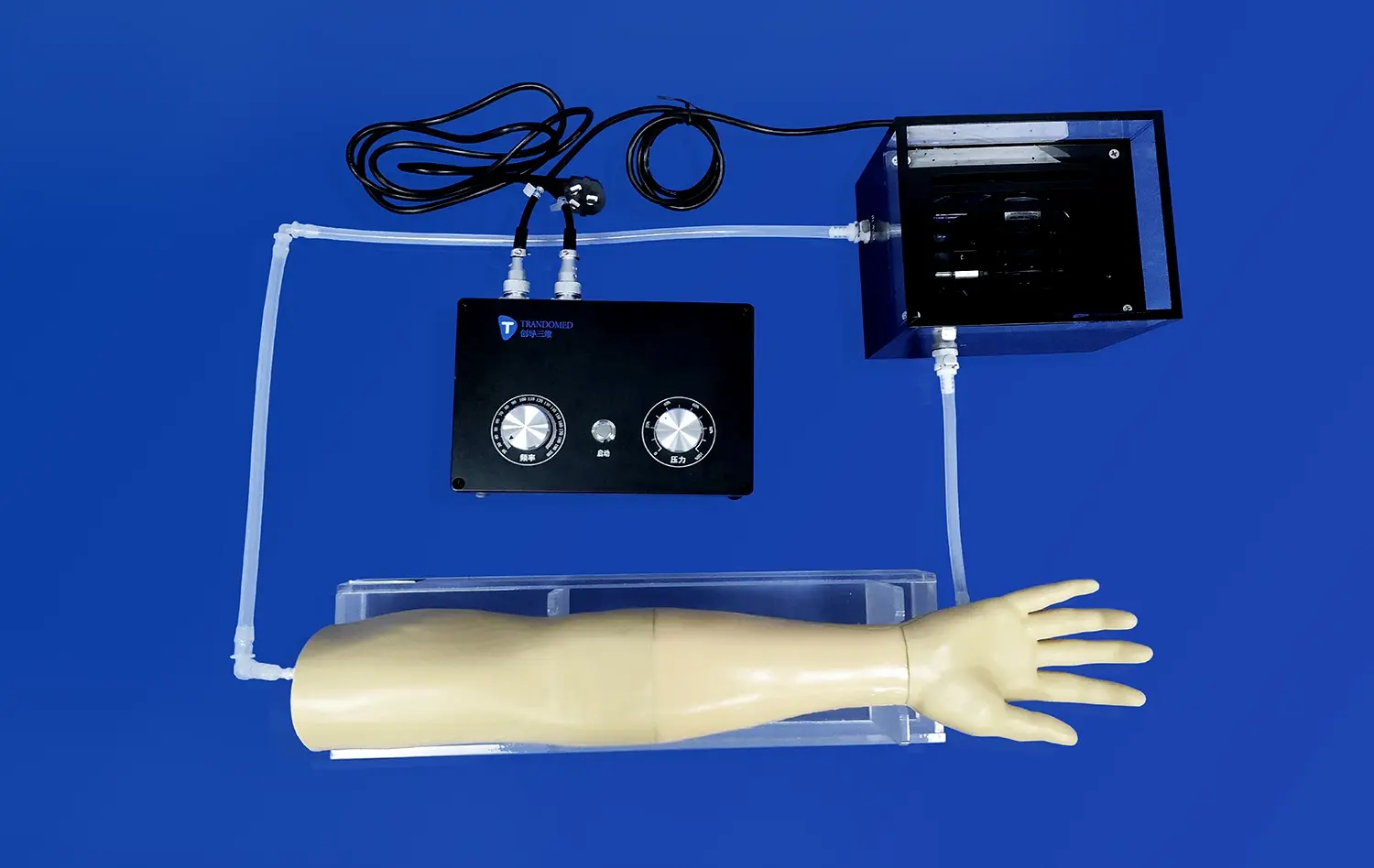
Precision Stent Placement
Lesion simulation using a neuro vascular simulator provides an ideal platform for practicing precise stent placement techniques. Trainees can experiment with different stent sizes, lengths, and deployment strategies without the pressure of a live procedure. This hands-on experience is invaluable in developing the skills necessary to achieve optimal stent apposition and expansion, which are critical factors in preventing complications such as stent thrombosis and restenosis.
Post-Deployment Assessment
Advanced simulators often incorporate features that allow for post-deployment assessment of stent positioning and expansion. This capability enables trainees to evaluate the effectiveness of their interventions immediately and make adjustments as needed. By providing instant feedback on stent deployment outcomes, these simulators accelerate the learning curve and help interventionists develop a keen eye for identifying and correcting suboptimal results.
Improving Procedural Efficiency Through Targeted Simulation Exercises
Customized Training Scenarios
Lesion simulation platforms can be programmed to create customized training scenarios tailored to individual learning needs. This targeted approach allows trainees to focus on specific areas of improvement, whether it's mastering complex bifurcation techniques or refining their approach to CTOs. By repeatedly practicing challenging scenarios, interventionists can build confidence and efficiency in their procedural skills, ultimately translating to improved performance in the catheterization laboratory.
Time-Pressure Simulations
To replicate the real-world pressures of the catheterization laboratory, some advanced neuro vascular simulator incorporate time-pressure elements into their training modules. These exercises challenge trainees to perform procedures efficiently while maintaining accuracy and safety. By practicing under simulated time constraints, interventionists can develop strategies to optimize their workflow and decision-making processes, leading to more streamlined and effective procedures in clinical practice.
Team-Based Training
Lesion simulation also offers opportunities for team-based training, allowing entire catheterization laboratory teams to practice together in a risk-free environment. This collaborative approach helps improve communication, coordination, and overall procedural efficiency. By simulating various scenarios, from routine cases to complex emergencies, teams can develop a shared understanding of roles and responsibilities, leading to smoother and more effective real-world procedures.
Conclusion
Simulating coronary artery lesions with neuro vascular simulators has revolutionized PCI training, offering unparalleled opportunities for skill development and procedural refinement. By providing realistic, diverse, and challenging scenarios, these advanced simulators enable interventional cardiologists to enhance their decision-making abilities, perfect their technical skills, and improve overall procedural efficiency. As simulation technologies continue to evolve, they will undoubtedly play an increasingly vital role in shaping the future of cardiovascular care, ensuring that patients receive the highest quality interventions possible.
Contact Us
For cutting-edge medical simulation solutions that can transform your PCI training program, look no further than Trandomed. Our state-of-the-art 3D printed silicone medical simulators offer unparalleled realism and versatility, helping healthcare professionals achieve better training outcomes. To learn more about how our innovative products can enhance your interventional cardiology training, contact us at jackson.chen@trandomed.com.
_1736215128474.webp)
 (SJ001D)_1734504338727.webp)
_1734507815464.webp)